-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1755-1759
doi:10.5923/j.ajmms.20231311.35
Received: Sep. 26, 2023; Accepted: Oct. 20, 2023; Published: Nov. 21, 2023

12-Year Dynamics for Acromegaly Morbidity in the Regions of the Republic of Uzbekistan According to the Register
Adliya Kholikova1, Zamira Khalimova2, Alisher Akbutaev3
1Department of Neuroendocrinology, Y.Kh. Turakulov Endocrinology Center, Tashkent, Uzbekistan
2Scientific Department of Neuroenocrinology and Pituitary Surgery, Y.Kh. Turakulov Endocrinology Center, Tashkent, Uzbekistan
3Department of Neurosurgery, Y.Kh. Turakulov Endocrinology Center, Tashkent, Uzbekistan
Correspondence to: Alisher Akbutaev, Department of Neurosurgery, Y.Kh. Turakulov Endocrinology Center, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Numerous investigations from various global regions and in nations with different healthcare systems revealed that the prevalence of acromegaly ranged from 0.2 to 13.7 instances per 100,000 people. Disease diagnosis is still frequently seen as having been delayed. Men are verified to have the condition in their fifth decade of life, while women are diagnosed between the ages of 38 and 56. Of the 526 patients that had been registered by January 1, 2019, 195 (37.07%) were men and 331 (62.93%) were women. Comparative investigation has revealed that between 2007 and 2019, the prevalence of acromegaly rose nationally. While acromegaly diagnosis declined over time in Djizzak and Samarkand, it improved in Tashkent city, Navoiy, and the Tashkent area. Over a 12-year period, the prevalence of acromegaly increased steadily nationwide. This statewide study can be used to inform local planning for initiatives aimed at raising the standard of care for acromegalic patients and lowering mortality and disease-related comorbidities.
Keywords: Acromegaly, Prevalence of acromegaly, Acromegaly morbidity
Cite this paper: Adliya Kholikova, Zamira Khalimova, Alisher Akbutaev, 12-Year Dynamics for Acromegaly Morbidity in the Regions of the Republic of Uzbekistan According to the Register, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1755-1759. doi: 10.5923/j.ajmms.20231311.35.
Article Outline
1. Introduction
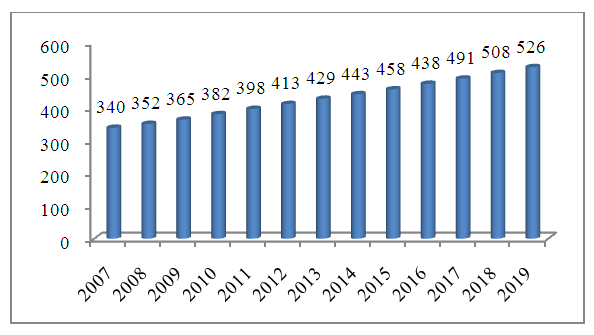
- Several studies, from different geographical areas worldwide, in countries with unalike healthcare systems, showed acromegaly prevalence from 2.8 to 13.7 cases per 100,000 population [14,17]. Agustsson TT et al [3] and Aagaard C et al [13] reported of 13.3–13.7 cases of acromegaly per 100,000. Regions with high prevalence of acromegaly include Iceland and Malta showing >13 cases per 100,000 individuals [7,10]. Studies in South Korea and Sweden discovered prevalence rate between 2.8 and 3.3 cases per 100,000 [16,24].Diagnosis of disease, to the date, considered significantly delayed in many cases. The presence of the disease is confirmed on the 5th decade of life in men (36.5–48.5 years-old), while women diagnosed between 38 and 56 years-old [7,13,16,21,24]. A period from disease manifestation to diagnosis varies across the studies from 3 to 25 years (average 4.5–5 years) [7,22,24]. These contribute to high macroadenomas frequency at diagnosis, which may result in less radical outcome of surgical treatment [3,4,6,7,13,21,24]. Current estimates of uncontrolled disease suggest decreasing life expectancy [5,19]. Number of studies showed increased mortality rate in patients with acromegaly by 2–3 times comparing with control group of the same age and sex [19]. Mostly, death caused by cardio-vascular and respiratory complications, and malignant disease [5,19]. Two meta-analyses showed inverse dependence between disease control and mortality rate – the better control, the lower mortality rate [8,11]. Additionally, remission of the disease, decrease of growth hormone levels, normalization of IGF-1 concentrations and somatostatin analogues administration contribute to lower mortality rates [11]. Decreased mortality rate with control improvement to population levels in acromegaly, except after radiation therapy, demonstrated across studies [8]. Sherlock M et al found that after radiation therapy the mortality rate of patients with acromegaly doubled compared to general population [23].In recent years, a number of studies have shown significance of nationwide or regional registries for acromegaly reflecting their effectiveness in better diagnosis, follow-up and treatment [19]. Uzbek nationwide registry for acromegaly was developed in 2007 and included patients from 1971 to 2007. Registry was designed for single examination with no option to follow patients. Thus, we developed new database with updated profiles to cover and survey acromegaly and its complications. The aims of this study were to assess comparative analysis of morbidity with acromegaly for 12-year period.
2. Materials and Research Methods
- Five hundred twenty six patients with GH-producing adenoma contributed to Uzbek acromegaly registry. All patients have been examined and registered from 1971 to 2019 i.e. forty eight-year period.All patients underwent examinations including radioimmune tests for LH, FSH, Prolactin, TSH, GH, IGF-1, IGFBP-3, Cortisole, Testosterone, Estradiol, free T4, computed or/and magnetic tomography of sellar region, ultrasound of thyroid and internal organs, ophthalmologic exam. To classify complications, we divided patients into three groups: with cardiovascular events, metabolic deviations, respiratory, bone-skeletal problems and neoplasms.
3. Results
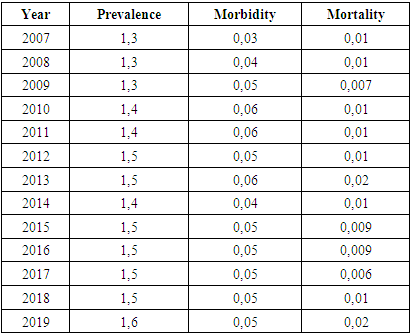
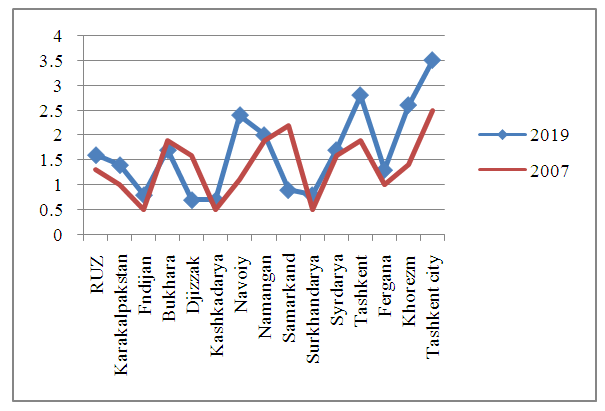
- Of 526 patients included in registry by 01/01/2019, 195 were males (37.07%) and 331 females (62.93%). Figure 1 demonstrates a growth of cases with acromegaly across Uzbekistan.
 | Figure 1. 12-year growth of acromegaly cases nationwide in the Republic of Uzbekistan |
|
|
 | Figure 2. Comparative evaluation of acromegaly prevalence across the regions |
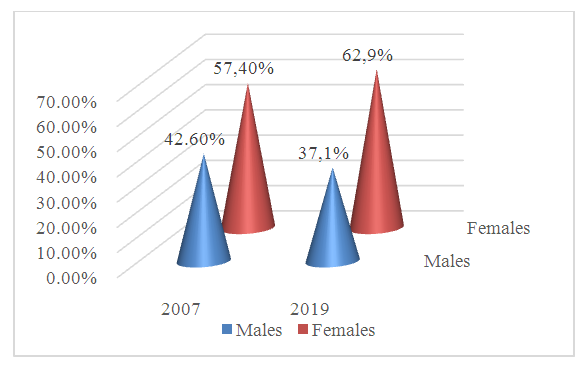 | Figure 3. Sex-associated relationship of acromegaly prevalence |
|
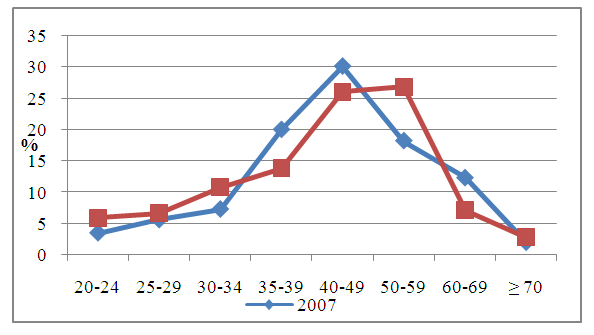 | Figure 4. Age-related cases of acromegaly for 12-year period |
4. Discussion
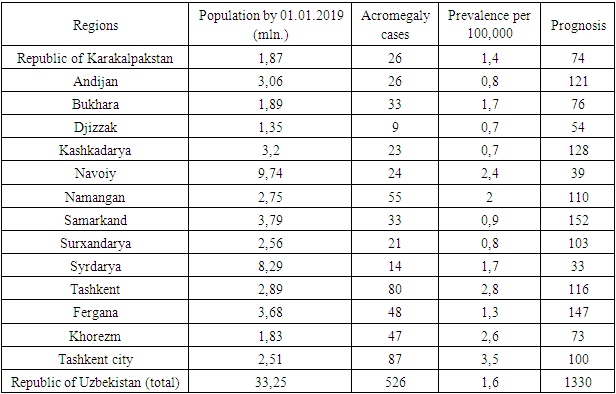
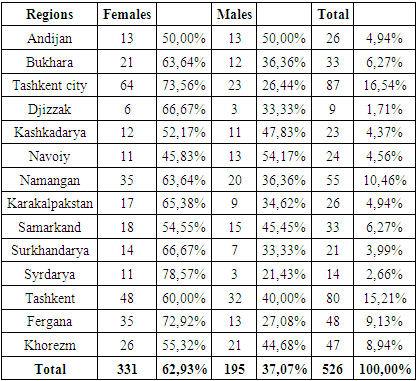
- Acromegaly is debilitating neuroendocrine condition causing multiorganic affection that leads to high disability and mortality rates. There are variety of literature data regarding the prevalence of acromegaly [3,7,9,17,24]. Our results suggest that prevalence of acromegaly by 2019 constituted 1.6 per 100,000 with significant fluctuations across the country (between 0.7 in Djizzak and Kashkadarya to 3.7 per 100,000 in Tashkent city). Equivalent prevalence rate estimates with other countries observed in Tashkent city (3.7) and Tashkent (2.8), Khorezm (2.6), Navoiy (2.4) regions. Lack of early diagnosis is the one of the essential reasons for low prevalence in Djizzak (0.7), Kashkadarya (0.7), Andijan (0.8) and Surkhandarya (0.8) regions. Compared to recent epidemiologic studies, our data correlates with international estimates (between 2.8 to 13.7 cases per 100,000) [3,7,13,22,24]. Tjornstrand et al showed 3.3 per 100,000 in Sweden [24], as well as Mestron et al demonstrated 3.4 per 100,000 prevalence of acromegaly in Spain.Epidemiological studies for acromegaly in relation with sex of the patients vary in data numbers [9,17,18,20]. According to Fernandez et al [115], Daly et al [96] and Agustsson et al [28] morbidity with acromegaly more often seen in males, while Gruppetta et al [9] and Kwon et al [16] reported higher numbers in female patients. Moreover, there are studies, which found no sex-specific differences in prevalence and morbidity of acromegaly [4,24]. In our study, we found that acromegaly morbidity is more common in female patients and for twelve-year period female/male ration showed growth from 1:1.3 to 1:1.7.It is acknowledged that morbidity rate among patients with acromegaly is higher than in general population [8,11]. In 2018 6 patients died, of which cardio-vascular events contributed to 59.5%, and morbidity rate constituted 0.02 ppm. Morbidity rate in our work remains on low level comparing to the world statistics, where this feature as twice as high the general population, which confirms that patients with acromegaly need better surveillance to follow main causes of mortality.
5. Conclusions
- Acromegaly prevalence growth showed progressive growth across the country through 12-year period. This nationwide research can be applied to the local planning of actions with the objective of improving the quality of care for acromegalic patients and reducing the mortality rates and complications associated with disease.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML