-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1748-1754
doi:10.5923/j.ajmms.20231311.34
Received: Nov. 9, 2023; Accepted: Nov. 20, 2023; Published: Nov. 21, 2023

Improvement of Tactical and Technical Aspects of Surgical Correction of Blepharoptosis
Ismailov S. I., Rasulov Zh. D., Akhmedov Sh. S.
State Institution "Republican Specialized Scientific and Practical Medical Center for Surgery named after Academician V. Vakhidov"
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Consideration of the severity of biomechanical disturbances of vector forces in ptosis of the upper eyelid of various etiologies made it possible to optimize the method of correcting this pathology. A method has been developed to relax the tarsal plate before correcting ptosis of the upper eyelids. Determining the function according to Berke allows you to choose which muscle the tarsal plate should be attached to. In case of satisfactory, good and excellent function of the levator of the eyelid, fixation is carried out to the levator of the eyelid and in case of unsatisfactory function - to the frontal muscle. The proposed technique for reducing tarsal plate resistance is effective and provides good aesthetic and functional results. The method is low-traumatic, simple to perform and low-cost. Its effectiveness is high both in acquired ptosis and in congenital ptosis with resulting satisfactory and good function of the levator eyelid.
Keywords: Blepharoptosis, Surgical correction, Ophthalmopathology, Tarsal plate
Cite this paper: Ismailov S. I., Rasulov Zh. D., Akhmedov Sh. S., Improvement of Tactical and Technical Aspects of Surgical Correction of Blepharoptosis, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1748-1754. doi: 10.5923/j.ajmms.20231311.34.
1. Introduction
- Ptosis of the upper eyelid is one of the topical topics in medicine. Its relevance is primarily due to the frequency of its spread among ophthalmopathology. Thus, according to various authors, ptosis of the upper eyelid among ophthalmopathies was 15.6%, and the total prevalence of hereditary eye diseases among adults was 2.42, among children-8.63 per 10,000 people. The relevance of this disease is also due to the fact that ptosis of the upper eyelid leads to various complications (up to 44.35% of cases), widely described in the literature [1,2,3]. Especially problematic today is congenital ptosis of the upper eyelid, which eventually leads to disruption of the visual apparatus and to complications such as amblyopia, strabismus, binocular vision disorder - monofocus vision, astigmatism, sometimes not amenable to correction, hypermetropia, severe myopia. Overhanging the eyelids on the pupils reduces the field of view from above. Over time, with congenital ptosis of the eyelids, the posture changes, the spine is deformed. With acquired ptosis, patients cannot strain their eyesight for a long time, there is increased fatigue, headaches. This category of patients, in addition to physical changes, suffer psychologically due to aesthetic inferiority, avoid society. Unfortunately, the frequency of ptosis of the upper eyelid has recently increased due to an increase in adverse factors, both social and hereditary [3]. The urgency of this problem is added by the fact that today there is no well-developed system for providing assistance to this category of patients. This is due to the fact that today there is no medical examination of patients with blepharoptosis, the operations performed with ptosis of the upper eyelid are not always effective, very often lead to various (from 17 to 40%) complications [1,3]. The risk of postoperative complications increases with the severity of ptosis of the eyelid and a decrease in the function of the levator of the eyelid. Of the currently existing methods of surgical treatment of ptosis of the upper eyelid, operations with resection of the levator muscle of the eyelid and operations of hanging the eyelid to the eyebrow are the most widespread. However, these techniques are not without drawbacks and often give complications, such as recurrent ptosis, hypocorrection, lagophthalmos, suture granuloma (32.4%) [4]. Reoperations after surgical correction of blepharoptosis are 8.7-18%, on the Muller muscle-3% [4]. After surgery, the eyelid often loses its protective, closing function, which can lead to keratitis, conjunctivitis. Operations with resection of the levator of the eyelid are not always possible to use in children under the age of 15 [3].This leads to the fact that uncomplicated blepharoptosis turns into complicated forms before adolescence. Operations with the suspension of the eyelid to the frontal muscle are inherently ineffective due to the high percentage of relapses. All this is the subject of discussion among ophthalmologists and plastic surgeons. The situation is not the best at the level of regions and districts. After surgery, the eyelid often loses its protective, closing function, which can lead to keratitis, conjunctivitis. Operations with resection of the levator of the eyelid are not always possible to use in children under the age of 15 [3]. This leads to the fact that uncomplicated blepharoptosis turns into complicated forms before adolescence. Operations with the suspension of the eyelid to the frontal muscle are inherently ineffective due to the high percentage of relapses. All this is the subject of discussion among ophthalmologists and plastic surgeons.
2. Materials and Methods
- The study included 155 patients with ptosis of the eyelid of various etiologies who underwent surgical treatment in private clinics "Fartuna YUR" in Kuvasai, in the private clinic "Biotest medical" in Fergana, in the clinic "Meridian" in Fergana in the clinic "FOCUS" medico center in Andijan, in the clinic "Nurly khayet" Kokand. 155 patients (197) with congenital and acquired ptoses of varying severity were operated on. The main group included 113 patients (131 eyes) with ptosis of the eyelids of various etiologies (66.7%), who before the correction of the eyelid had relaxation of the tarsal plate according to the original developed technique. The comparison group included 42 (66 eyes) patients (33.3%).The age of the patients ranged from 4 to 70 years. There were 10 (15.2%) male patients in the comparison group, 32 (48.5%) female, 41 (31.3%) and 72 (55.5%) in the main group, respectively, while there were 65 (41.9%) patients under the age of 18.Taking into account the fact that patients with blepharoptosis of both eyelids and ptosis of both eyelids came to us, we believe that for greater objectivity it is necessary to take into account not the number of operated patients, but the number of operated eyes. A total of 197 eyes were operated on. Of these, 66 (33.6%) were operated on in the control group, and 131 (66.8%) were operated on in the main group.In the main group, 43 (38.1%) patients were treated for congenital complicated blepharoptosis, 56 (49.6%) with congenital uncomplicated blepharoptosis, in the comparison group there were only 8 (19%) patients with congenital complicated blepharoptosis.Taking into account the wide spread of aesthetic blepharoplasty in the comparison group today, we decided to include patients with senile blepharoptosis with aesthetic blepharoplasty - 30 (71.4%) cases. In the main group, ocular myasthenia gravis occurred in 6 (5.3%) cases, 3 (2.7%) patients had neurogenic blepharoptosis, 3 (2.7%) with posttraumatic blepharoptosis, and 2 (1.8%) with gravitational ptosis. In the comparison group, neurogenic and posttraumatic ptosis were 2 (4.8%) cases each. Moreover, of all the patients, 23 (14.8%) had previously been corrected for ptosis of the eyelid, the rest were admitted initially. In all previously operated patients, the disease has recurred, which indicates a low level of medical care for patients with congenital blepharoptosis.The disease of both eyes was noted in 42 cases, in 24 (57.1%) in the comparison group and 18 (15.9%) in the main group, the right eye - in 49 cases, of which 13 (31%) in the comparison group and 36 (31.9%) in the main group, the left eye - in 64 cases, of which 5 (11.9%) in the comparison group and 59 (52.2%) in the main group.Preoperative examination does not require special equipment. The collection of complaints, anamnesis is carried out, it turns out whether they have been contacted about the disease and to which specialists, whether any operations have been performed, an oculist must be examined to identify intraocular pathology.The local status measures the width of the eye slit, levator function, corneal light reflex (MRD), the presence and height of the fold MCD). All these measurements are made using a ruler. Next, the Bell phenomenon is determined in order to identify the presence or absence of a blinking reflex, the mobility of the eyeballs and the mobility of the eyebrows are determined.According to the degree of ptosis of the eyelids, the patients were distributed as follows. In the comparison group, grade 1 ptosis was in 47 (71.2%) cases out of 66 eyes, 14 (21.2%) eyes were operated on with grade 2 ptosis, and 5 (7.6%) eyes were operated on with grade 3. In the main group, grade 1 ptosis was in 30 (22.9%) cases out of 131 eyes, 56 (42.7%) eyes were operated on with grade 2 ptosis, 45 (34.4%) eyes were operated on with grade 3 ptosis.All patients underwent general clinical methods of examination, anamnesis was collected, objective examination, laboratory methods of examination (general blood test, biochemical blood tests, coagulogram). The function of the levator of the century was determined by the Berke method. Patients with the function of the levator of the eyelid were divided into 4 groups: 1) with excellent eyelid levator function (above 12 mm); 2) with good levator function (8-12 mm); 3) with satisfactory levator function (5-7 mm); 4) with unsatisfactory levator function (0-4 mm).The examination of patients showed that the excellent function of the eyelid levator was only in 2 (3.0%) cases in the comparison group. Good function was noted in 43 (65.2%) eyes in the comparison group and 21 (16%) cases in the main group, satisfactory function was determined in 17 (25.8%) and 78 (59.5%) eyes, respectively, unsatisfactory was detected in 4 (6.1%) and 32 (24.4%) eyes.In the main group, operations were performed according to the proposed method of relaxation of the tarsal plate before correction of ptoses of the upper eyelids of various etiologies. When performing operations in the main group, the proposed methodology has the following main stages:• The operation is performed by transcutaneous access for adults mainly under local anesthesia, for children under 16 years of age under intravenous anesthesia in combination with local anesthesia with 1% lidocaine solution;• The skin is marked at a distance of 8-10 mm from the ciliary edge. The excised skin flap is drawn depending on the degree of stretching of the eyelid skin. In children and young people, this is a strip 2-3 mm wide;• After excision of the skin strip, the fibers of the circular muscle of the eye are separated. The septum of the eyelid intersects. The elevator of the century and the tarsal plate are exposed. Soft tissues are bluntly and sharply separated from the bottom down to the ciliary edge. The front surface of the tarsal plate is completely highlighted;• Projections of the edges of the irises of the eye are determined and marks are applied to the tarsal plate. At the level of the designated areas, the tarsal plate intersects across from the ciliary edge to the aponeurosis of the levator with a slight intersection of the lower edge of the aponeurosis (Fig. 1).
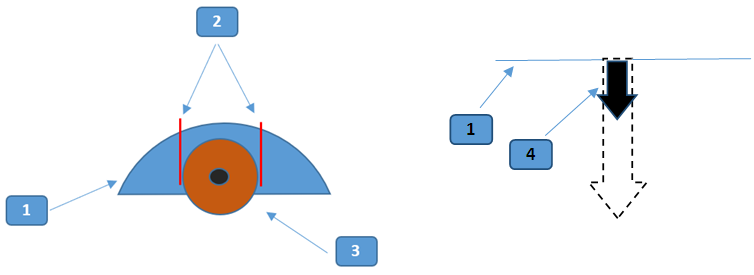 | 1. Tarsal plate. 2. Intersection sections. 3. The iris of the eye. 4. Tarsal plate resistance |
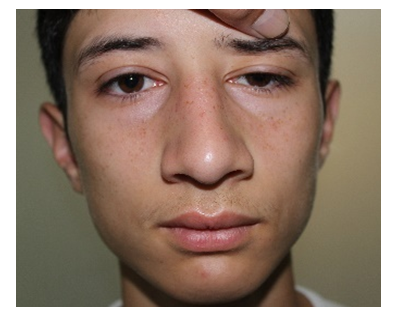 | Figure 2. Initial view |
 | Figure 3. Excision of the eyelid skin strip |
 | Figure 4. Separation of the fibers of the circular muscle of the eye and the exposure of the septum of the eyelid |
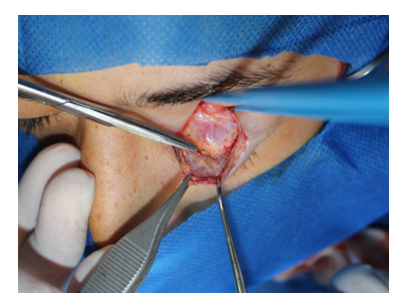 | Figure 5. Exposure of the levator of the century |
 | Figure 6. The stage of exposure of the tarsal plate to the ciliary edge marking along the lines of intersection of the tarsal plate |
 | Figure 7. The tarsal plate is crossed on the projections of the limb edges |
 | Figure 8. Application of U-shaped sutures between the levator of the eyelid and the central part of the tarsal plate |
 | Figure 9. Suturing the wound with the creation of a fold of the eyelid with nodular sutures |
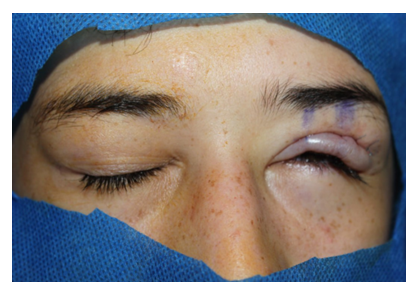 | Figure 10. Postoperative lagophthalmos check |
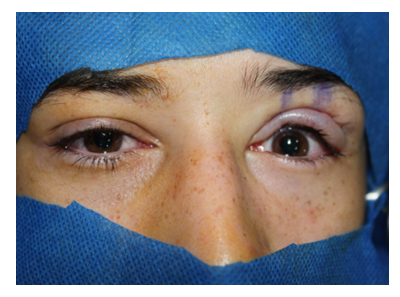
 | Figure 11. The view before and after the operation, the stages of the operation, closing of the eyelids a week after the operation |
3. Results and Discussion
- The proposed method of relaxation of the tarsal plate before correction of ptosis of the upper eyelids of various etiologies was developed taking into account the vector forces of the levator and was implemented after receiving a high frequency of unsatisfactory operations in the comparison group. For an objective comparative analysis, the results of operations are given from the number of operated eyes. Accordingly, 66 eyes were operated on in the comparison group, and 131 eyes were operated on in the main group.The analysis of postoperative complications showed that in the comparison group there were only 14 (21.2%) complications, whereas in the main group this indicator was only 3.8% (5 cases), which was significantly different (χ2=15,240; df=1; p<0.001).Among the complications, entropion development was noted in 3 (4.5%) cases in the comparison group and in 1 (0.8%) in the main group. Ulcerative keratitis developed in 5 (7.6%) and 2 (1.5%) cases, respectively, ligature fistula in 1 (1.5% and 0.8%) cases in both groups, pathological lagophthalmos in 4 (6.1%) patients in the comparison group.Complications such as keratitis, entropion and endophthalmitis developed up to 7 days after surgery. Further, ligature fistulas were verified after 2 months. In turn, if lagophthalmos was not resolved within 6 months after surgery, then it was treated as permanent, and in cases from 4 mm and above, lagophthalmos was regarded as pathological.Of the 5 cases with the development of ulcerative keratitis in the comparison group, in 4 (6.1%), the complication was resolved conservatively, forced suturing was performed in 1 (1.5%) observation. Despite conservative therapy, 1 patient with neurogenic blepharoptosis in the comparison group had to have stitches removed with artificial creation of blepharoptosis due to the threat of endophthalmitis and blindness. In the main group, 2 (1.5%) ulcerative keratitis were resolved conservatively.A complication in the form of a relapse of blepharoptosis is considered as the main cause of unsatisfactory correction results. In the comparison group, with the initial first degree of ptosis out of 47 operated eyes, relapse developed in 26 (55.3%) cases, with the second degree out of 14 in 9 (64.3%), with the third degree in all 5 cases. In the main group, with the initial first degree of ptosis out of 30 operated eyes, there was no recurrence (χ2=33,122; df=1; p<0.001 relative to the comparison group), with the second degree out of 56 in 2 (3.6%) cases (χ2=31,171; df=1; p<0.001), with the third degree out of 45 in 5 (11.1%) observations (χ2=22,222; df=1; p<0.001). In total, there were 40 (60.6% of 66 eyes) relapses of blepharoptosis in the comparison group, whereas in the main group there were only 7 (5.3% of 131 eyes) cases (χ2=89,199; df=1; p<0.001).In the comparison group, ptosis is not taken into account and is not corrected during surgery, and therefore relapses are possible immediately after surgery. During the resection of the levator of the eyelid, the cause of relapse was mainly a strong lateral tension, leading to the cutting of the seams within up to 3 months after correction. During suspension operations, the cause of relapse is also a strong lateral tension and cutting of seams both from the upper part of the connecting link with the frontal mouse and from the tarsal plate.In the main group, the causes of relapses at the stage of the introduction of the new technique were that the function of the eyelid levator was not taken into account and the tarsal plate was attached to the levator, even with its unsatisfactory function. Starting in 2021, in patients with unsatisfactory levator function or with complete absence of levator function, the tarsal plate was attached to the frontal muscle in the subcutaneous region, which significantly reduced the frequency of relapses. Accordingly, in the main group in 7 cases there was a lack of consideration of the levator function and then 2 methods with the frontal muscle were developed.Performing corrective operations may be accompanied by the development of temporary lagophthalmos, as a rule, it was resolved within 6 months after the operation. The width of the eye slit up to 3 mm is possible without harmful effects on the eyeball, which referred to the permissible lagophthalmos. Pathological lagophthalmos is a permanent lagophthalmos from 4 mm and above. In our observations in the comparison group, pathological lagophthalmos developed in 4 (6.1%) cases, the temporary form in 11 (16.7%), without this manifestation there were 51 (77.3%) operated eyes, however, it should be noted that in most cases in this group there were recurrences of ptosis. In the main group, pathological lagophthalmos was not noted (χ2=8,104; df=1; p=0.005 in relation to the comparison group), the temporary form was in 54 (41.2%) cases and in 77 (58.8%) cases of lagophthalmos was not noted. Permanent, but acceptable lagophthalmos was noted only in 1 case in the main group.A significant decrease in the proportion of patients without lagophthalmos is due to the fact that relaxation of the tarsal plate makes it possible to attach it lower, preserving a longer section of the levator muscle without resection with the creation of a conventional duplication. In the case of the frontal muscle, it should not be attached as high as possible, it is enough in the subcutaneous part. It is the sufficient length of the preserved muscle that ensures its extensibility and, accordingly, the closing of the eyelid does not suffer. In this connection, there were many patients with preserved levator function in the main group.In our observations from 11 eyes in the comparison group, temporary lagophthalmos regressed within 1 week after surgery in 2 (18.2%) cases, in 2 more cases after 2 weeks, in 3 (27.3%) by 4 weeks. At the same time, in 4 (36.4%) patients, lagophthalmos is regarded as permanent, but acceptable. In the main group of 54 operated eyes, lagophthalmos regressed within 1 week after surgery in 28 (51.9%) cases, in 23 (42.6%) cases after 2 weeks, in 2 (3.7%) by 4 weeks, in 1 patient (1.9%) 2 mm lagophthalmos was regarded as permanent, but acceptable (fig. 12).
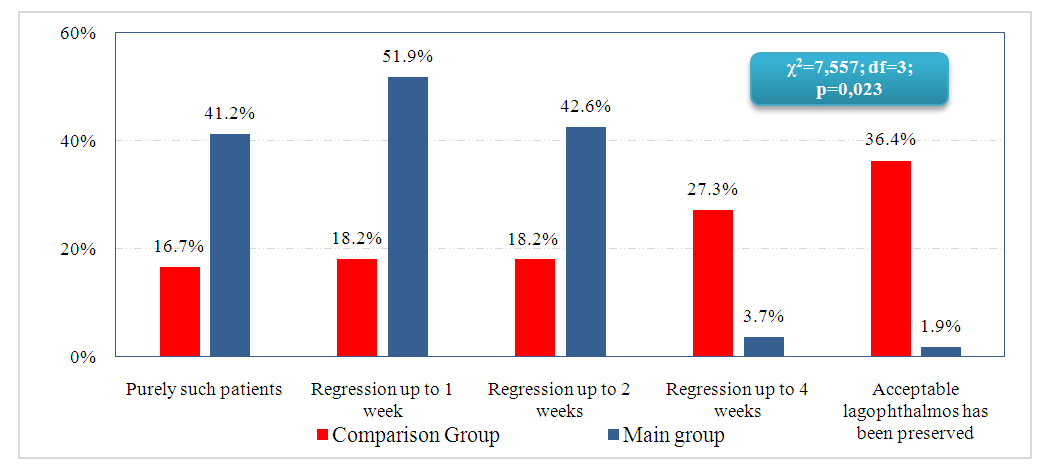 | Figure 12. Terms of regression of temporary lagophthalmos |
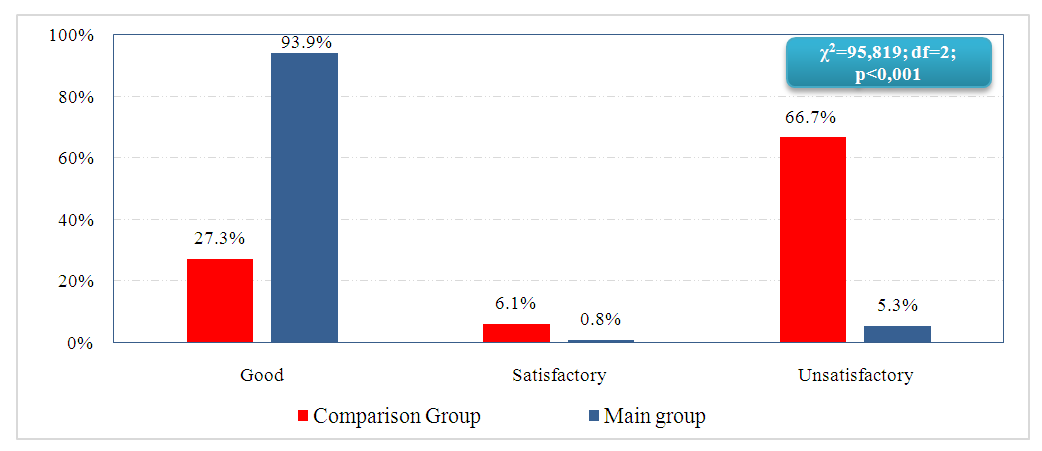 | Figure 13. Summary aesthetic results in comparison groups |
4. Conclusions
- Taking into account the severity of biomechanical violations of vector forces in upper eyelid ptosis of various etiologies allowed optimizing the methodology for correcting this pathology. A method of relaxation of the tarsal plate before correction of ptosis of the upper eyelids of various etiologies has been developed, including exposure of the tarsal plate and stitching of the tarsal plate to the eyelid levator, characterized in that the anterior surface of the tarsal plate is exposed, then two transverse parallel through-cuts of the tarsal plate are applied in projections of the edges of the limbs from the ciliary edge to the eyelid levator muscle with partial dissection of its aponeurosis to a depth of 1 to 2 mm, the stitching of the tarsal plate with the levator of the eyelid is performed by creating a duplicate of the tarsal plate with the levator of the eyelid or by suturing between the tarsal plate and the frontal muscle.The Berke function definition allows you to choose which muscle to attach the tarsal plate to. In case of satisfactory, good and excellent function of the eyelid levator, fixation is carried out to the eyelid levator, in case of unsatisfactory function to the frontal muscle.The proposed method of reducing the resistance of the tarsal plate is effective and provides good aesthetic and functional results. The method is low-traumatic, easy to perform and low-cost. Its effectiveness is high both in acquired postures and in congenital ptoses with satisfactory and good function of the eyelid levator.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML