-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1708-1710
doi:10.5923/j.ajmms.20231311.25
Received: Oct. 17, 2023; Accepted: Nov. 5, 2023; Published: Nov. 11, 2023

Transient Ischemic Attack in a Patient Presenting with Hypertension: Clinical Perspectives
Mulenga Chewe1, Miyanze Towela1, Muletambo Chisha1, Mweene Jenipher1, Gamal Maksoud1, Mwinsa Chimese2, Kennedy Gondwe3, Christopher Nyirenda1
1The Copperbelt University, School of Medicine, Department of Clinical Sciences, Ndola, Zambia
2Ndola Teaching Hospital, Department of Medicine, Ndola, Zambia
3The Copperbelt University, School of Medicine, Department of Clinical Sciences, Kitwe, Zambia
Correspondence to: Christopher Nyirenda, The Copperbelt University, School of Medicine, Department of Clinical Sciences, Ndola, Zambia.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Patient SM, F/29 years, a known HIV patient, referred from a local clinic of Ndola district presented with paralysis of the mouth, deviation of lips to the right, dysarthria for 1 day. She reported a positive family history of hypertension with no history of fainting, dizziness, blackout, fitting, irrelevant talking, weakness in the limbs, nor headaches. There was no history of body hotness, night sweats, or chills. She was stable and alert with a Glasgow coma scale of 15/15, temperature: 35.9°C, pulse rate: 103bpm, respiratory rate: 21/min, blood pressure: 153/107mmHg, lower left facial paralysis, intact facial sensation, regularly irregular heart sounds, and normal peripheral neurological assessment. The patient received inpatient care with anti-hypertensives and adjuvant therapy. Complete symptom resolution was marked by the third day post admission. The report highlights a typical clinical sequelae suggesting features of a transient ischemic attack despite symptoms resolving beyond 24 hours in care.
Keywords: Cerebral Vascular Accident, Transient Ischemic Attack, Facial Paralysis, Hypertension
Cite this paper: Mulenga Chewe, Miyanze Towela, Muletambo Chisha, Mweene Jenipher, Gamal Maksoud, Mwinsa Chimese, Kennedy Gondwe, Christopher Nyirenda, Transient Ischemic Attack in a Patient Presenting with Hypertension: Clinical Perspectives, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1708-1710. doi: 10.5923/j.ajmms.20231311.25.
Article Outline
1. Introduction
- Background of the diseaseA transient ischemic attack (TIA) is a syndrome of neurological deficit that is focal and generally resolves promptly due to disruption in the blood flow to the specific area of the brain. Typically and previously defined as focal neurological deficit that resolves within 24 hours [1]. More recent definitions however, de-emphasize on the time aspect and emphasize the tissue aspect, describing the pathology as ischemia, as opposed to a stroke which is also focal neurological deficit in which the pathology is infarction [2]. Symptomatology largely rests on the specific region of the brain parenchyma that is transiently starved of oxygen and glucose [3]. Diagnostic imaging modalities are the Magnetic Resonance Imaging (MRI) and the Computer Tomography (CT) scan [2]. Background of the patientPatient is SM, female aged 29 years. Resident of a township of Twapia township in Ndola urban district who was referred from a local clinic to a university teaching hospital in Ndola. She presented to the medical out-patient department for further evaluations and continuation of care.
2. Clinical Presentation
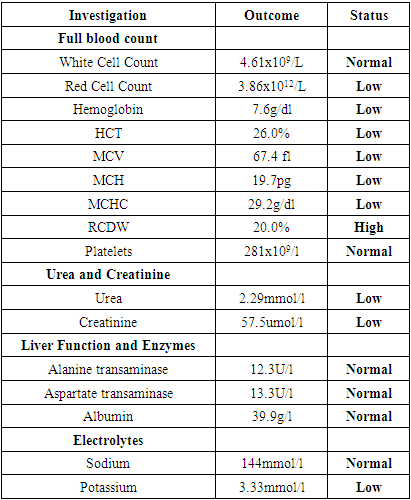
- HistoryPatient was well until 2 days prior to history taking when she developed pain on her throat associated with difficulties to swallow solids but not liquids. The pain was of sudden onset and not progressive. A day later, the pain on her throat resolved, however she noticed that her mouth and lips felt heavy. At the same time, her mother noticed that her mouth had deviated towards the right. She then started having difficulties talking, about 17 hours prior presentation. There was no history of fainting, dizziness, blackouts, fitting, irrelevant talking, weakness in the limbs and no headaches. She also reported no history of body hotness, night sweats, or chills. There was no report of easy fatigability, orthopnoea, paroxysmal nocturnal dyspnea, cough, chest pain, or dyspnea. She reported no abdominal pain, vomiting, anorexia, diarrhea hematuria, or dysuria. She further suggested, no family history of diabetes, asthma or sickle cell, but positive history of hypertension in mother and uncle from mothers’ side. Patient is a known HIV patient on anti-retroviral therapy (ART) for 2 years, with no known history of tuberculosis, sickle cell disease, diabetes mellitus, asthma or hypertension. There was no known food or drug allergy. She lived in a township, was not married, and had 1 child that demised. She reported no smoking or alcohol intake.Physical ExaminationShe was stable and alert, GCS 15/15, temperature: 35.9°C, pulse rate: 103bpm, respiratory rate: 21/min, blood pressure: 153/107mmHg. Repeat BP was done 6 hours later: 170/108mmHg.The mouth was deviated towards the right and was most prominent when she opened her mouth, and had slurred speech. She was unable to blow her cheeks and protract her tongue. The oral cavity was clear, oral pharynx was not erythematous. Sensation on her face both fine and crude, was intact. She was failing to clench her teeth however, she was able to raise her eyebrows symmetrically and Bells Phenomenon was absent. Cranial nerves I-IV, VI, VIII-XII were intact.The apex beat was in the 5th interspace midclavicular line. Percussion note was resonant, vesicular breath sounds heard bilaterally with no rales, S1S2 heard regularly irregular rhythm. She had no obvious abdominal distension. Her abdomen was soft and non-tender and no organs palpated. Neurological assessment revealed normal muscle bulk in all the limbs, no fasciculations, normal tone, power of 5/5 in all the limbs, normal reflexes (Grade 2). Her coordination was intact. Both crude and fine touch were intact and her proprioception was normal.Diagnostic Focus and AssessmentAt presentation, a number of differential diagnoses were considered, as guided by the history taking and the subsequent clinical examination. The presentation including history of dysphagia, dysarthria and facial paralysis, with an elevated blood pressure was a strong case for stroke. However, syndromes of facial paralysis such as Bell’s palsy and Ramsay-Hunt syndrome couldn’t simply be ruled out from the history. On examination, it was noted that the paralysis only affected the lower half of the face. This is because she was able to raise both eyebrows, and Bells phenomenon was absent. Thus an upper rather than a lower motor neuron lesion was concluded, effectively ruling out Bell’s palsy and Ramsay-Hunt syndrome. She had presented with elevated blood pressure with no prior history of hypertension. However, there was positive family history of hypertension from the mothers’ side. Two blood pressure readings were taken that were 6 hours apart and both were elevated. A diagnosis of hypertension was considered, in this index presentation with neurological deficit. She was admitted for in-patient assessment and care.Baseline blood workups were ordered. These included; a full blood count, serum urea, creatinine and electrolyte levels, liver enzymes and lipid profile. A CT scan of the head was ordered as a diagnostic investigation for the neurological deficit but patient did not have the finances to meet the cost involved. Detail of the results for the lab works are as reflected in table 1. The patient was Commenced on hydrochlorothiazide 55mg, enalapril 5mg and simvastatin 20mg and hematinics. A BP profile was also ordered.
|
3. Discussion
- The patient was managed as a case of transient ischemic attack (TIA) in a newly diagnosed hypertensive. This was an index presentation. Patient had presented with dysarthria and lower facial paralysis. At the time of referral the symptomatology had been there for about 17hours. Her blood pressure was elevated for over 6 hours under observation, warranting a diagnosis of hypertension. The confirmation of the neurological lesion towards the diagnosis especially required imaging which could not be conducted due to lack of finances on the part of the patient, ultimately rendering the diagnosis more clinical. Another aspect worth noting is the onset of the hypertension. Primary hypertension is seen mostly in the elderly, because by the age of 80, up to 90% of individuals will be hypertensive [4]. The patients’ renal function was within normal while possible hormonal imbalances contributing to the hypertension were not clinically suggested. However, there was a family history of hypertension, as a plausible a risk factor. Neurological pathology generally possess a diagnostic challenge. This rests largely on the modalities of diagnosis that are mainly radiological. In the case of our patient, there was no back up CT scan report. Another aspect of note is the failure of definitions in the presentation and progression of symptoms for the patient. Clearly the patients’ presentation didn’t meet the previous definition of a transient ischemic attack based on the timing since the symptoms had persisted beyond 24 hours. The 2 definitions commonly used are; one based on time in which the symptom resolution should be within 24 hours, and the other considered the revised version being based on the appearance of tissue with no infarction on magnetic resonance imaging [5]. Further, the patients’ condition didn’t satisfy the definition of a stroke because the patient later on fully recovered.
4. Conclusions
- The report presents a sequelae clinically consistent with a TIA despite the resolution of symptoms being beyond 24 hours. The failure to confirm the status as TIA with back up imaging such as MRI or CT scan per the requirement in the revised criteria, highlights typical challenges in care towards the management of patients presenting with vascular and neurological deficits in the face of resource limitations.
5. Patient’s Perspective
- The condition was worrisome to the patient, especially the fact that her BP was elevated. The situation was more disheartening to her when the costs of some of the diagnostic modalities were suggested. However, when the condition improved, she was very hopeful and optimistic.
Consent
- Informed Consent for assessment, write-up and publication was obtained from the patient.Conflict of Interest: The authors declare that there was no conflict of interest regarding the publication of the manuscript.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML