-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1689-1692
doi:10.5923/j.ajmms.20231311.21
Received: Sep. 16, 2023; Accepted: Oct. 23, 2023; Published: Nov. 11, 2023

Dynamics of Transferrin at Different Periods of Pregnancy
Azimova Sevara Bahodirovna1, Mamadiyarova Dilshoda Umirzokovna2, Mamadiyarova Dilfuza Umirzakovna3
1Associate Professor of the Department of Normal and Pathological Physiology of the Tashkent Medical Academy, Doctor of Medical Sciences, Uzbekistan
2Assistant and Independent Researcher of Samarkand State Medical University, Faculty of Medicine, Department of Physiology, Samarkand City, Uzbekistan
3Associate Professor of the Department of Pedagogy and Psychology of Samarkand State Medical University, Doctor of Philosophy in Psychology, Uzbekistan
Correspondence to: Mamadiyarova Dilfuza Umirzakovna, Associate Professor of the Department of Pedagogy and Psychology of Samarkand State Medical University, Doctor of Philosophy in Psychology, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

60 pregnant rabbits were examined in order to determine the main indicators of iron metabolism in the peripheral blood of pregnant rabbits, the dynamics and characteristics of iron metabolism at different periods of pregnancy. In different periods of pregnancy, the amount of iron in the peripheral blood of rabbits fed with iron and zinc supplements under different nutritional conditions and the factors affecting its metabolism has a unique dynamic and physiological character depending on the type of food, the duration of pregnancy and the stages of fetal development. has been shown to have.
Keywords: Pregnancy, Iron, Transferrin, Dynamics, Amount, Term
Cite this paper: Azimova Sevara Bahodirovna, Mamadiyarova Dilshoda Umirzokovna, Mamadiyarova Dilfuza Umirzakovna, Dynamics of Transferrin at Different Periods of Pregnancy, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1689-1692. doi: 10.5923/j.ajmms.20231311.21.
Article Outline
1. Relevance of the Topic
- According to WHO data, 2 billion people (more than 30% of the population) suffer from iron deficiency anemia. Iron deficiency is a leading problem among women of reproductive age, pregnant women and children of various ages. According to the conducted studies, 74.7% of mothers of babies who died in the first week of life, and 43.5% of mothers of babies who died in the first month of life had iron deficiency. Today, all cases of iron deficiency are divided into pre-latent, latent and iron deficiency. Latent, hidden and iron deficiency is caused by a decrease in the transport of stored iron through erythrocytes. Biochemical and clinical signs are not observed. By the end of the last trimester of pregnancy, latent iron deficiency is detected. This is characterized by a decrease in the amount of iron in the reserve.
2. Materials and Methods
- Peripheral blood of 60 pregnant rabbits fed with different diets was examined. 15 of them were fed with normal feed, 15 were fed with iron supplement, 15 were fed with zinc supplement, and 15 were fed with insufficient feed. Based on the goals and tasks of the research, the factors involved in the metabolism of iron in the peripheral blood of pregnant rabbits at different periods (7-14-21-28 days) were studied. For these analyses, blood samples were taken from the ear vein of rabbits. The obtained blood samples were taken into special test tubes and hematological, biochemical, IFA and IXLA analysis was performed. Blood samples taken from the control and experimental groups were developed in laboratory conditions based on Mindray's most advanced hematological diagnostic technology BC-5000 - hematology analyzer (general blood analysis), biochemical analyzer for testing Fe and iron-storing proteins in blood serum - User Manual XL- 200 were used. Developed on the basis of Mindray's most advanced hematological diagnostic technology, the BC-5000 hematology analyzer is the lightest, most compact and convenient in appearance, and is designed for hematological analyzes and calculation of 5 populations of leukocytes in laboratory conditions. 23 whole blood parameters, 3 histograms and 3 different scatter diagrams can be obtained with this device.Three-vector laser scattering, flow focusing, and chemical staining allow better differentiation of leukocytes in 5 populations, even in highly eosinophil samples. 5 ml of venous blood is taken for analysis.User Manual XL-200 analyzer is a compact desktop biochemical analyzer capable of performing urgent biochemical analyses. The device has a very high productivity - it can detect 200 photometric tests or 360 ion-selective tests per hour.Through hemolytic and biochemical analyses, the indicators of Fe and iron-storing compounds in the blood were determined every 7 days of pregnancy, and the characteristics and dynamics of iron metabolism were monitored.In addition to the above indicators, hypoxia induced by the immunoassay method (Elisa) in Cloud-Clone (Cloud-Clone corp., USA) blood serum with mr 96 microplate photometer (Mindray, China) at 450 nm wavelength measurements The concentration of the inflammatory factor (HIF-1α, ng/ml) was determined (see Table 2.3). For this purpose, 1 ml of blood is taken, centrifuged at 3000 rpm for 15 minutes and the serum is separated, then the serum is placed in the IFA apparatus.Transferrin belongs to β globulin in the blood serum and plays an important role in transporting iron from the intestines to the reserve. The synthesis of this protein takes place in the liver depending on the amount of iron in the body: as the amount of iron decreases, its synthesis increases. One transferrin molecule can bind 2 iron atoms. In hidden iron deficiency in the body, the iron saturation level of transferrin decreases. Ferritin plays an important role in the transfer of iron in the intestine and placenta. It is a mediator that connects iron with transferrin and transfers it from the mother to the fetus. The functional purpose of reserve iron is to maintain the iron concentration in the blood serum at a constant level. When necessary, iron from the reserve is released in the form of ferritin, binds with transferrin and is directed to the bone marrow. During the first trimester of pregnancy, iron deficiency anemia can be determined by the amount of ferritin in the plasma [1,2].
3. The Purpose of the Study
- Determining the characteristics of dynamic parameters of iron metabolism in different periods of pregnancy related to different nutrients and periods of pregnancy.
4. Research Results and Discussion
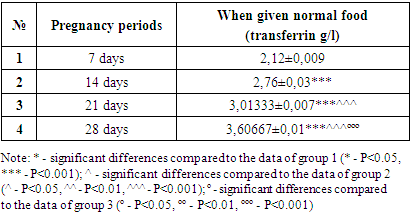
- In the group fed with normal feed, 15 white Khikol rabbits were determined on the 7-14-21-28 days of pregnancy of transferrin levels in the peripheral blood. (Table 1).
|
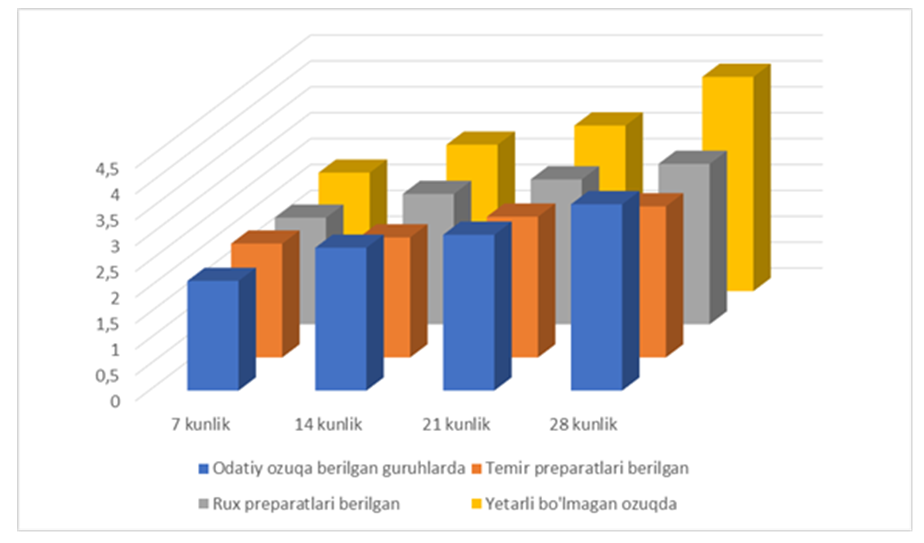 | Figure 1. Dynamics of the amount of transferrin in groups fed with different feeds |
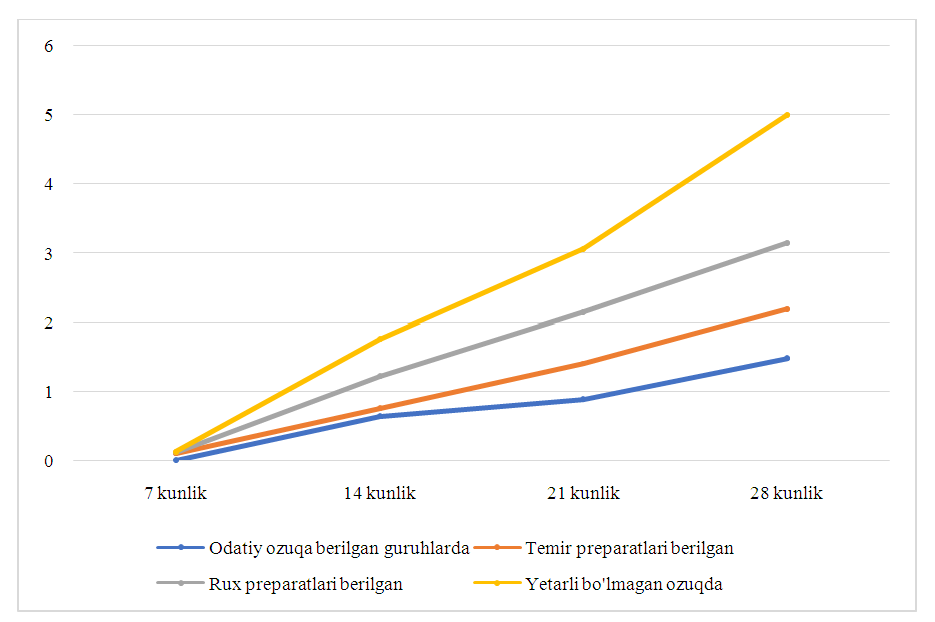 | Figure 2. Dynamics of transferrin content in peripheral blood at different periods of pregnancy in groups fed different diets |
5. Conclusions
- Thus, in the initial period (7 days) of pregnancy, the amount of transferrin increases in the groups fed with iron supplements, while in the groups fed with zinc, it decreases compared to the group given the usual feed, and in the group given insufficient feed, its amount increases. During the remaining periods of pregnancy, an increase in the amount of transferrin is observed in all group observations. As the duration of pregnancy increases, the amount of transferrin increases in all observation groups.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML