-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1666-1668
doi:10.5923/j.ajmms.20231311.16
Received: Oct. 11, 2023; Accepted: Nov. 2, 2023; Published: Nov. 8, 2023

Ovarian Hypertecosis in an Infertile Marriage
Shokirova S. M.1, Israilov R. I.2
1Andijan State Medical Institute, Andijan, Uzbekistan
2Republican Center of Pathological Anatomy, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In this work, the pathomorphological characteristics of a part of the ovary in ovarian infertility were studied. The material of the study was the surgically removed parts of the ovary during surgery for infertility. In ovarian infertility, the tunica albuginea of the ovary was subjected to an inflammatory-sclerotic process and there are many primordial follicles in the corvous layer. In all layers, a plurality of epithelial theca cells has been identified.
Keywords: Ovary, Hyperthecosis, Pregnancy, Infertility, Theca cells
Cite this paper: Shokirova S. M., Israilov R. I., Ovarian Hypertecosis in an Infertile Marriage, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1666-1668. doi: 10.5923/j.ajmms.20231311.16.
Article Outline
1. Introduction
- Infertility, according to various authors [1,2], occurs in 15-20% of cases and its prevalence is constantly increasing. Infertile marriage structure accounts for 50-60% of women's infertility, and 35-75% of cases are caused by ovarian changes [3,4]. Today, a number of candidate genes related to the development of this disease have been found in ovarian connective tissue, adipose tissue, follicular fluid, and T-lymphocytes. In 2009, Z.A. Mohamed-Husseini H. Sarahani studied 1081 genes, 1066 known and 15 unknown proteins, related to the TPS sympathocomplex [5].According to the authors, 468 genes are associated with 339 proteins in TPS, of which 34 are transcription factors, 37 are recognition proteins, 35 are protein dimers, 50 are protein receptors, 13 are cyclins, 24 are enzymes, 13 -one was growth factor and 3 were follistatins. According to the studies of the authors, the expression of a large number of genes was observed during the development of polycystic ovary, and the changes of cells with gene information were determined during the progression of the disease [6]. Genetic aspects of TPS have been found to be not only maternal and sib-specific, but also male-specific, such as rapid male pattern baldness, hormone deficiency, and insulin resistance [7].
2. Test Material and Methods
- As material, 48 cases of biopsy of women treated for infertility and surgical removal of the ovaries were taken, which were examined in the biopsy department of the Republican Center for Pathological Anatomy and in the private laboratory of IPSUM. Ovary slices were frozen in 10% neutralized formalin solution for 48 hours, then washed in running water for 3-4 hours. Dehydration was carried out in increasing concentrations of alcohols and chloroform, followed by embedding in paraffin with wax, and sections were prepared. Histological sections with a thickness of 5-6 mkm were prepared from paraffin blocks and stained by hematoxylin-eosin and van Gieson methods. Preparations were studied in 10, 20, 40 lenses of a light microscope, and necessary areas were photographed.
3. Examination Results and Analysis
- Macroscopically, the ovary is of normal size, the surface is smooth or uneven, nodular due to cystic follicles, light gray. In the section, the white membrane is thickened, under it there are cysts of different sizes, the bark layer is sharply expanded and has a discharge color. Histologically, there are many primordial follicles in the cortical layer and few developing follicles. No corpus luteum is found. As a result of the growth of stromal theca tissue, it is determined that the ovary is enlarged or nodules have appeared. Epithelioid theca cells are scattered or multiply around blood vessels. Theca cells are round-polygonal in shape, the cytoplasm is foamy vacuolated, the nucleus is large, functionally active cells. Since these indicated pathomorphological changes are not characteristic of any other disease, this disease can be considered as a separate nosological form.The results of the microscopic examination showed that almost all layers of the ovary were covered by growth of theca tissue. Proliferated theca tissue cells are similar to internal theca cells in their histological structure. They are relatively sparsely located, the cytoplasm is light-colored, the nuclei are round and oval in shape, and most of them are relatively enlarged and resemble epithelioid cells (Fig. 1). Theca tissue tufts are randomly arranged, dense and large tufts in some places, and sparse tufts have appeared in other areas, especially around blood vessels. formed. These cells consist of bundles of different levels, and it is determined that they are located around the blood vessels in the form of separate circular bundles (Fig. 2). Their nuclei are mostly hyperchromic, and darkly stained nuclei are observed among them. The growing theca tissue first occupies the cortical layer, then it spreads towards the white membrane and the medulla. In fact, the white membrane consists of a thin unformed connective tissue, instead of which the theca tissue grows and completely occupies the private plate located on the outer surface of the ovary, and instead of it, a thin membrane of cells similar to epithelioid cells with a relatively hyperchromic, elongated nucleus appears (Fig. 3).
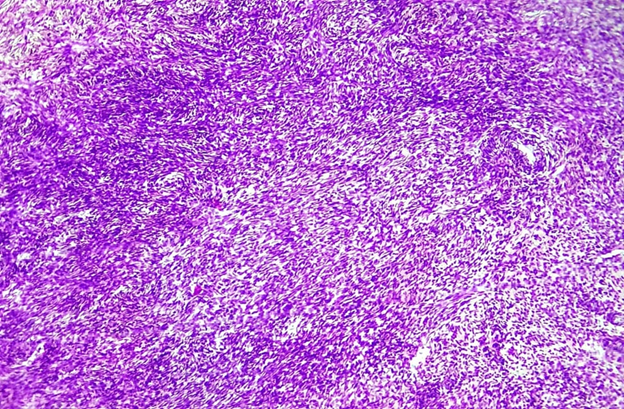 | Figure 1. A 29-year-old female P ovary. Growth of theca tissue in all layers. Paint: G-E. Floor: 10x10 |
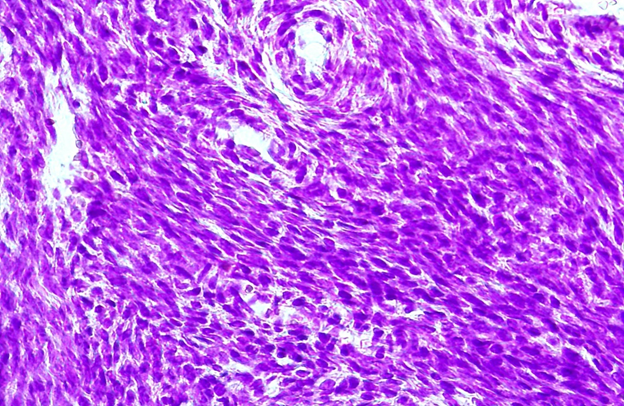 | Figure 2. P ovary of a 29-year-old woman. Theca cells resemble epithelioid cells in that their nuclei are enlarged. Paint: G-E. Floor: 10x40 |
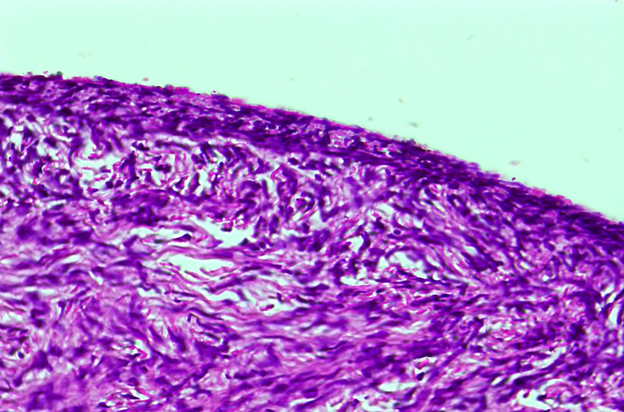 | Figure 3. A 28-year-old female named V. Theca tissue has also taken over the white veil, forming a thin and dense veil of theca tissue on the outer surface. Paint: G-E. Floor: 10x40 |
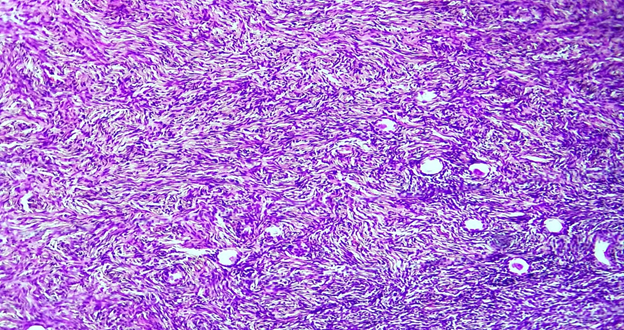 | Figure 4. A 26-year-old woman named B has an ovary. Diffuse proliferation of epithelioid-shaped theca cells, transformation of primary follicles into a cystic cavity. Paint: G-E. Floor: 10x10. |
4. Conclusions
- Hyperthecosis is a rare disease, which often begins as a result of extragenital diseases, endocrine pathologies and leads to primary infertility. Pathogenesis is the proliferation of epithelioid theca cells instead of theca cells due to the activation of sex hormones. Secretory activity of theca cells leads to an increase in the amount of androgens, virilization of the body. In 1942, S. Geist and J. Geines were the first to show, as a result of histological examination of the ovary, that the luteinized theca cells increased, similar in structure to internal theca cells, and multiplied independently of follicles. Currently, because the name of this process is not given clearly, it is called unihypertecosis, cortical stromal hyperplasia, stromal proliferation, stromal thekosis thekamatosis. Histologically, the cortex contains many primordial follicles, few developing follicles, and no corpus luteum. As a result of the growth of stromal theca tissue, it is determined that the ovary is enlarged or nodules have appeared. Epithelioid theca cells are scattered or multiply around blood vessels. Theca cells are round-polygonal in shape, the cytoplasm is foamy vacuolated, the nucleus is large, functionally active cells. Since these indicated pathomorphological changes are not characteristic of any other disease, this disease can be considered as a separate nosological form.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML