-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1651-1656
doi:10.5923/j.ajmms.20231311.12
Received: Oct. 13, 2023; Accepted: Nov. 5, 2023; Published: Nov. 7, 2023

The Correlation Between Indicators of Time Intervals of Left Ventricular Activity and Markers of Myocardial Damage and Coronary Artery Atherosclerosis in Patients without-ST-Segment Elevation Acute Coronary Syndrome (NSTE-ACS)
Bekmetova F. M., Yuldoshev N. A., Fozilov Kh. G., Bekbulatova R. Sh., Abdullaeva S. Ya., Koshimov Sh. U., Doniyorov Sh. N., Karimov B. S., Ilkhomova L. T., Khotamova M. N., Arslonov S. F.
Republican Specialized Scientific-Practical Medical Center of Cardiology, Tashkent with a Branch of the City of Karshi, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The study investigated the correlation between indicators of time intervals of left ventricular activity and myocardial damage and coronary atherosclerosis in patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS). The study was conducted on patients with both positive and negative troponin levels using tissue Doppler echocardiography. In patients with NSTE-ACS, the temporal indicators and their ratios can be used to assess the extent of myocardial damage, determine the coronary territory involved, evaluate the potential for recovery and response to therapy, as well as monitor the progression of the disease over time.
Keywords: Tissue Doppler imaging, With non-ST-segment elevation acute coronary syndrome, Isovolumetric relaxation time, Myocardial performance index
Cite this paper: Bekmetova F. M., Yuldoshev N. A., Fozilov Kh. G., Bekbulatova R. Sh., Abdullaeva S. Ya., Koshimov Sh. U., Doniyorov Sh. N., Karimov B. S., Ilkhomova L. T., Khotamova M. N., Arslonov S. F., The Correlation Between Indicators of Time Intervals of Left Ventricular Activity and Markers of Myocardial Damage and Coronary Artery Atherosclerosis in Patients without-ST-Segment Elevation Acute Coronary Syndrome (NSTE-ACS), American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1651-1656. doi: 10.5923/j.ajmms.20231311.12.
Article Outline
1. Introduction
- Acute coronary syndrome (ACS) stands as a prominent contributor to fatality rates across many nations. A significant portion of cardiovascular disease (CVD) mortalities stem from sudden non-ST-segment elevation incidents. Data from the United States' National Registries of Myocardial Infarction (NRMI I, II, and III) exhibits a notable rise in the prevalence of ACS cases lacking ST-segment elevation, surging from 45% to 63% between 1990 and 1999 [6]. Contemporary advancements have introduced novel, non-invasive, advanced methodologies and approaches for diagnosing ACS instances that lack ST-segment elevation.The guidelines concerning ACS without ST-segment elevation propose utilizing echocardiography within the emergency department as a means to aid in distinguishing chest pain syndromes and subsequently stratifying risk among patients [9]. Diagnosis of one variant of acute coronary syndrome emerges from the initial interaction between physician and patient exhibiting clinical and electrocardiographic signs of acute coronary insufficiency. To validate myocardial infarction (MI) as the diagnosis, elevation in cardiac biomarkers within the patient's bloodstream and visualization of evidence indicating myocardial necrosis or abnormal wall movement become imperative. In practicality, the prognosis of ACS patients without ST-segment elevation generally hinges on the extent and severity of myocardial necrosis and remodeling of the left ventricle (LV) [4]. The strategic assessment of risk for these patients holds significance in order to appropriately apply intensified diagnostic and treatment approaches aimed at averting recurrent hospitalizations [1,3].It's recognized that color tissue Doppler imaging (TDI) is a technique capable of assessing cardiac temporal intervals [2,6,8], encompassing isovolumetric contraction time (IVCT), isovolumetric relaxation time (IVRT), ejection time (ET), and myocardial performance index (MPI), calculated as the ratio [(IVRT+IVCT)/ET]. As impairment in LV diastolic function exacerbates, myocardial relaxation decelerates, leading to extension of isovolumetric relaxation time (IVRT) and cardiac time intervals—particularly composite indices that offer insights into both LV systolic and diastolic functions. These indices can serve as non-invasive predictors, unveiling subtle cardiac function impairments within the general population that often elude routine echocardiographic assessments. Results from multiple studies [3,4,7] underscore MPI's potential as a valuable tool for forecasting myocardial damage and adverse outcomes in patients afflicted by diverse CVD.Doppler visualization (TD) similarly proves advantageous in gauging unfavorable outcomes within certain CVD cases. In ACS, several clinical markers such as arterial hypertension (AH), diabetes mellitus (DM), prior stroke/transient ischemic attack (TIA), and LV dysfunction not only worsen in-hospital prognoses but also have repercussions over the long term [10-12].In the investigation led by Okay Abaci et al. [15], it was ascertained that within the high-risk population affected by ACS lacking ST-segment elevation, a straightforward measurement of MPI could serve as a discerning factor in identifying those who might derive advantages from diverse treatment strategies and risk evaluation. Within ACS patients, MPI quantified through tissue Doppler imaging exhibited notable elevation among those with greater infarct dimensions, reduced LV ejection fraction, and more severe ischemic heart disease. Employing tissue Doppler imaging in the study highlighted the exacerbation of diastolic velocity parameters in individuals showcasing normal baseline LV ejection fraction—an autonomous harbinger of mortality. Additionally, the ratio of E/(e's') velocities emerged as a vital, self-sufficient prognostic marker for cardiac incidents among ACS patients [17].In the broader populace, cardiac temporal intervals-comprising data regarding LV myocardial function within metrics such as IVRT/ET and MPI-demonstrated their prowess as not only robust, stand-alone predictors for forthcoming significant adverse cardiovascular events (MACE) but also as sources of supplementary prognostic insight, surpassing the contributions of standard clinical and widely endorsed echocardiographic indicators gauging LV systolic and diastolic functions [1].Furthermore, recognized are the pivotal echocardiographic parameters related to LV diastolic function, encompassing velocity metrics acquired via tissue Doppler imaging (TDI)—these include the early diastolic velocity tied to septal motion (e' < 7 cm/s) and lateral mitral annular movement (e' < 10 cm/s), as well as the ratio denoting the peak early transmitral flow velocity over the early diastolic mitral annular velocity (E/e' > 14) [13]. Correspondingly, findings have established that patients with an E/(e's') ratio ≥ 1.63 exhibited more adverse demographic, echocardiographic, and laboratory profiles, along with a heightened occurrence of SYNTAX scores ≥ 22 in contrast to individuals with lower velocity ratios [16]. According to other authors, distinct outcomes within ACS patients were linked to metrics such as left ventricular ejection fraction (LVEF), the E/e' ratio, mitral deceleration time (DT), and mitral regurgitation [5].The objective of our analysis was to assess the potential of tissue Doppler imaging in detecting myocardial damage through the evaluation of cardiac cycle intervals among individuals affected by non-ST segment elevation acute coronary syndrome (NSTE-ACS). The study encompassed a cohort of 98 NSTE-ACS patients admitted to the Intensive Care Unit of the Cardiology Branch at the Republican Specialized Scientific-Practical Medical Center in Karshi, spanning from June to December 2022. The research was conducted in strict accordance with the Helsinki Declaration, and all participants furnished informed consent for their involvement in the study.Every patient underwent transthoracic two-dimensional echocardiography alongside tissue Doppler imaging within the initial 24-hour span of hospitalization. The process of transthoracic echocardiography was repeated at least twice, with the goal of gauging left ventricular (LV) contractile function. The first instance occurred within the initial 24 hours, followed by a subsequent assessment at the point of discharge. The patient cohort was split into two distinct groups based on whether cardiac troponin I (TnI) levels exceeded 0.04 ng/mL: those exhibiting elevated TnI levels and those devoid of elevation. The measurement of TnI levels was conducted within the initial 10 minutes of hospitalization and then replicated every 4-6 hours across the initial two days. The diagnostic evolution from NSTE-ACS to acute myocardial infarction correlated with the elevation of cardiac troponin I, whereas unstable angina was characterized by the onset of new angina symptoms and the progression of angina without concurrent TnI elevation.The stratification of patient risk and anticipation of both near-term (during primary hospitalization) and extended periods of NSTE-ACS were undertaken using the GRACE score. In this context, low risk was defined as a mortality rate below 1% (as computed using an automated calculator) or a score less than 109 points (determined manually). Medium risk encompassed mortality rates ranging from 1% to 3% (as per automated calculator) or scores between 109 and 140 points (manual calculation). High risk constituted mortality rates surpassing 3% (calculated through automation) or scores exceeding 140 points (manual calculation). The study's exclusion criteria encompassed patients showcasing ST segment elevation across all leads, left bundle branch block, valvular and congenital heart anomalies, atrial fibrillation, cardiomyopathies, past occurrences of myocardial infarction, prior coronary artery bypass grafting or percutaneous coronary intervention, episodes of acute heart failure, systemic ailments, pregnancy, chronic obstructive pulmonary disease (COPD), and emphysema. Patients grappling with mitral regurgitation of a degree higher than II, aortic regurgitation exceeding grade II, tachycardia with heart rates surpassing 100 beats per minute, and mitigated application of pulsed Doppler echocardiography due to mitral stenosis were also excluded from the study.Inclusive to the study, all participants underwent coronary angiography (CAG) through employment of the GE Innova IGS 530 system (manufactured by GE Healthcare, USA) to scrutinize coronary atherosclerosis in accordance with the SYNTAX score algorithm. Stenoses measuring up to 50% in diameter (equivalent to less than 70% in area) were considered marginal, while stenoses surpassing the 50% threshold were deemed significant (exceeding 70% in area).
2. The Methodology of Echocardiography (ECG) and Tissue Doppler Imaging (TDI)
- The approach of utilizing echocardiography (ECG) in conjunction with tissue Doppler imaging (TDI) was employed in this research. The investigation encompassed the utilization of two-dimensional transthoracic echocardiography, conducted on a GE Vivid T8 Pro apparatus (Manufacturer: GE Healthcare, USA). The determination of left ventricular ejection fraction (LVEF) entailed subtracting left ventricular end-systolic volume (LVESV) from left ventricular end-diastolic volume (LVEDV) and then dividing the result by LVEDV. This calculation was performed using Simpson's method, in both the apical two- and four-chamber perspectives (biplane disk method). For assessment of left atrial volume (LA), the endocardial border of the left atrium was traced in the apical four-chamber view.Furthermore, trans-mitral Doppler velocities for early and late diastolic phases (E and A waves, respectively) were acquired by positioning the cursor at the tips of the mitral valve leaflets within the apical four-chamber view. Doppler indices were established utilizing trans-mitral Doppler flow (TMDF). The TMDF profile was obtained by situating the sample volume at the level of the mitral valve leaflet tips in the apical four-chamber alignment. Multiple diastolic function parameters were assessed through standard Doppler ultrasound techniques, including peak E velocity, peak A velocity, ejection time (ET), filling time (FT), deceleration time (DT), isovolumic relaxation time (IVRT), isovolumic contraction time (IVCT), and E/A ratio.IVRT duration was measured through continuous wave Doppler imaging across the left ventricular outflow tract, commencing from the termination of aortic ejection to the onset of trans-mitral flow. Employing tissue Doppler imaging (TDI) from the apical four-chamber perspective, a set of parameters evaluating left ventricular diastolic function was collected. This encompassed measurement of the systolic wave (s') and two diastolic waves (e' and a'), attained by analyzing the movement of the mitral annulus using tissue Doppler imaging. The sample volume was positioned at the septal or lateral side of the mitral annulus. Peak e' and s' velocities were measured over five successive cardiac cycles at the expiration's conclusion and averaged. The average velocities of the septal and lateral segments were utilized for E/e' calculations.The myocardial performance index (MPI) or Tei index was determined through the formula, involving the ratio of isovolumic contraction time and isovolumic relaxation time to ejection time [(IVRT + IVCT) / ET]. This index was computed as the ratio of the interval between the end of one trans-mitral flow to the commencement of the next, relative to the left ventricular ejection time.The amassed data underwent analysis via statistical tools, including SPSS and SAS software. The examination of the correlation between left ventricular timing parameters and coronary atherosclerosis in patients afflicted by non-ST segment elevation acute coronary syndrome (NSTE-ACS) was undertaken through correlation analysis.
3. Results
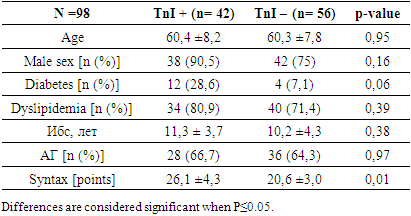
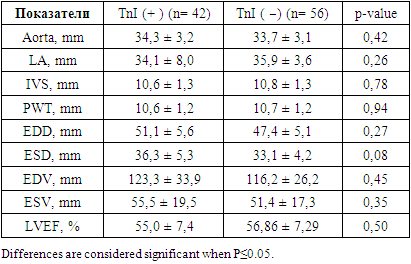
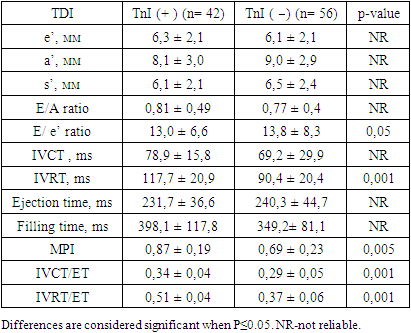
- Results demonstrated that the patient pool was categorized into two groups based on the presence of troponin, a myocardial injury biomarker, in their bloodstream. Group comparisons were conducted, assessing the clinical and demographic attributes of the study cohorts, as presented in Table 1.
|
|
|
|
4. Discussion
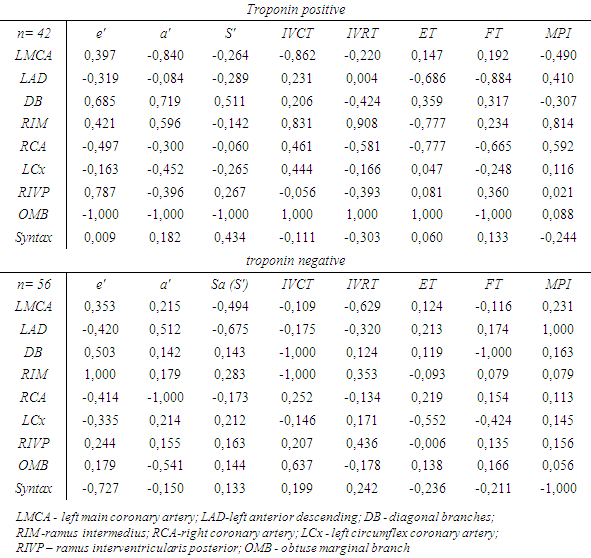
- The relationship between tissue Doppler imaging parameters and myocardial damage in patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS) has been the subject of numerous studies in recent years. A promising parameter that has emerged as a significant indicator of myocardial function is the myocardial performance index (MPI), formulated as the ratio (IVCT+IVRT)/ET. Additionally, certain investigations [4] have illuminated that MPI showcases a heightened sensitivity in reflecting the recovery of viable segments within NSTE-ACS patients post revascularization. Meanwhile, elevated MPI values align with an augmented probability of necessitating revascularization and an escalated risk of adverse cardiovascular occurrences, encompassing heart failure, recurrent myocardial infarction, and mortality [5]. Further endorsement for the applicability of IVCT/ET and IVRT/ET ratios as prognostic markers for cardiovascular events has been lent by a population-based study from 2015, a notion that our study corroborates.An exploration reported in the 2016 edition of the American Journal [18] delved into the correlation between cardiac time intervals, gauged via tissue Doppler imaging in M-mode, hypertension, left ventricular geometry, and forthcoming ischemic cardiovascular ailments. The findings unveiled a significant linkage between the (IVCT+IVRT)/ET ratio and various parameters of left ventricular diastolic function, including the E/A ratio and deceleration time. The study's conclusion posited that cardiac time intervals serve as determinants of impaired cardiac function in individuals burdened with arterial hypertension, irrespective of conventional risk factors, even within participants presenting a normal standard echocardiographic assessment. IVRT/ET and MPI were recognized as independent predictors of forthcoming cardiovascular diseases. In our own study, the ratios involving time intervals-IVCT/ET and IVRT/ET-alongside the myocardial performance index, emerged as discernible indicators of myocardial damage. Distinct differences exist between studies scrutinizing the interplay between time interval ratios and the extent of coronary atherosclerosis, quantified through the Syntax score, within NSTE-ACS patients [16], and our own findings grounded in tissue Doppler imaging parameters. These outcomes substantiate the hypothesis that connections persist between the Syntax score, the coronary artery territory, and tissue Doppler imaging parameters.
5. Сonclusions
- Overall, the study provides valuable insights into the relationship between left ventricular dysfunction and coronary atherosclerosis in patients with NSTE-ACS without ST-segment elevation, highlighting the potential of velocity and temporal parameters of the left ventricle as new markers for early detection of myocardial damage. In essence, the study underscores the potential utility of ratios concerning time intervals, evaluated through tissue Doppler echocardiography, as pivotal indicators for assessing myocardial function and foreseeing cardiovascular events and myocardial impairment among NSTE-ACS patients lacking ST-segment elevation. In addition, it's crucial to highlight that the findings underscore the significance of advancing research endeavors to gain a deeper comprehension of the interplay and linkages between diastolic cardiac function, parameters of myocardial damage, and left ventricular functionality. Broadening the scope of analysis and engaging a more extensive patient pool for examination could yield supplementary evidence, consequently refining the derived conclusions. Subsequent investigations are warranted to validate the applicability of these identified parameters in clinical decision-making processes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML