-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1616-1621
doi:10.5923/j.ajmms.20231311.06
Received: Oct. 11, 2023; Accepted: Oct. 27, 2023; Published: Nov. 2, 2023

Relationship Between Left Atrium Stunning and Left Ventricular Myocardial Hypertrophy
Mehriban Subidinovna Baratova , Malika Jamolovna Rizaeva
Bukhara State Medical Institute named Bukhara State Medical Institute Republican Scientific Center of Emergency Medical Care, Bukhara Branch Bukhara, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Medical School called the phenomenon of myocardial stunning, which means stunning. In addition, the question of whether myocardial stunning has clinical significance, since the decrease in myocardial contractility during stunning is reversible, remained controversial. An increase in blood pressure leads to the development of left ventricular (LV) remodeling, which includes the processes of hypertrophy and dilatation, changes in geometry and impaired systolic and diastolic functions. Structural changes in the LV are accompanied by an overload of the left atrium (LA) and its dilatation, which, in turn, leads to stunning of the LA and is a factor predisposing to the development of rhythm disturbances such as ventricular extrasystoles (VE), atrial fibrillation (AF). On the other hand, this rhythm disturbance itself causes LA dilatation. However, recent research data indicate that a more accurate marker of LA structural remodeling is the LA volume index.
Keywords: Left ventricular remodeling, Left atrial stunning, Cardiac arrhythmias, VE, AF, Arterial hypertension
Cite this paper: Mehriban Subidinovna Baratova , Malika Jamolovna Rizaeva , Relationship Between Left Atrium Stunning and Left Ventricular Myocardial Hypertrophy, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1616-1621. doi: 10.5923/j.ajmms.20231311.06.
1. Introduction
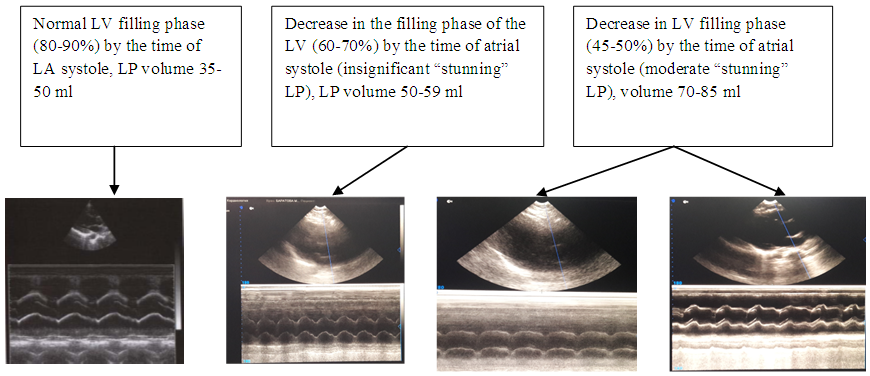
- Changes in blood pressure, starting as a functional disorder, consistently lead to specific organ damage and, in the absence of timely and adequate therapy, to severe cardiovascular complications. One of the significant medical and social problems is arterial hypertension (AH). By 2025, it is predicted that the number of hypertensive patients will increase by more than 1.5 times and will amount to 1.5 billion patients in the world [1,12,17,18,23,27]. Such as disability and premature mortality from the development of complications such as atrial fibrillation, thrombosis of the heart cavities, cerebrovascular accident, myocardial infarction, circulatory failure, etc. Heart changes that occur with arterial hypertension are the cause of the development of heart rhythm disturbances ventricular extrasystoles (VE), tachycardia, atrial fibrillation (AF). Atrial dilatation plays an important role in the development of AF. In 1975, representatives of the Harvard Medical School, led by Heyndrickx G.R., presented the results of an experimental study that examined the effect of ischemia and subsequent reperfusion on myocardial contractility. Later, other representatives of the Harvard Medical School called this phenomenon myocardial stunning, which means "stunning" [13,30,31]. In addition, for a long time the question of whether myocardial stunning has a clinical significance, since the decrease in myocardial contractility during stunning is reversible, remained controversial. Structural changes in the atria such as “stunnedness” or stunning of the myocardium are of particular importance for the development of tachycardia, PVC, AF [5,6,9]. A natural consequence of arterial hypertension (AH) is the formation of left ventricular hypertrophy (LVH), which leads to an increase in left ventricular (LV) rigidity and worsening of its diastolic relaxation, which leads to LV diastolic dysfunction.Arterial hypertension leads to an increase in blood pressure, the development of left ventricular (LV) remodeling, which includes the processes of hypertrophy and deformation of the cavity, changes in geometry and impaired systolic and diastolic functions. Structural changes in the LV are accompanied by hypertrophy of certain parts. An early sign of hypertrophy can be detected during routine examination for echocardiography [3,6,9]. The amount of preload is of great importance in the diastolic function of the ventricles. The compliant ventricle, is easily filled with blood, which contributes to adequate stretching and subsequent contraction of muscle fibers according to the Frank-Starling law. A "hard" ventricle is unable to receive the required volume of blood. In order to achieve stretching of the muscle fibers and provide the necessary preload, an increased filling pressure is required. As a result, the end-diastolic pressure (EDP) in the ventricle increases, which contributes to the preservation of the normal EDP and cardiac output for the time being [1,3]. The consequence of a violation of the extensibility of the ventricular myocardium is also a compensatory increase in atrial contractility, which intensively ejects at the end of the diastola the last volume of blood filling the ventricle, increasing the preload and maintaining the normal stroke volume (SV) and cardiac output. With atrial fibrillation, in the absence of a single atrial contraction, there is a significant decrease in preload, stroke volume and cardiac output [4]. LV diastolic dysfunction promotes hemodynamic overload of the left atrium, its stretching, manifestation of arrhythmic activity in the form of supraventricular rhythm disturbances - extrasystole, atrial fibrillation [14]. Back in 1964 G.K. Moe et al. came to the conclusion that any increase in the size of the left atrium increases the likelihood of developing atrial fibrillation [23].And in 1986 M.S. Kushakovsky described dilatation of the left atrium as a prerequisite for the inevitability of atrial fibrillation [9,18]. It is known that atrial myocardial dystrophy with their subsequent "primary" and "secondary" (retrograde) expansion create a substrate for sinus rhythm disturbances (SR). However, earlier, in 1949, E. Phillip and S. Levin reported on the possibility of developing paroxysms of tachycardia, atrial fibrillation (AF) in people who do not have any heart disease, except for the tachyarrhythmia itself. Diagnosis of disorders of diastolic function is based mainly on the use of instrumental methods [20,21,25,26,30,31]. To assess diastolic function in a clinical setting, two approaches are used: a) assessment of active and passive characteristics of relaxation; b) analysis of the structure of diastolic filling. It is known that in hypertension, remodeling of the left ventricle (LV) develops, including the processes of hypertrophy and dilatation, changes in geometry and impairment of systolic and diastolic functions [13,26]. Structural changes in the LV are accompanied by LA overload and its dilatation, which, in turn, is a factor predisposing to the development of rhythm disturbances. On the other hand, this rhythm disturbance itself causes LA dilatation [15,17,22,28]. However, recent research data indicate that a more accurate marker of LA structural remodeling is the LA volume index (LPI) [21,31].In 1989. W. Manning et al. demonstrated in their studies that in most patients with persistent AF, after restoration of sinus rhythm, a phenomenon of temporary mechanical LA dysfunction was observed, characterized by the authors as the phenomenon of "stunning" or "stunning" [22]. And in subsequent studies by other authors, the phenomenon of inhibition of the function of the LA and its ear was confirmed [16,14,21]. In 1988 I. Van Dam et al. proposed to use a combined index - the ratio of the velocities of the peaks E and A of the transmitral blood flow [32]. If relaxation of the left ventricle is impaired, the decrease in pressure in it during diastole slows down, which in turn leads to a decrease in the rate of early filling (peak E). As a result, there is an increase in the filling volume and the rate of contraction of the left atrium (peak A). The important thing to detect irregular rhythm is existing heart’s structural pathology which is called a stanning of LA [2,5].In the mosaic lesion of the myocardium, there are areas without signs of mechanical activity, but with preserved basic physiological functions. Departure from this ideal geometry dictates the need for early application of diagnostic methods for the "dormant", "stunned" left atrial myocardium. Thus, the diagnosis of stanning LP in arterial hypertension with normal and latent diastolic dysfunction in the analysis of literature data allows us to conclude that currently it is insufficiently studied.Purpose of the study: To diagnose left atrial stunnid in patients with arterial hypertension with normal and latent left ventricular diastolic dysfunction. The research results were processed using the statistical processing packages Statistica, version 6.0. The research used the methods of mathematical statistics: methods of variation statistics, frequency, variance and correlation analyzes. The significance of differences in the groups was determined using the t-test (Student's test).
2. Material and Research Methods
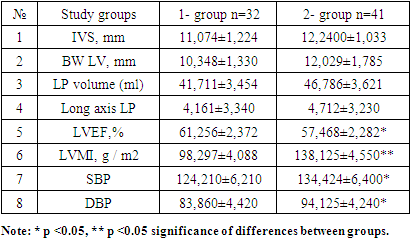
- On the basis of the regional cardiological dispensary, a retrospective study was made of 73 outpatient records of patients with essential hypertension and rhythm disturbances aged 30 to 56 years (average age 40.2 ± 2.7 years). The observation period was 6 months. Patients complained of palpitations, recurrent discomfort behind the breastbone, feeling short of breath, and destabilization of blood pressure. A Holter ECG and an ultrasound examination (ECHOKG) were performed. In order to diagnose left ventricular (LV) remodeling, the myocardium mass, myocardial mass index, and relative wall thickness index were determined. To assess the geometric model of the LV, the classification was used (normal LV geometry, concentric left ventricular remodeling - LV, concentric LV hypertrophy - eccentric LV hypertrophy). The patients were divided into 2 groups: group 1 (n = 32) with hypertension without heart rhythm disturbances. The duration of hypertension was 4.894 ± 2.21 years, in group 2 (n = 41) with hypertension and cardiac arrhythmias - tachycardia, VE, impaired repolarization of the ventricles. The duration of hypertension in this group was 5.820 ± 3.21 years. In the presented group, during the study, we identified the following variants of heart rhythm disturbances: tachycardia - 10 (24%), frequent ventricular monotopic extrasystole - 18 (44%), polytopic - 6 (33%), atrial fibrillation - 13 (32%). The diagnosis was established on the basis of anamnestic, clinical, laboratory data, as well as the results of a functional diagnostic study, echo cardiographic examination and examination of the fundus, if necessary, consultation of a neuropathologist. Symptomatic arterial hypertension was excluded based on the results of the study of general blood, urine, biochemical parameters, and ultrasound examination of the kidneys. Among the patients studied, there were also no patients with ischemic heart disease, with signs of heart and renal failure, anemia, lung disease, diseases, thyroid gland, diabetes mellitus.Systolic and diastolic blood pressure was measured for all subjects, echocardiographic studies were performed on the dimensions of the left atrium along the long axis and in the 2-chamber position, the transmitral flow, the thickness of the interventricular septum and the posterior wall of the left ventricle.The primary study and the decision to enroll in the study were carried out within the first 2-3 days after contacting the clinic. During this period of time, patients did not receive drugs that could affect hemodynamics. The studies were carried out in a polyclinic on a SANNOMED-500 ultrasound machine. During echocardiography along the long axis, the end diastolic (EDV) and end systolic (ESV) volumes of the left ventricle were determined, along the long axis and in the apical 2-chamber position, the systolic volumes of the left (VLP), the size of the LP. With the help of pulse-wave Doppler, the degree of mitral regurgitation was specified. To assess the systolic function of the left ventricle, the ejection fraction (LVEF) was calculated. Violation of left ventricular diastolic function was diagnosed if people under the age of 50 had less than 55 cm/s.Statistical processing of the obtained results was carried out using the statistical package "Statisticav.6.0". The arithmetic mean (M) and the error of the mean (m) were calculated. The normality of the sample distribution was assessed by the Kolmogorov - Smirnov test. The reliability of the differences between the values was determined using the Student's t-test with a normal distribution of the trait, with the distribution of a trait different from normal - using the nonparametric Mann - Whitney method. For the analysis of qualitative features, Fisher's exact test and χ2 were used. Differences were considered significant at p≤0.05.
3. Results of the Study
- ECG changes were diagnosed in the first group 40.13% of cases, in the second group 47.71% of cases and in the third group 12.14% of cases, risk distribution: risk 1 - 53 people. (35.58%), risk 2 - 50 people. (33.50%), risk 3 - in 39 people. (26.17%), risk 4 - in 7 people. (4.75%). In total, changes in the analyzed ECG parameters were detected in 48.99% of cases.Research algorithm:
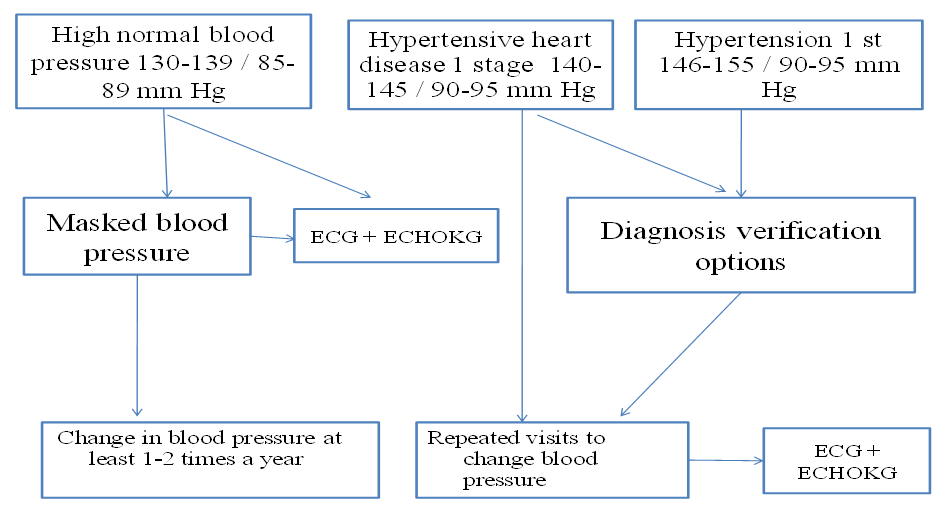 | Figure 1 |
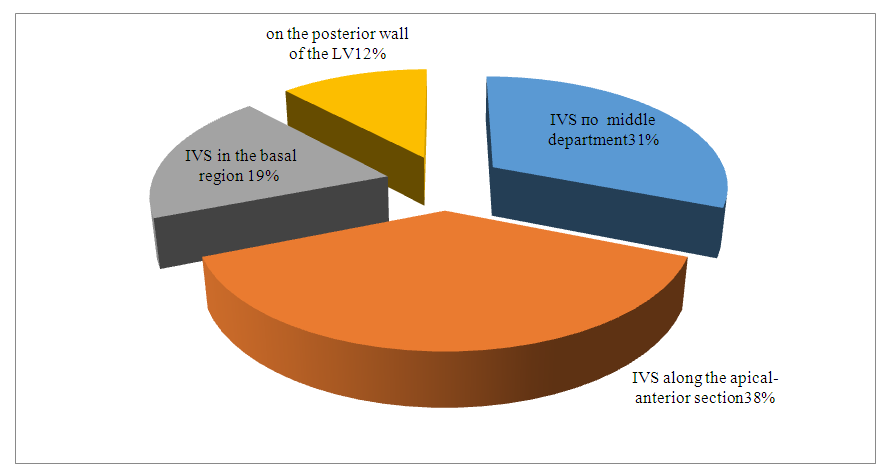 | Figure 2. EchoCG indices of changes in the interdigital septum and the posterior wall of the left ventricle in the subjects |
 | Figure 3 |
|
4. Conclusions
- In patients, the electrocardiogram in 39.5% reveals changes associated with stanning of the left atrium, leading to impaired intraventricular conduction, early repolarization syndrome and cardiac arrhythmias (tachycardia, extrasystoles). Remodeling was observed, leading to hypertrophy of certain parts of the myocardium, and in 31.5% of cases, the concentric type of hypertrophy occurs, which is considered the most unfavorable in prognostic terms, which requires more careful monitoring of this category of patients. The examined patients showed early signs of left ventricular diastolic dysfunction, diastolic dysfunction is mainly represented by hemodynamic disorders and early stanning of the left atrium (67%). It is certain that with atrial contraction and their relation to the transmitral blood flow in LV hypertrophy leads to a partial absence of atrial systole (peak A) as well as to a decrease in the speed of atrial systolic blood flow less than 0.5 m/sec.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML