-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1604-1607
doi:10.5923/j.ajmms.20231311.03
Received: Oct. 1, 2023; Accepted: Oct. 22, 2023; Published: Nov. 2, 2023

Evaluation of the Effect of Angiotensin II Receptor Blockers on the Example of Azilsartan Medoxomil (Edarbi) on the Functional State of the Kidneys in Metabolically Healthy Obesity
I. I. Islomov1, A. G. Gadaev2, O. S. Yuldashev3, B. R. Fayzullayev3, A. I. Abdullayev4
1Urgench Branch of Tashkent Medical Academy, Private Clinic Elite Clinic at Shifo Quvonch Fayz Ltd, Urgench, Uzbekistan
2Tashkent Medical Academy, Tashkent, Uzbekistan
3Urgench Branch of Tashkent Medical Academy, Urgench, Uzbekistan
4Urgench Branch of Tashkent Medical Academy, MEDCOMPLEX Private Clinic, Urgench, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

One of the features of kidney damage is that, regardless of the etiological factor, there is atrophy of the renal tubules, interstitial fibrosis and cellular infiltration, and this can lead to an increase in the size of the interstitium, as well as minor changes in glomerular filtration in the early stages of the process, and the mediators of these processes are mainly chemotactic, pre-inflammatory and vasoactive, fibrogenic, apoptic, the increased overexpression of antigenic and adhesive receptor biomarkers in relation to growth-stimulating cytokines and these molecules on the surface of target cells is described in detail in the chapter of the literature review on the sequence of processes of tubulointerstitial fibrosis, beginning with damage, ending with the formation of fibrous tissue and organ destruction.
Keywords: Renal functional reserve (RFR), Interstitial fibrosis, Glomerular filtration rate, Kidneys, Creatinine, Transforming growth factor beta-1 (TGFß1), Angiotensin II receptor blockers
Cite this paper: I. I. Islomov, A. G. Gadaev, O. S. Yuldashev, B. R. Fayzullayev, A. I. Abdullayev, Evaluation of the Effect of Angiotensin II Receptor Blockers on the Example of Azilsartan Medoxomil (Edarbi) on the Functional State of the Kidneys in Metabolically Healthy Obesity, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1604-1607. doi: 10.5923/j.ajmms.20231311.03.
Article Outline
1. Introduction
- Interstitial fibrosis is initially caused by a violation of the processes carried out by elements of the extracellular matrix and the basement membrane aimed at maintaining the normal structure of the tissue, in particular the control of fibrogenesis [1]. In pathological conditions, as a result of fibrosis, ischemia increases with narrowing of vessels, cavities of peritubular capillaries [2]. This process of fibrosis leads to scarring of interstitial tissue and tubular epithelium, tissue destruction and transdifferentiation of tubular epithelial cells. It reacts to damage to epithelial cells by undergoing the following changes: proliferation or epithelial-mesenchymal transformation (EMT) [3,4]. The process of transformation of the tubular epithelium into fibroblasts using EMT is considered to be an unexplored mechanism of fibrosis development [5,6,7]. There are several mediators involved in this process, which are mainly produced by infiltrating cells [8], which complement the endothelium of peritubular capillaries, and macrophages [9,10], which proliferate and play an important role in the progression of damage to the renal parenchyma in chronic kidney disease (CKD).Chemoattractants secreted by the basement membrane of damaged tubules involve inflammatory cells (monocytes and lymphocytes) in the process and cause fibroblast proliferation. This process, in turn, proceeds with the formation of a broken connection between fibrogenesis and inflammation. [11]. In this process, specially activated tubule cells produce the following biomarker-chemoatractant cytokine-transforming growth factor beta-1 (TGFß1) [12]. As fibrogenesis is activated, the accumulation of this marker increases. When the kidneys of patients with CKD were examined by biopsy, it was found that the main element of inertia tissue are myofibroblasts, and that they are closely related to the degree of fibrosis, that is, there is a correlation [13,14]. Activated myofibroblasts are considered a histological marker of outbreaks of kidney diseases. [15,16] Myofibroblasts can be formed by transdifferentiation of fibroblasts, tubular epithelial cells, vascular pericytes and macrophages [4,17,18].Myofibroblasts begin to accumulate around the damaged renal ducts and arterioles. Ischemic and hemodynamic changes in borax beads occur in the presence of vasoactive mediators: angiotensin II and endothelin-1, when microvascular obliteration occurs due to fibrosis and vasoconstriction. As these changes increase, the accumulation of tgfß1 also increases. From the above it becomes known that one of the factors playing an important role in kidney damage is angiotensin II. In this regard, it is advisable to use angiotensin II receptor blockers in order to prevent CKD and other types of kidney damage. This is evidenced by the fact that in some researchers, the concentration of fibrosis factors when using drugs belonging to this group reduces the level of fibrosis in organs and tissues, such as kidneys and other organs, especially the heart and liver [4,17,18].In addition to above data published by us else publication about comparing to GFR, RFR detection allows a more accurate assessment of kidney function. Walking, which is one of the methods of treatment without drugs, in turn has a positive effect on the functional state of the kidneys. It became known as a result of our study that this positive effect also depends on the intensity and duration of walking. Because the rate of RFR improvement between walkers 1 hour a day and more has been found to be significantly and convincingly high compared to walkers around 30 minutes a day.
2. Objective
- Evaluation of the effect of angiotensin ii receptor blockers on the example of azilsartan medoxomil (edarbi) on the functional state of the kidneys in metabolically healthy obesity. For this situation we use low doses of azilsartan medoxomil (edarbi) especially 10 mg a day, because this dose is calculated twice as low as the recommended dose of the drug according to guidelines recommendations.
3. Material and Methods
- In total 123 individuals, including 83 individuals with metabolic healthy obesity at levels 1 and 2, 20 practical healthy individuals from the South Aral Sea Region, 10 practically healthy individuals from the Qibray District of the Tashkent region, and 20 individuals with metabolic healthy obesity were selected. They were between 25 and 50 years old and averaged 36.83±0.72. Females made up 45 (54.21%). All individuals were placed on outpatient observation and separated into primary and control groups. The core group was divided into 2 groups based on body mass index (BMI): 1 group was made up of 46 individuals with metabolic healthy obesity comprising BMI 30-34.9 kg/m2,2 groups were made up of 37 individuals with metabolic obesity comprising BMI 35-39. 9 kg/m2. The control group was made up of 20 practically healthy individuals from the South Islet Region, 10 practically healthy individuals from the Qibray District of the Tashkent region and 20 individuals with metabolic healthy obesity. Even 50% less than the recommended minimum hypotensive dose of the drug Edarbi, i.e. 10 mg per day, from the group I and II of patients of the established group involved in the trial, and the indicators of the functional state of the kidneys after the 3rd and 6th month of the initial and follow – up of patients – estimated glomerular filtration rate (eGFR) and functional reserve of kidneys (FRK) were compared.
4. Results and Discussion
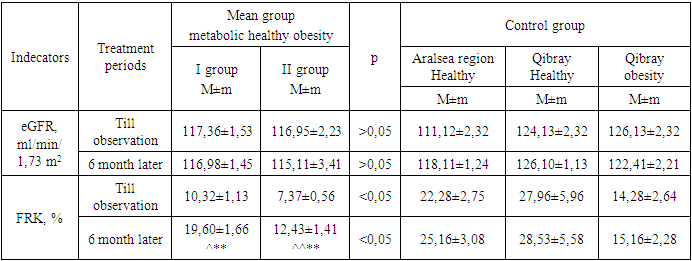
- In the group of Group I receiving 10 mg per day of Edarbi peraratin, this indicator, when examined for observation and pre-intervention eGFR, was 117.36±1.53 ml/min/1.73 m2, while in the 3rd month this indicator was 119.50±1.79 ml/min/1.73 m2, and by the 6th month of the study, the eGFR indicator was 116.98±1.45 ml/min/1.73 m2 (p>0.05). However, it has been known that the differences are at an implausible level when these changes are compared with indicators before and after observation and interventions and in control group representatives, which also expresses an inadequacy in assessing the functional state of the eGFR kidneys. In the case of FRK indicators, the following results were recorded: the FRK average before observation and intervention was 10.32±1.13%, while the average of this indicator in the 3rd month of observation was 13.61±1.10%, and by the 6th month of examination was 19.60±1.66%, in which the results differed convincingly before and after treatment and in relation to the control group (p<0.001). In order to more accurately represent such a growth rate of dynamism, we will consider dividing patients into 3 groups according to the types of FRK condition. It is known that we divided each of the main group into “no”, “decreased” and “saved” groups of reserves according to the FRK. Earlier in the study, the ratio of this group I to Edarbi intake-initial FRK indicators was as follows: the number of patients without or “no” FRK was 4 , patients with a “decreased” in FRK was 1, and the number of patients with FRK “saved” was 13. By 6 months of the study, no patients with “decreased” were observed at all, that is, due to their improvement in FRK, these group patients joined FRK “decreased” and “saved” groups, the number of patients with a decrease in FRK increased from 1 to 2 people, this increase occurred due to the addition of FRK among them to the group of those with, the initial FRK indicator was found to have increased by 90% by the 6th month of observation and intervention (χ2=29,478; p=0.00026).In the group of Group II that received 10 mg per day of Edarbi, this indicator, when examined for observation and pre-intervention eGFR, was 116.95±2.23 ml/min/1.73 m2, while in the 3rd month this indicator was 117.39±3.07 ml/min/1.73 m2, and by the 6th month of the study, the eGFR indicator was 115.11±3.41 ml/min/1.73 m2 (p>0.05). However, it has been known that the differences are at an implausible level when these changes are compared with indicators before and after observation and interventions and in control group representatives, which also expresses an inadequacy in assessing the functional state of the eGFR kidneys. In the case of FRK indicators, the following results were recorded: the average FRK before observation and intervention was 7.37±0.56%, while in the 3rd month of observation, the average of this indicator was 9.58±0.76%, and by the 6th month of examination, 12.43±1.41%, in which the results differed convincingly before and after treatment and compared to the control group (p<0.001). In order to more accurately represent such a growth rate of dynamism, we will consider dividing patients into 3 groups according to the types of FRK condition. It is known that we divided each of the main group into “no”, “dropped” and “saved” groups of reserves according to the FRK. Earlier in the study, the ratio of this group I to Edarbi intake-initial FRK indicators was as follows: the number of patients without FRK was 8 , patients with a decrease in FRK was 2, and the number of patients with saved FRK was 0. By 6 months of the study, no patients with FRK were observed at all, that is, due to their improvement in FRK, these group patients joined FRK decreased and stored groups, the number of patients with FRK decreased increased from 2 to 4, this increase occurred due to the addition of FRK to the group of saved among them, ultimately the growth rate of FRK, the initial FRK indicator was found to have increased by 69% by the 6th month of observation and intervention (χ2=29,478; p=0.00026). These indicators are presented in Table 1.
|
5. Conclusions
- In conclusion, from the above data and results, it can be confirmed that any damage to the kidneys is followed by interstitial fibrosis and cellular infiltration, no matter what the reasonable factor is, and this can lead to the enlargement of the inertial cell, as well as a slight change in the filtration of the balls in the early stages of the process, and the mediators of, increased hyperexpression of growth-stimulating cytokines and target cell surfaces of antigen and adgesive receptor biomarkers relative to these molecules, a sequence of processes in tubulointerstisial fibrosis course results in fibrotic tissue formation and limb degradation. The role of angiotensin II, one of the factors that play an important role in these fibrosis processes, has been found to be extremely important. In this view, it is advisable to use angiotensin II receptor blockers with the aim of obtaining for CKD and other types of kidney damage. This is true in some research, in which it was shown that the concentration of fibrosis factors when drugs including into this group were used decreased levels of fibrosis in organs and tissues such as the kidneys and other organs, in particular the heart and liver. In this context, the effect of the drug Edarbi, aimed at improving the functioning of the kidneys, this is explained by the decrease in the processes of fibrosis carried out through its angiotensin II.The indicators in this table are described in the diagrams as follows:
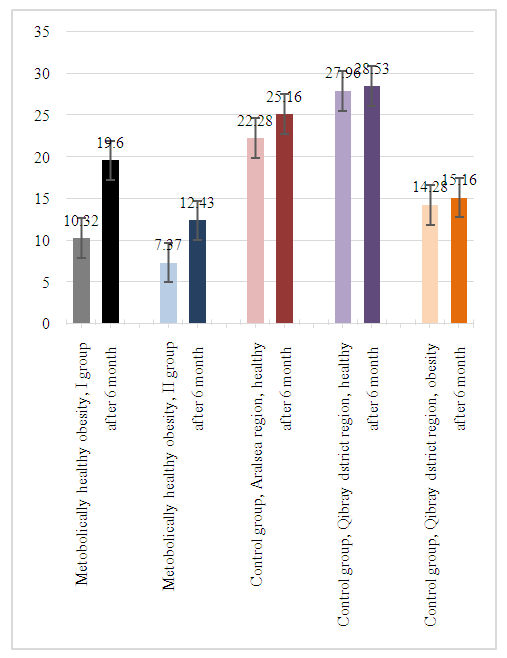 | Figure 1. Assessment of the effect of the drug azilsartan medoxomil (Edarbi), an antagonist of angiotensin II receptors, on the functional state of the kidneys in metabolic healthy obesity |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML