-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(10): 1587-1590
doi:10.5923/j.ajmms.20231310.46
Received: Oct. 11, 2023; Accepted: Oct. 25, 2023; Published: Oct. 27, 2023

COVID 19 Disease Severity Prediction Using Blood Urea Nitrogen/Creatinine Ratio and Other Regular Blood Indicators
Tillyashaykhova Iroda Mirzagalebovna1, Parpiyeva Nargiza Nusratovna2, Rakhimova Gulnara Nishanovna3
1PhD Researcher, Republican Scientific and Practical Medical Center of Phthisiology and Pulmonology, Uzbekistan
2Doctor of Medical Sciences, Professor, Director of the Republican Scientific and Practical Medical Center for Phthisiology and Pulmonology, Uzbekistan
3Doctor of Medical Sciences, Professor, Head of the Department of Endocrinology at the Center for the Development of Professional Qualification of Medical Workers, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

There is growing evidence that renal impairment is accompanied by coronavirus disease 2019 (COVID-19). The relationship between renal dysfunction brought on by the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) and prognosis is still unclear. From normal blood measures, particularly the blood urea nitrogen (BUN)/creatinine (Cr) ratio, we sought to investigate independent predictors of the severity and prognosis of COVID-19 disease. This was a retrospective study conducted at the Zangiota Infectious Diseases Hospital of Respublic Uzbekistan. Data from the lab were extracted, together with demographic traits. There were 114 (82.6%) non severe and 24 (17.4%.) severe cases in 138 COVID-19 patients. The most common comorbidities were hypertension (52.9%), CVD (18.3%) diabetes (27.5%) in the both groups. But, the rates of total comorbidities, HT, and heart disease were significantly higher in the severe group. COVID-19 severity differs between patients. Age, comorbidities, and immunological state are the biggest risk factors for disease severity.
Keywords: COVID-19, Renal dysfunction, Blood urea nitrogen, Prognosis
Cite this paper: Tillyashaykhova Iroda Mirzagalebovna, Parpiyeva Nargiza Nusratovna, Rakhimova Gulnara Nishanovna, COVID 19 Disease Severity Prediction Using Blood Urea Nitrogen/Creatinine Ratio and Other Regular Blood Indicators, American Journal of Medicine and Medical Sciences, Vol. 13 No. 10, 2023, pp. 1587-1590. doi: 10.5923/j.ajmms.20231310.46.
Article Outline
1. Introduction
- In the latter half of 2019, unknown pneumonia cases began to arise in Wuhan, China. (Hubei province). [1,2] A new betacoronavirus subtype was discovered in China in January 2020 using high throughput sequencing and throat swab data. [3] The World Health Organization (WHO) designated this coronavirus disease as "COVID19" and called it a significant international pandemic and public health issue. [4] According to WHO figures, as of early May 2020, over 3 million global cases had been confirmed, with over 20 000 deaths [5]. As a result, all medical practitioners, scientific researchers, and all sectors of society must work together to reduce COVID-19 spread and discover appropriate therapies, medications, and methods. Nonetheless, the clinical features of renal impairment caused by SARS-CoV-2 are rarely described. Furthermore, the clinical significance of SARS-CoV-2-induced renal impairment and its recovery status are still unknown. In humans, the end products of nitrogen metabolism are blood urea nitrogen (BUN) and creatinine (Cr). They can be easily filtered from the nephrons because they are tiny molecules. Typically, roughly 30% to 40% of BUN is Typically, 30% to 40% of BUN is reabsorbed from tubules, whereas Cr is poorly reabsorbed [6,7]. The primary goal of this study was to determine whether SARS-CoV 2 caused renal impairment, as well as its risk variables, such as age and comorbidities, in COVID-19 patients. The goal of this study was to assess the role of applicable and costeffective BUN/Cr ratios, as well as other regular blood indicators, in predicting COVID19 disease severity.The purpose of this study was to assess the role of applicable and costeffective BUN/Cr ratios, as well as other regular blood indicators in predicting the severity of COVID19 disease.
2. Materials and Methods
- This was a retrospective study conducted at the Zangiota Infectious Diseases Hospital of Respublic Uzbekistan. All methods were performed in accordance with relevant guidelines/regulations and in accordance with the Declaration of Helsinki. Study population included 138 patients admitted to the hospital with Sars-Cov2 positive RT-PCR nasopharyngeal swab, from July, in 2022. The hospital was totally converted to COVID-19 management during the pandemic outbreak. Multidisciplinary teams composed by internist, pneumologist, nephrologist, infectious disease specialist, emergency care physician and anesthetist were established. Inclusion and exclusion criteriaThe analysis included all COVID-19 patients aged ≥ 18 years who resulted positive to at least 2 Sars-Cov2 positive RT-PCR nasopharyngeal swabs, and whose radiological findings documented pulmonary disease (via either X-ray or CT scan), based on the Republican Specialized Medical Center Zangiota. Individual signed informed consent was gained from patients.Exclusion criteriaThe exclusion criteria were age < 18, pregnancy, lactation, patients with negative IgSARS-CoV-2 and patients participating in any other clinical trial.Data collectionIn COVID-19 patients, the hospital stay was calculated. Demographic information as well as clinical variables were gathered. COVID-19's severity was assessed. Age, gender, blood pressure, comorbidities such as cardiovascular disease (CVD), diabetes, hypertension, chronic obstructive pulmonary disease (COPD), and malignancies were all obtained at the time of hospital admission. The following parameters were measured: complete blood count, blood urea nitrogen, uric acid, and estimated glomerular filtration rate (eGFR). Standard techniques were used to assess peripheral venous blood samples. All laboratory tests were carried out at the Zangiota Infectious Diseases Hospital's clinical laboratory.The routine blood tests (including white blood cell count [WBC], leukocyte subtypes, and platelet count) were measured with Sysmex XN-L 550 automatic hematology analyzer (Sysmex America, Inc.) Mindray BC-380 automated biochemistry analyzer (Mindray Bio-Medical Electronics Co, Ltd, Shenzhen, China). was used to measure the biochemical parameters. Statistical analysisStatistical data analysis was performed using MS Excel 2016 software. For static calculations, the arithmetic mean, standard deviation, and percentage were used.
3. Results
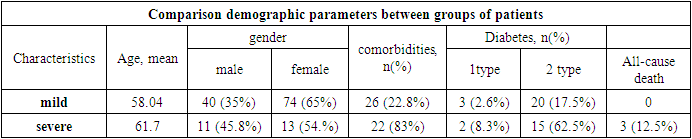
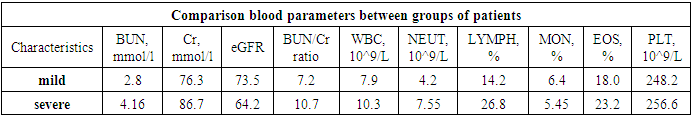
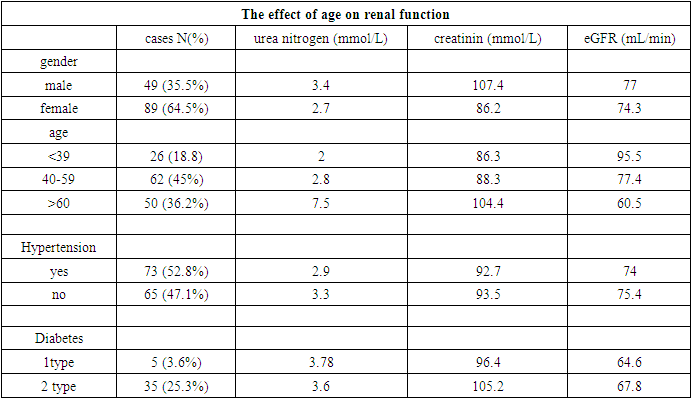
- Demographic information and clinical manifestations All 138 COVID-19 patients were enrolled and analyzed of the Republican Specialized Medical Center Zangiota of Respublic Uzbekistan. Our research shown, of COVID-19 patients, 49 (35.5%) were male and 89 (64.5%) were female. There were 69 patients 26 years old <39 years old, 62 patients aged between 40 and 59 years, and 50 patients >60 years old. The median duration of hospitalization was 11.5 days.The number of non-severe patients was 114 (82.6%). Severe patients made up 17.4% of the total. Furthermore, demographic data were analysed. In all groups, the most prevalent comorbidities were hypertension (52.9%), CVD (18.3%), and diabetes (27.5%).
|
|
|
4. Discussion
- COVID19 has an average incubation period of three days and is readily transmitted from person to person, leading to a rapid pandemic. Patients with mild or moderate COVID19 have milder symptoms and a better prognosis than patients with severe or critical disease, who typically have more complex symptoms and a high mortality rate. COVID19 can be treated and managed more effectively by determining the predictive variables for severe disease using routine blood tests. The demographic, comorbidity, and typical blood parameters of 138 COVID19 patients were evaluated to identify prospective biomarkers for disease severity and survival. This was a retrospective research conducted at the Zangiota Hospital for Infectious Diseases in the Republic of Uzbekistan. The age distribution of COVID19 varies significantly. According to our data, patients with severe conditions were elderly. Rates of total comorbidities, HT, and heart disease were higher in patients with severe conditions. The clinical characteristics of our patient populations are consistent with those of other investigations. According to Yuwei et al., the overall mortality rate was 13.47%. Our cohort had a total mortality rate of 12.5%. COVID19 progression and prognosis are primarily determined by the immune status and inflammatory response of the body. Neutrophils are a vital component of the leukocyte family and play a crucial function in the immune response. NEUs generate reactive oxygen species, which degrade the DNA of virus cells. In addition to interacting with various compartments, NEUs produce a large number of cytokines and mediators, particularly vascular endothelial growth factor. However, lymphocytes are primarily involved in the human immune response induced by a viral infection. Systemic inflammation reduces CD4+ T lymphocytes and increases suppressive CD8+ T lymphocytes by reducing cellular immunity markedly. Consequently, viral-caused inflammation increases the NLR. Several investigations have analysed the leukocyte counts of COVID19 patients at various clinical stages. In their study, Qin et al. found that the neutrophil count was greater and the lymphocyte count was reduced among COVID19 patients in the severe group compared to those in the nonsevere group. As a result, those with severe infection had greater NLR levels. The NLR linked with illness severity in this research as well. The key indicators of kidney function are BUN and Cr levels, as well as the BUN/Cr ratio. The BUN/Cr ratio is critical in the treatment and clinical followup of patients with acute myocardial infarction (AMI), with a clear association between a high BUN/Cr ratio and AMI patients' longterm mortality. According to Yoichi et al, the BUN/Cr ratio is connected with an increased risk of mortality in AHF patients. Gotsman et al found that the BUN/Cr ratio on admission was linked with higher 1 year and longterm (mean: 6.5year followup) mortality in patients with AHF in their research. Brisco et colleagues discovered a link between a high admission BUN/Cr ratio and higher mortality. Coronavirus can alter kidney function by directly entering renal cells through ACE230 and stimulating the reninangiotensinaldosterone system (RAAS) with the systemic effects it produces. The RAAS promotes water and salt absorption in the renal tubules, resulting in passive reabsorption of BUN. These systemic effects promote renal vasoconstriction, which reduces glomerular filtration and BUN excretion. Regardless, the BUN/Cr ratio rises when Cr is filtered by the glomeruli rather than reabsorbed. In light of this knowledge, the authors believe that the BUN/Cr ratio can be used to predict the severity and survival of COVID19. This is the first study to look at the impact of the admission BUN/Cr ratio on the severity and survival of COVID19. The Cr counts in this cohort were comparable in the severe and nonsevere individuals. In the severe patient group, the BUN/Cr ratio was greater. Finally, the study found that a high BUN/Cr ratio and a low NLR were independent predictors of COVID19 disease severity and survival. The BUN/Cr ratio and NLR can give useful information in the first assessment of COVID19 patients. Because they are costeffective and simple to administer, the BUN/Cr ratio and NLR are suggested for use in predicting the severity of COVID19. There were several limitations to this investigation. First, because this was a retrospective, singlecenter clinical investigation, the sample size was modest. Second, despite efforts to account for several confounders, additional unknown factors may have had a role. Third, no data were available from the group of mild patients who were discharged at the time of admission. Fourth, there was inadequate information about things like a high protein diet, which might have altered the baseline BUN/Cr ratio. Because of these constraints, multicenter extensive research are required.
5. Conclusions
- COVID19 severity varies from patient to patient. The primary risk factors determining disease severity and important differently risk factors for renal dysfunction include advanced age, comorbidity, immunological status, and hypertension. Severe sickness has a low survival rate. The BUN/Cr ratio and NLR may be related with illness severity, and routine use of these markers in disease assessment may be useful. Overall, this investigation focused on SARS-CoV-2-induced renal failure at the Zangiota Infectious Diseases Hospital of the Republic of Uzbekistan. These findings show that renal failure is more common in severe COVID-19 individuals.
ACKNOWLEDGEMENTS
- We would like to express our gratitude to all healthcare professionals and hospital administrators who laboured tirelessly during the pandemic.
Conflict of Interests
- The authors declare that there are no conflict of interests.
Ethics Statement
- All methods in research involving human subjects were carried out in line with the Institutional Research Committee's ethical standards, as well as the 1964 Helsinki Declaration and its subsequent revisions or similar ethical standards.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML