-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(10): 1532-1536
doi:10.5923/j.ajmms.20231310.34
Received: Sep. 24, 2023; Accepted: Oct. 10, 2023; Published: Oct. 13, 2023

Nature of Cardiolatation Complications in Patients with Cardia Achalasia
Z. M. Nizamkhodjaev, R. E. Ligai, A. S. Babajanov, A. O. Tsoi, Kh. N. Bekchanov, J. A. Khadjibaev, K. B. Babajanov, A. D. Abdukarimov, J. Avalbayev
Republican Specialized Scientific and Practical Medical Center of Surgery Named after Academician V. Vakhidov, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the research was to study the effect of infrared pulsed laser radiation and an improved cardiodilator model as methods of preventing complications of cardiodilation in patients with neuromuscular disorders of the esophagus. Introduction. For the first time, a pneumatic cardiodilator for the treatment of the esophagus neuromuscular diseases was developed in the 50s of the last century, and in the Soviet Union it became widely used only since 1964 by modification developed in the same year by O.D. Fedorova and G.M. Melnik. After more than half a century, the device of the pneumatic cardiodilator has not undergone much structural changes. The results of cardiodilation are evaluated by many authors in different ways. Material and methods. Clinical material was divided into two groups. In the comparison group, only pneumatic cardiodilation was used, and, a combination of low-intensity laser radiation and a new utility model of a dilator was used in the main group. Results. After dilatation courses, 685 (84.2%) patients had no complications, and 128 (15.7%) patients had various complications. The most common complication was reflux esophagitis, which was observed in 95 (37%) patients. Discussions. Thus, in the main group, the number of bleedings was observed in 12 (3.3%) patients, while in the comparison group this indicator was noted in 54 (11.8%) patients, and in the main group it decreased to 19 and made up 5.3%. Non-penetrating esophageal injuries in the comparison group were noted in 25 (5.4%) patients, while in the main group this indicator decreased to 4 (1.1%) patients. Conclusion. The use of low-intensity laser radiation in combination with a new model of cardiodilator significantly reduced the total number of complications from 20% to 10%. In the structural analysis of complications, thanks to new technologies and our own developments, a significant reduction in almost all types of com-plications was also achieved from 44.8% to 14.3%.
Keywords: Neuromuscular diseases of the esophagus, Achalasia cardia, Laser therapy, Pneumatic cardiodilation
Cite this paper: Z. M. Nizamkhodjaev, R. E. Ligai, A. S. Babajanov, A. O. Tsoi, Kh. N. Bekchanov, J. A. Khadjibaev, K. B. Babajanov, A. D. Abdukarimov, J. Avalbayev, Nature of Cardiolatation Complications in Patients with Cardia Achalasia, American Journal of Medicine and Medical Sciences, Vol. 13 No. 10, 2023, pp. 1532-1536. doi: 10.5923/j.ajmms.20231310.34.
1. Introduction
- For the first time, a pneumatic cardiodilator for the treatment of the esophagus neuromuscular diseases was developed in the 50s of the last century, and in the Soviet Union it became widely used only since 1964 by modification developed in the same year by O.D. Fedorova and G.M. Melnik [1-3]. Despite the fact that the pneumatic cardiodilator has more than half a century of history in the post-Soviet space, the technique remains relevant to this day. After more than half a century, the device of the pneumatic cardiodilator has not undergone much structural changes. The essence of pneumatic cardiodilatation is the forced expansion of the lower esophageal sphincter (LES), which is associated with trauma to the mucous membrane, muscular layer and feeding vessels. Considering that the pressure pumped into the esophagogastric cuff increases from session to session, the risk of complications such as bleeding, severe pain, reflux esophagitis and esophageal perforation increases accordingly with each subsequent session [4-5]. Evaluation of the cardiodilatation efficiency is ambiguous. The results of cardiodilation are evaluated by many authors in different ways. According to D. Katzka, T. Vanuytsel and M. Vela, perforation of the esophageal wall during dilatation is observed in 1-8%, and bleeding from deep mucosal defects in 2-5%, and multiple courses of dilatation can lead to the development interstitial fibrosis, hiatal hernia (HH), traumatic diverticulum [6-8]. Special attention should be paid to the fact that there are no studies in the literature aimed at reducing these complications.Summarizing the mentioned above, it should be noted that the ussies for prevention of minimally invasive treatment methods complications of cardia achalasia are not fully solved at the moment. Aim of the research was to study the effect of infrared pulsed laser radiation and an improved cardiodilator model as methods of preventing complications of cardiodilation in patients with neuromuscular disorders of the esophagus.
2. Material and Methods
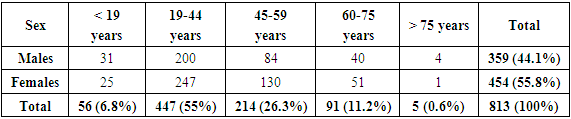
- The Department of the Esophagus and Stomach Surgery of the Republic Specialized Scientific and Practical Medical Center of Surgery named after academician V. Vakhidov has experience in the treatment of 813 patients with neuromuscular disorders of the esophagus who were on treatment in the period from 2010 to 2022. The standard distribution of patients by gender and age according to the WHO classification is presented in Table 1.
|
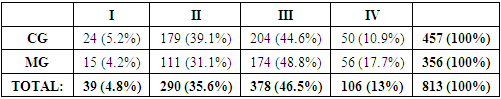
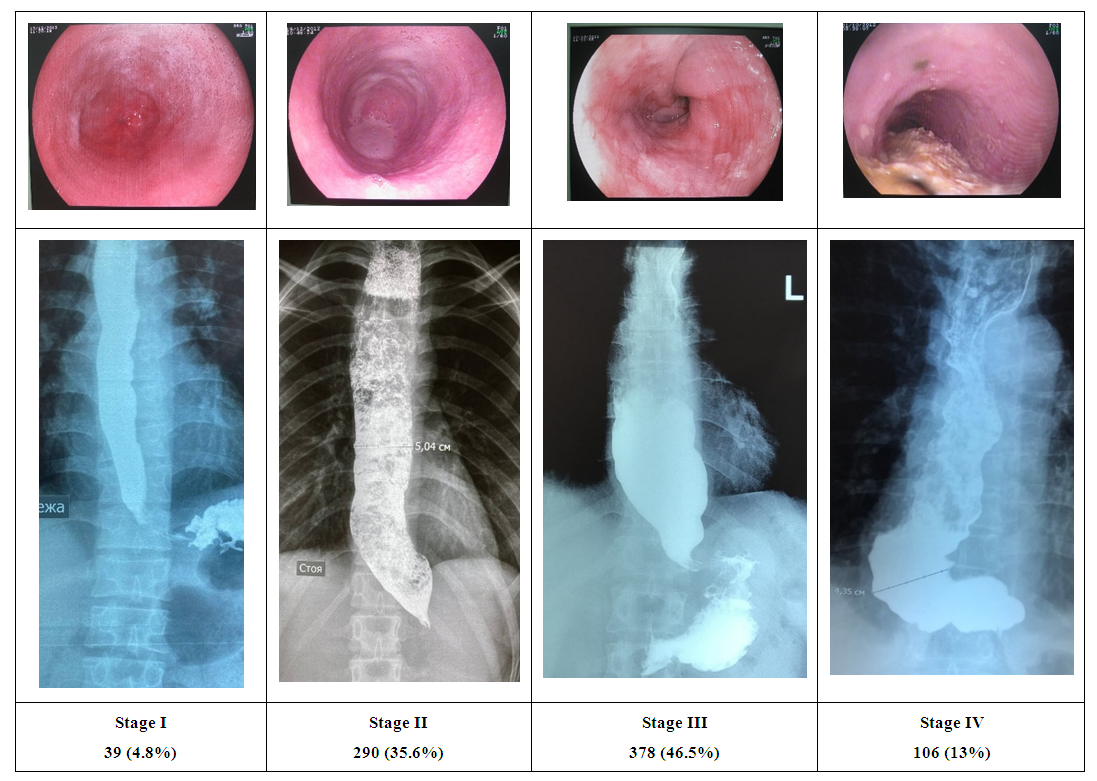 | Figure 1. Stages of the disease according to Petrovsky B.V. |
|
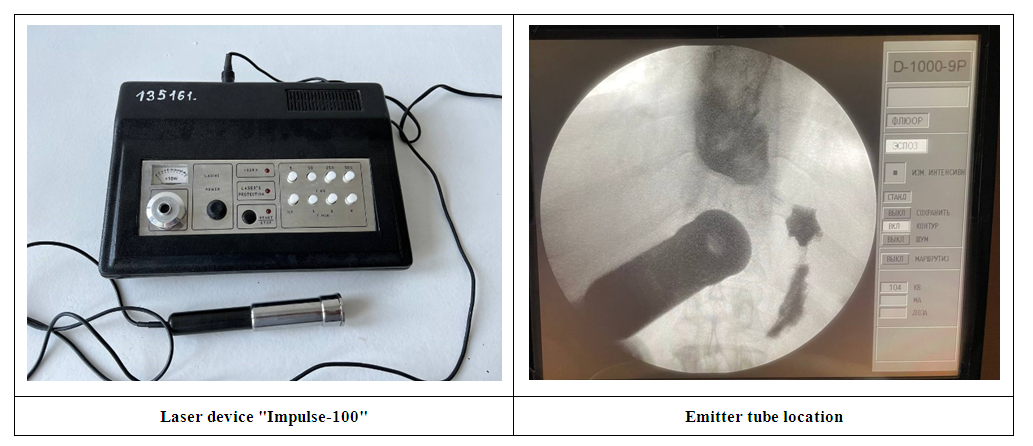 | Figure 2. Laser device and methodology |
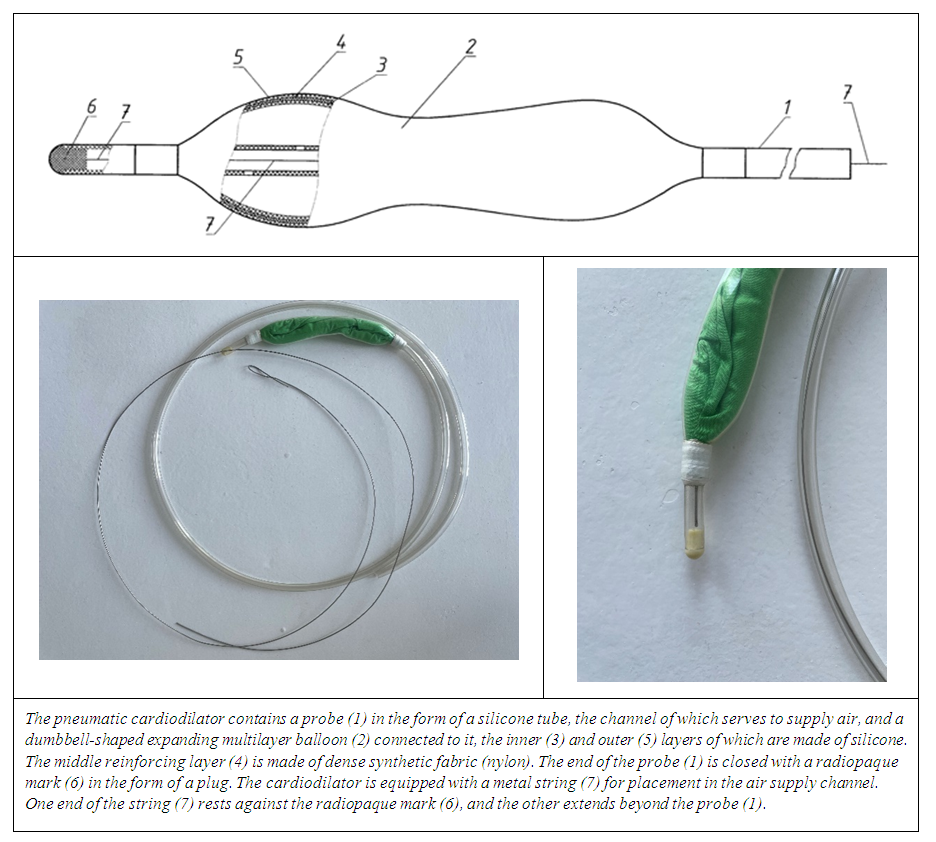 | Figure 3. Utility model “Pneumatic cardiodilator” |
3. Results
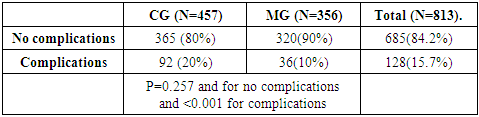
- After dilatation courses, 685 (84.2%) patients had no complications, and 128 (15.7%) patients had various complications. The distribution of patients according to the total number of complications is presented in Table 3.
|
|
4. Discussions
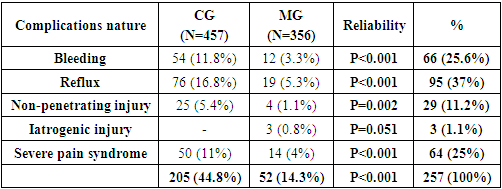
- As the structural analysis of complications in the compared groups showed, in the main group, thanks to the implemented technologies and own developments, it was possible to significantly reduce the number of almost all complications by two or more times. Thus, in the main group, the number of bleedings was observed in 12 (3.3%) patients, while in the comparison group this indicator was noted in 54 (11.8%) patients, and in the main group it decreased to 19 and made up 5.3%. Non-penetrating esophageal injuries in the comparison group were noted in 25 (5.4%) patients, while in the main group this indicator decreased to 4 (1.1%) patients. Iatrogenic injury of the esophagus was observed only in 3 (0.8%) patients of the main group. Pronounced pain syndrome not relieved by non-narcotic analgesics in the comparison group occurred in 50 (11%) patients, in the main group this indicator decreased to 14 (4%) patients.
5. Conclusions
- The use of low-intensity laser radiation in combination with a new model of cardiodilator significantly reduced the total number of complications from 20% to 10%.In the structural analysis of complications, thanks to new technologies and our own developments, a significant reduction in almost all types of complications was also achieved from 44.8% to 14.3%. The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML