-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(10): 1521-1525
doi:10.5923/j.ajmms.20231310.32
Received: Sep. 21, 2023; Accepted: Oct. 9, 2023; Published: Oct. 13, 2023

Evaluation of Graft Survival at Different Periods after Surgery at the Development of Urological Complications
S. S. Kariev, F. R. Nosirov, E. S. Salokhiddinov, F. Y. Yuldashev
Republican Specialized Scientific and Practical Medical Center of Urology, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

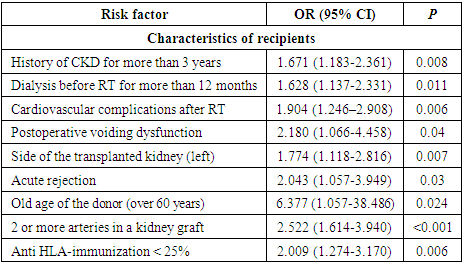
Aim of the study was to evaluate the frequency, risk factors and impact on graft survival associated with urological complications in patients after renal transplantation. Material and methods. The research was based on the examination and treatment results of 162 adult recipients (≥ 18 years) with urological complications after related renal transplantation, who were on outpatient and inpatient treatment at the Republican Specialized Scientific and Practical Medical Center of Urology and at the Republican Specialized Scientific and Practical Medical Center of Surgery named after academician V. Vakhidov for the period from June 2010 to May 2023. The multivariate logistic regression model has been adjusted to identify factors related to urological complications. The survival time of the patient and the transplant was analyzed using the Kaplan-Meyer method. Results. In our cohort of recipients, the donor was elderly (odds ratio (OR) = 6.377, p = 0.024), and had a history of chronic kidney disease of more than 3 years (OR =1.671; р=0.008), dialysis before RT for more than 12 months (OR = 1.628; p = 0.011), cardiovascular complications after RT (OR =1.904; р=0.006), postoperative voiding dysfunction (OR = 2.180; p = 0.04), left-sided RT (OR = 1.774; p = 0.007), acute rejection (OR = 2.043; p = 0.03), more than 2 arteries in the kidney graft (OR = 2.522; p<0.001), anti-HLA immunization <25% (OR =2.009; p=0.006) were predictors of the risk of developing major and minor urologic complications in recipients of a donor kidney. It was revealed that in kidney transplant recipients with urologic complications, in contrast to recipients without urologic complications, a higher incidence of decreased graft function requiring hemodialysis was determined (13.6% versus 11.4%; p = 0.487), however, without a statistical difference and without a significant effect on short-term (92.4% and 94.1% in the group with and without urologic complications, respectively) and long-term (81.0% and 82.7% in the group with and without urologic complications, respectively) kidney transplant survival (log-rank test 0.158, p=0.635). Conclusion. Urologic complications are common complications after related RT. Identification of urologic complications and risk factors may help transplant teams make future surgical and clinical decisions. There are no significant differences in graft survival depending on the presence of urologic complications.
Keywords: Renal transplantation from a living related donor, Major and minor urological complications, Frequency, Structure, Risk factors, Graft survival
Cite this paper: S. S. Kariev, F. R. Nosirov, E. S. Salokhiddinov, F. Y. Yuldashev, Evaluation of Graft Survival at Different Periods after Surgery at the Development of Urological Complications, American Journal of Medicine and Medical Sciences, Vol. 13 No. 10, 2023, pp. 1521-1525. doi: 10.5923/j.ajmms.20231310.32.
1. Introduction
- End-stage chronic renal failure (CRF) is defined as a significant decrease in kidney function, which leads to death in the absence of dialysis or transplantation [1]. The incidence of CRF is more than 1,500 people per million of the population in countries with a high prevalence (such as the USA and Japan). Risk factors for the development of CRF include hypertension, diabetes mellitus, obesity and a history of acute renal failure [2]. About two-thirds of people with CRF receive hemodialysis, a quarter of patients undergo renal transplantation (RT), and one-tenth receive peritoneal dialysis. At the same time, RT is considered superior to chronic dialysis as it prolongs survival and relieves uremic symptoms [3]. Renal transplant recipients are at risk of developing various postoperative complications against the background of receiving immunosuppressive drugs and concomitant pathologies associated with long-term chronic kidney diseases (CKD) [4,5]. Urological complications (UCs) are the second cause of morbidity after RT and rejection episodes, and may be associated with graft loss and mortality [6-9].In patients with chronic renal failure, the life quality is influenced by the disease itself and the treatment option that the patient resorts to. Many factors affecting the life quality of hemodialysis patients have been identified, for example, age, gender, duration of dialysis, family care and support, life status, patient adherence to treatment and level of education [9,10,11]. It is noted that elderly recipients have significantly lower graft survival, as well as a significantly higher risk of graft loss and mortality [12,13]. Life after RT has such negative aspects as a strict regimen of immunosuppressants and related side effects, frequent visits to the doctor, infections, uncertainty and anxiety about rejection episodes, potential transplant loss, lifelong treatment costs and unemployment.It is also important to take into account personal, environmental and clinical factors that negatively affect the life quality associated with health. Life quality evaluation is a useful tool in determining the efficiency of certain therapeutic interventions in patients with chronic diseases, when a complete cure is impossible. [12,13]. Various instruments such as WHOQOL-BREF, KTQ, SF-36, etc. can be used to measure the patient's life quality.The aim of this study was to evaluate the survival of a transplant with urological complications after a related RT.
2. Material and Methods
- The research was based on the examination and treatment results of 162 adult recipients (≥ 18 years) with UCs after related RT, who were on outpatient and inpatient treatment at the Republican Specialized Scientific and Practical Medical Center of Urology and at the Republican Specialized Scientific and Practical Medical Center of Surgery named after academician V. Vakhidov for the period from June 2010 to May 2023. The mean age of recipients with UCs made up 34.5 years (from 20 to 63 years). Young patients (from 18 to 44 years) predominated among the recipients – 84.0% (136 from 162). Middle-aged recipients (from 45 to 59) accounted for 15.4% (25 from 162). Only 1 (0.6%) recipient was elderly. In most cases, surgeries were performed on male recipients – 124 (76.5%) observations.The mean age of donors was 40.4 years (from 18 to 63 years). Young patients (from 18 to 44 years) also prevailed among donors – 62.9% (102 from 162). Middle-aged donors (from 45 to 59 years) made up 34.0% (55 out of 162). Only 5 (3.1%) donors were elderly. Male donors made up slightly more than half (50.6%; 82 from 162) of the cases. Kidney donors were most often first-line relatives - fathers (17.3%), mothers (24.7%), brothers (24.1%) and sisters (21.0%). A significant majority of patients (90.7%; 147 from 162) were operated on for end-stage CKD as a result of chronic glomerulonephritis. In other cases, indications for RT, i.e., the cause led to the terminal stage of CKD, were polycystic kidney disease (2.5%; 4 from 162), chronic pyelonephritis (1.2%; 2 from 162), type 2 diabetes mellitus (0.6%; 1 from 162), various abnormalities of the urinary system (0.6%; 1 from 162). The etiology of CKD was not established in 4 (2.5%) recipients.We conducted a factor analysis by comparing the characteristics of recipients with UCs and their donors with the characteristics of recipients without UCs and their donors. We have identified indicators characterizing both recipients and donors, as well as those associated with the underlying disease (CKD), concomitant pathologies, and features of the course of the early and long-term post transplantation period among potential risk factors. Evaluation of renal transplant survival, as one of the main components of the analysis of the immediate and long-term results of RT, was carried out by constructing the actuarial Kaplan-Meier curve.When calculating the survival rate of a renal transplant, the time from the moment of kidney transplantation to a persistent decrease in graft function requiring hemodialysis or until the patient’s death.
3. Results
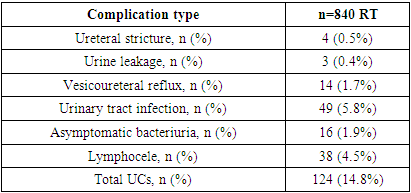
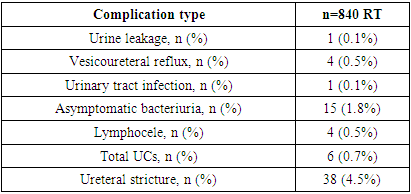
- UCs had a greater occurrence frequency in the early and nearest period after a related RT. In total, the prevalence of UCs after related RT was 19.3% (162 from 840) and it determined them as a significant factor affecting the clinical course of the post transplantation period. The early and immediate period (0-3 months after RT) was characterized by the development of UCs in 14.8% (124 from 840) cases, the frequency of which in the long-term period (more than 3 months after RT) was 4.5% (38 from 840). Urine leakage primarily occurred during the first 3 months (3 (0.4%)) patients. The number of patients with ureteral obstruction after 3 months was 4 (0.5%) and increased up to 7 (0.8%) in the long-term period. Vesicoureteral reflux (VUR) was also more common in the first 3 months after related RT – 1.7% (14 from 840) versus 0.5% (4 from 840) in the long-term period. The incidence of urinary tract infection decreased as the post-transplant period increased from 5.8% (49 of 840) to 1.8% (15 of 840), as did the prevalence of asymptomatic bacteriuria (ASB) (a decrease was noted from 1.9% in early to 0.5% long-term period) (Tables 1 and 2).
|
|
|
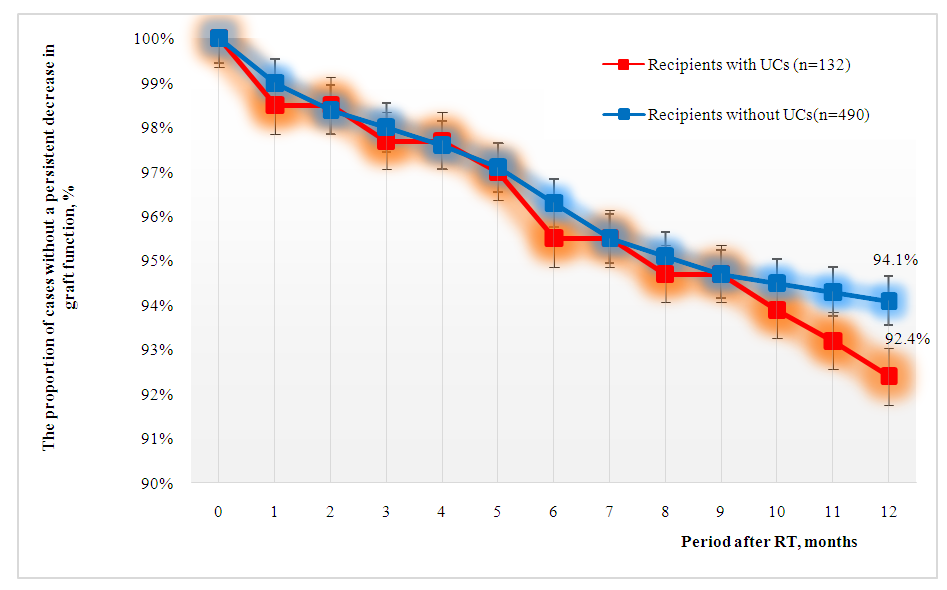 | Figure 1. Evaluation of one-year survival of a kidney transplant depending on the presence of post-transplant UCs |
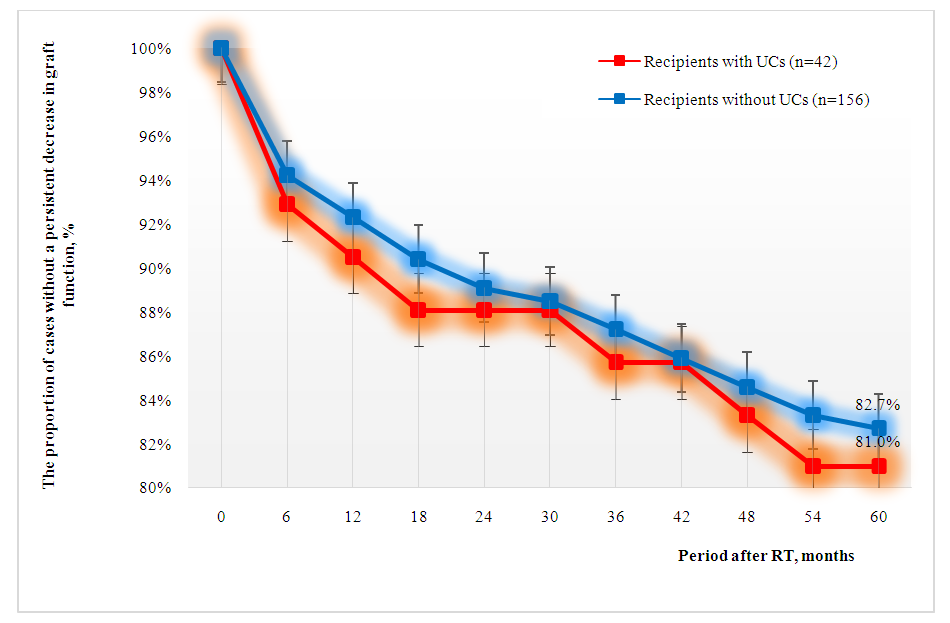 | Figure 2. Evaluation of 5-year survival of a kidney transplant depending on the presence of post-transplant UCs |
4. Conclusions
- UCs are frequent complications of related RT and represent a serious burden for the patient and the healthcare system and may require invasive procedures or repeated surgeries. Reliable predictors of UCs occurrence after related RT were the elderly age of the donor, anamnesis of CKD for more than 3 years, dialysis before RT for more than 12 months, left-sided RT, more than 2 arteries in a kidney transplant, anti-HLA immunization < 25% and early postoperative urinary dysfunction. At the same time, the occurrence of UCs did not significantly affect the survival of the transplant in the short and long term. The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML