Nazyrov F. G., Маkhmudov U. M., Маtkarimov S. U.
State Institution “Republican Specialized Scientific and Practical Medical Center for Surgery Named after Academician V.Vakhidov”
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
To date, the puncture-drainage method is successfully used for evacuation of intra-abdominal pathological exudate accumulations, rehabilitation of postoperative abdominal abscesses. A method for performing puncture-drainage treatment of limited fluid accumulations (LFA) in the abdominal cavity is proposed, aimed at strengthening local adhesive properties and repairing the residual cavity, as well as preventing recurrence. The study included 129 patients with LFA in various parts of the abdominal cavity who underwent puncture-drainage intervention under the control of ultrasound. The main group included 68 patients who underwent minimally invasive treatment according to the proposed method. The comparison group included 61 patients who were treated with LFA according to the standard method of external percutaneous drainage under the control of ultrasound. The overall effectiveness of treatment in the main group increased from 68.9% to 89.7%, and the proportion of recurrence of the development of acute respiratory infections in the abdominal cavity, respectively, was 31.1% and 10.3%, in the structure of which repeated minimally invasive treatment was required in 21.3% of cases in the comparison group and 8.8% in the main group, and open surgical treatment in 9.8% and 1.5%.
Keywords:
Abdominal cavity, Limited fluid accumulations, Puncture-drainage method FarGALS
Cite this paper: Nazyrov F. G., Маkhmudov U. M., Маtkarimov S. U., Improvement of Minimally Invasive Treatment of Limited Fluid Accumulations in the Abdominal Cavity, American Journal of Medicine and Medical Sciences, Vol. 13 No. 10, 2023, pp. 1506-1512. doi: 10.5923/j.ajmms.20231310.30.
1. Relevance of the Research Topic
One of the most frequent complications after abdominal surgery is limited fluid accumulation (LFA) [1,2,3]. Currently, there is an active use of the puncture-drainage method in the treatment of these complications. Thus, puncture aspiration and percutaneous drainage of nonparasitic cysts and liver abscesses is considered the preferred intervention [4,5]. The puncture-drainage method is successfully used for evacuation of intra-abdominal pathological accumulations of exudate, rehabilitation of postoperative abscesses of the abdominal cavity [6,7,8,9,10,11].The advantages of minimally invasive methods of treatment in comparison with traditional surgical interventions include low traumatism, low postoperative mortality, no risk of general anesthesia, reduction of the patient's hospital stay [8,12]. The occurrence of limited fluid accumulations in the early postoperative period in most cases is the result of a combination of several general and local factors and depends in particular on the type and volume of surgery, the patient's age, the level of his preparation for surgery, the presence of concomitant pathology [13]. The main method of treatment of limited fluid accumulations is considered by most surgeons to be minimally invasive interventions under ultrasound or CT control [8].Of great importance for the effectiveness of ultrasound puncture drainage of intra-abdominal abscesses is not only the correct implementation of this intervention, but also the subsequent management of the patient [10]. The accumulation of practical experience in puncture drainage under ultrasound guidance makes it possible to successfully heal ulcers previously available only for traditional, "open" autopsy [2,11]. For the treatment of intraperitoneal abscesses, the choice of surgical correction method depends on the method of verification of the abscess during ultrasound, laparoscopy; localization of purulent accumulation: adheres to the wound, in the pelvic cavity, subhepatic, interstitial; the complexity of the configuration of the abscess: single or multiple cavities, ulcers of several localizations [1].The choice of the nature of percutaneous intervention is influenced by the distance to the LFA, the complexity of the trajectory of the instrument, the intended nature of the contents. The more complicated the trajectory, the more preference is given to puncture. However, one of the defining selection criteria is the size of the LFA (maximum size and integral indicator - volume). All liquid accumulations are divided into: small (up to 2 cm, volume up to 10 ml), medium (2-4 cm, volume 11-80 ml), large (4-8 cm, volume 81-600 ml) and giant (over 8 cm, volume more than 600 ml) [2,10].However, despite the advantage of percutaneous interventions in the treatment of LFA, the results of these operations do not always satisfy surgeons. The disadvantage of the method is the need for long-term wearing of drainage, which depends on the reasons supporting the cavity and its size. This is primarily due to the difficulties of carrying out high-quality sanitation of the cavity of limited fluid accumulations / abscess and adequate antibacterial therapy. The cavity of the abscess from the inside can be covered with a dense layer of fibrinous overlays and purulent-necrotic masses, which are a nutrient substrate for bacteria, interfere with the action of drugs and reduce the effectiveness of treatment. Often, after such interventions, relapses occur, which require repeated manipulations up to open operations.Thus, the task is to increase the effectiveness of puncture-drainage treatment of LFA in the abdominal cavity, prevention of recurrence, as well as strengthening local adhesive properties and repair of the residual cavity.
2. Material and Methods of Research
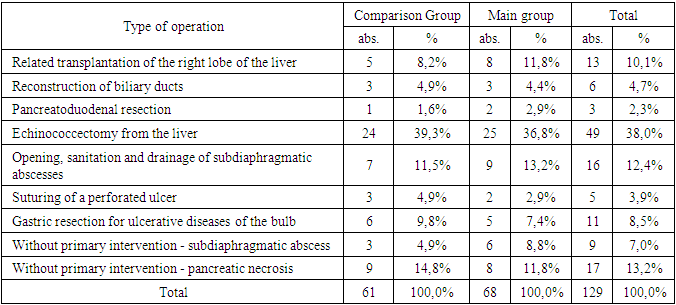
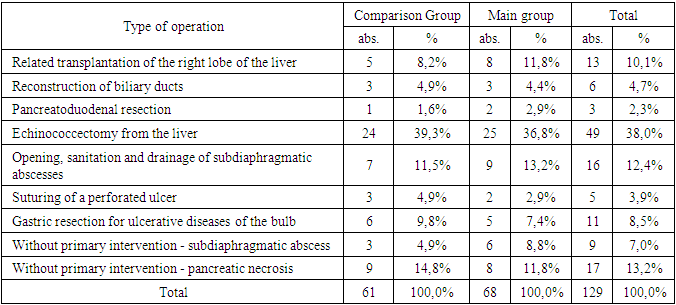
The study is based on the development of a new method of puncture-drainage treatment of LFA in the abdominal cavity. The study included 129 patients with LFA in various parts of the abdominal cavity who underwent puncture-drainage intervention under ultrasound control for the period from 2020 to September 2023. The material was accumulated in the State Institution "Republican Specialized Scientific and Practical Medical Center for Surgery named after Academician V. Vakhidov" - 96 patients and the clinic of the Andijan State Medical Institute - 33 patients. All patients were divided into 2 groups. The main group included 68 patients (2022-2023) who underwent minimally invasive treatment according to the proposed method. The comparison group included 61 patients (2020-2021) who were treated with LFA according to the standard method of external percutaneous drainage under the control of ultrasound. The distribution of patients due to the development of LFA in the abdominal cavity is presented in Table 1.Table 1. Types of primary operations complicated by the development of LFA
 |
| |
|
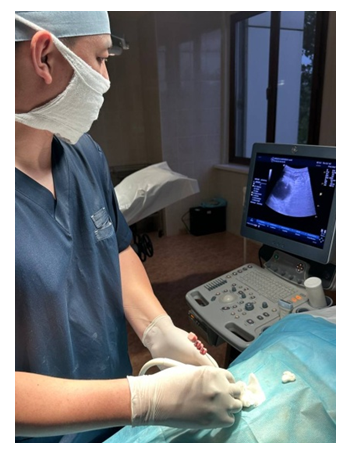
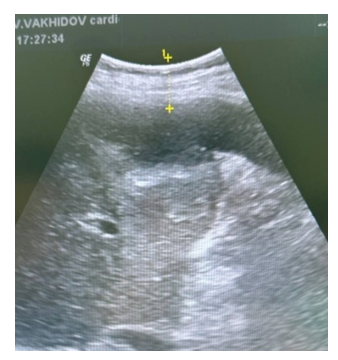
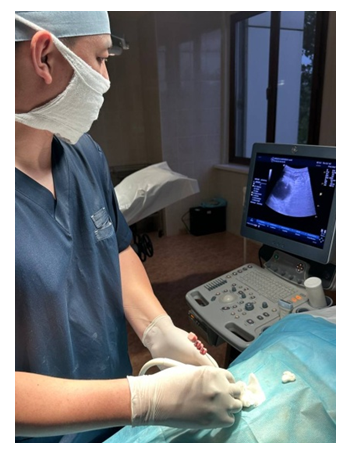
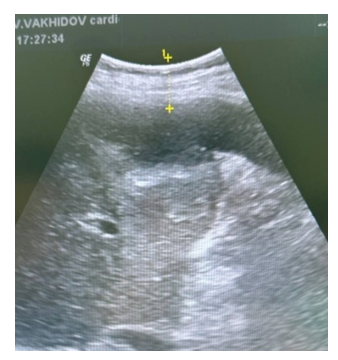
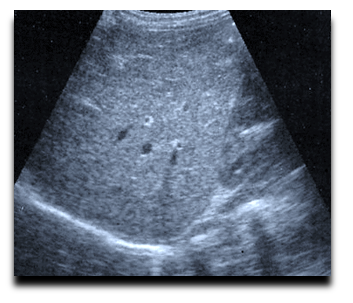
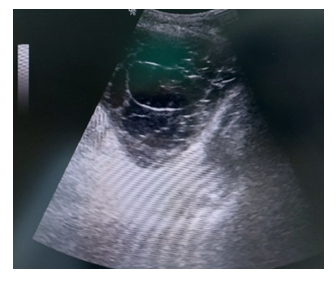
Among the studied main group there were 39 women (57.4%), 29 men (42.6%). The age of the patients ranged from 16 to 74 years and averaged 50.7 ± 1.3 years. In the comparison group, there were 25 men (41.0%), 36 women (59.0%). The average age was 45.4 ± 1.2 years.In both groups, the largest number of patients were with LFA localization in the subdiaphragmatic and subhepatic regions. This once again confirms that previously performed operations in most cases were performed on organs of the hepatopancreatobiliary zone. Thus, localization of LFA subdiaphragmal was noted in 45 cases (in 21 and 24 patients of both groups), subhepatic in 33 cases (in 16 and 17 patients, respectively). Further, the number of patients with LFA localization was noted in the epigastric region – 25 (13 and 12 cases, respectively.During ultrasound, the approximate volume of LFA was determined in milliliters. Thus, LFA with a volume of 200-300 ml was diagnosed in 41% (25 patients) in the compared group and 35.3% of cases in the main group. LFA volume of 300-500 ml in 26.2% (n=16) and 30.9% (n=21) of observations, respectively. The LFA volume of more than 500 ml was established in 25 observations of both groups, respectively.The nature of the fluid obtained during puncture-drainage intervention in most cases (47% and 50%, respectively) was infected in the form of purulent fluid, as well as accumulation of serous exudate in 29.5% and 23.5% of observations, respectively. Pathogenic flora in the form of Escherichia coli was most often present according to the results of seeding – 19 (31.1%) and 21 (30.9%, respectively, and Staphylococcus s.p. in 16 (26.2%) and 18 (26.5%) patients. Sterile discharge was found in 15 patients in the comparison group and 16 in the main group.LFA drainage was performed in the operating room under local or general anesthesia. Local anesthesia was performed with a 0.25% novocaine solution. Total intravenous anesthesia was used for general anesthesia. Ultrasound control during manipulation was carried out by a LOGIQ G6/P6 Pro device (GE Healthcare, Milwaukee, Wisconsin 53201 U.S.A) with a convexic sensor for transabdominal scanning C 3-7D with a variable frequency of 3-7 MHz. During the diagnostic puncture, the shortest access point to the LFA was selected. For surface LFA, large–caliber needles were used - up to 14 G, and for deeply located thinner ones - 20 G. When performing puncture-drainage intervention for LFA, stiletto catheters of the "pig tail" type of caliber 4 – 12 Fr, direct trocar catheters of caliber 8 – 28 Fr Ingram (Cook, U.S.A.) were used.The punctate is sent for bacteriological examination and determination of sensitivity to antibiotics, for cytology if a tumor is suspected, and for biochemical analysis for the content of amylase or bilirubin.In large-diameter LFA, a two-catheter drainage technique was used using large (from 20 to 32 Fr) and small (from 8 to 10 Fr) caliber catheters in order to ensure flow sanitation of the infected focus, the main condition of which is free outflow from the cavity.Technical aspects of the method of puncture-drainage treatment of limited fluid accumulations in the abdominal cavity:• a puncture of the fluid accumulation is performed under the control of ultrasound (the resulting punctate is sent for bacteriological examination to determine the type of pathogen and its sensitivity to antibacterial agents);• further, a two-channel drainage is carried out along the conductor string into the residual cavity for subsequent washing of the residual cavity with FarGALS antiseptic in 50% concentration (50 ml of FarGALS is diluted with 50 ml of sterile water for injection in a ratio of 1:1);• the resulting solution is drip-injected into the residual cavity through drainage at a rate of 15-20 drops per minute for 60 minutes (total volume of 100 ml per wash);• such washing is carried out 3 times a day for 2 days (Fig. 1-4);• at the same time, after washing, vacuum aspiration is installed on the drainage by using a vacuum device of the "Redon" type, the capacity of which creates a vacuum in the residual cavity of 70-100 kPa;• from the same period, the residual cavity is irradiated with laser radiation of the Matrix apparatus using a laser emitting head KL-VLOK-365 (КЛ-ВЛОК-365), providing a wavelength of 365-400 nm, with a power of 3 MW, for 2 minutes per volume of 1 cm3 using a light guide with radiation at an angle of 90-120° with a frequency of 1 time per day (on average 2-3 sessions);• drainage is removed after a clear verification of the fall of the residual cavity and the absence of a pathological discharge or the presence of a serous discharge of up to 20 ml;• at the same time, if, after removing the vacuum, a recurrence of liquid accumulation is determined on ultrasound, then this procedure is repeated again. | Figure 1. Ultrasound |
 | Figure 2. Stage of puncture under the control of ultrasound needle "Chiba" |
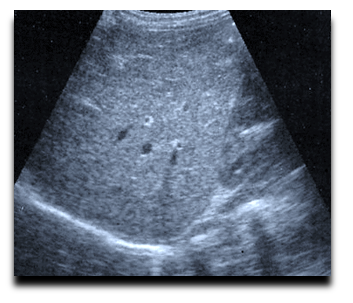
 | Figure 3. In dynamics |
 | Figure 4. After drainage removal |
Rinsing the residual cavity with FarGALS solution provides an antibacterial and antiseptic effect, and the addition of the procedure with intraluminal laser irradiation contributes both to an additional antiseptic effect and leads to a photodynamic effect of the FarGALS solution, which generally provides enhanced local adhesive properties and repair of the residual cavity (Fig. 5-6).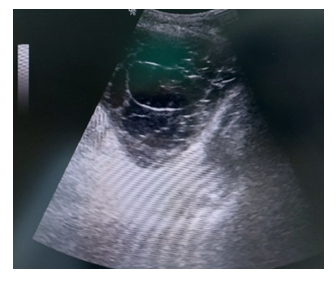 | Figure 5. Puncture under ultrasound control |
 | Figure 6. After the elimination of the hearth |
The advantages of the claimed method are the following criteria: • washing with FarGALS solution provides an adequate antibacterial effect due to a wide antimicrobial spectrum;• the solution has an anti-inflammatory effect, which will contribute to the rapid purification of the cavity from pathological impurities, as well as ensure the cessation of production into the cavity of the liquid component;• the proven property of FarGALS is the activation of reparative processes, which will accelerate the obliteration of the residual cavity;• direct exposure to laser radiation in the infrared spectrum on the residual cavity through drainage also has an anti-inflammatory and regenerative effect;• the combined use of a laser and a FarGALS provides an enhancement of the effect of the latter due to the presence of photodynamic properties of the drug.Patent for the invention of the Ministry of Justice of the Republic of Uzbekistan No. IAP 07422 dated May 31, 2023 ("Method of puncture-drainage treatment of limited fluid accumulations in the abdominal cavity") was obtained for this method.
3. Results and Discussion
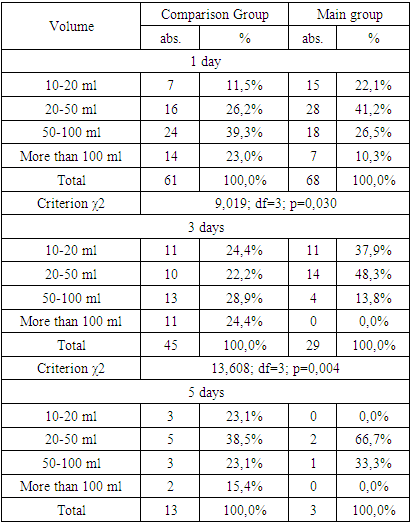
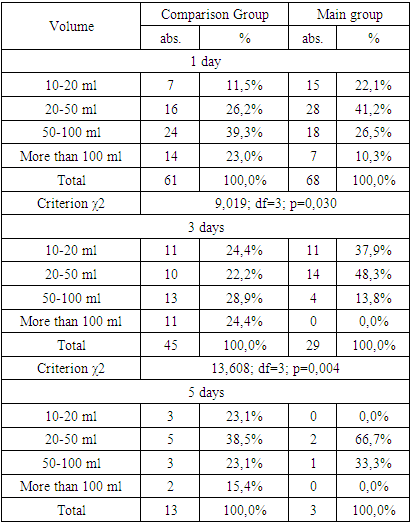
The conducted studies allowed to substantiate the effectiveness of minimally invasive treatment of LFA with the washing of the residual cavity with the antiseptic agent FarGALS and its direct irradiation with laser radiation of the Matrix apparatus. These two factors determine the pathogenetic therapeutic effect, which can be characterized by the following advantages. Firstly, taking into account the possible infection of the LFA contents, seeding with the determination of the type of microflora and its sensitivity to antibacterial drugs, which takes at least 1-3 days, washing with FarGALS solution, which has a wide antimicrobial spectrum, is pathogenetically justified, since there is a direct effect on the residual cavity. Secondly, the solution itself has an anti-inflammatory effect, promotes rapid purification of the cavity from pathological impurities, and also ensures the cessation of production or the release of a liquid component into the cavity. Thirdly, FarGALS treatment promotes the activation of reparative processes and closure of the residual cavity. Fourth, the direct effect of laser radiation in the infrared spectrum on the residual cavity through drainage also has an anti-inflammatory and regenerative effect. Fifth, the combined use of a laser and a FarGALS provides an enhancement of the effect of the latter due to the presence of photodynamic properties of the drug. All these factors have a definite advantage in the treatment of LFA. This applies not only to drainage interventions, but also to standard puncture manipulations, when the fluid obtained from LFA has a serous character without pathological impurities and can be limited only to its evacuation. In these cases, a single performance of washing with FarGALS solution and laser irradiation through a puncture needle will also contribute to rapid obliteration of the cavity with a reduction in the risk of recurrence of congestion.Analysis of the course after minimally invasive intervention showed that standard approaches allowed to limit the drainage time to 2-3 days only in 16 (26.2%) patients of the comparison group, while the use of a new technique in the main group allowed to increase this indicator to 57.4% (in 39 of 68 patients).Within 4-5 days after the intervention, drains were removed in 32 (52.5%) and 26 (38.2%) patients, respectively. On the 6th-8th day, 9 (14.8%) and 3 (4.4%) patients had more. In the comparison group, 4 (6.6%) patients required longer drainage – 9-10 days or more. In terms of drainage timing, a significant positive difference was obtained in the main group (χ2=16,909; df=3; p<0.001).After evacuation of the LFA contents, the volume of discharge ranged from 10 to 300 ml, while during the first day the minimum discharge (10-20 ml) was only in 7 (11.5%) patients in the comparison group and 15 (22.1%) in the main group (Table 2).Table 2. Volume of discharge by drainage
 |
| |
|
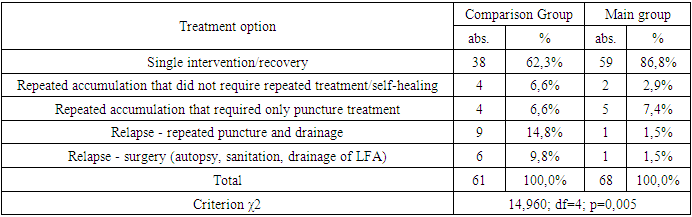
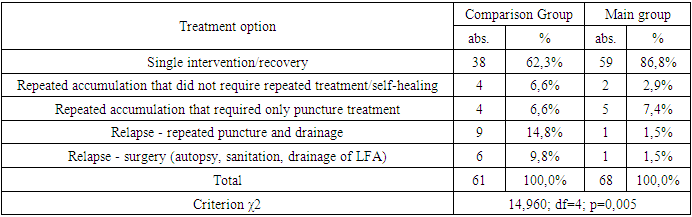
Local impact on the residual cavity in patients in the main group provided a decrease in the volume of discharge. So, a day after drainage with therapeutic sessions, the volume of discharge was 54.6 ±45.1 ml/day, whereas in the comparison group it was 90.9±73.9 ml (t=3.32; p<0.05). On day 3, the average values were 33.3±20.8 and 74.2±54.5 ml (t=4.55; p<0.05), and on day 5, 35.0±17.3 versus 60.0±46.9 ml.The therapeutic effect of local LFA treatment was also characterized by a faster regression of the temperature reaction. Thus, out of 49 patients admitted with hyperthermia, the temperature returned to normal on 1-2 days in 32 (65.3%) patients, whereas in the comparison group in 19 of 42 (45.2%). By day 3, the daily temperature was within the normal range in 14 (28.6%) and 11 (26.2%) patients, by day 5 in 3 (6.1%) and 8 (19.0%) patients, respectively, in 4 more (9.5%) cases in the comparison group, longer treatment was required (χ2=9.464; df=3; p=0.024).The leukocyte level at the time of minimally invasive LFA treatment was 11.1±1.9 x 109 in the comparison group and 11.3±1.7 x 109 in the main group. During the day, these indicators decreased slightly, but were significantly indistinguishable - 10.4±1.8 and 9.9±1.4 x 109, respectively, on day 3, the indicators were already significantly different and were less in the main group - 10.2±1.4 versus 9.3±0.7 x 109 (t=3.63; p <0.05), a similar picture was It was also obtained among patients continuing treatment on day 5 - 9.5± 1.3 versus 8.3±0.8 x 109 (t=3.59; p<0.05).Among other markers of inflammation, the dynamics of the level of C-reactive protein and procalcitonin were traced. The C-reactive protein index (norm up to 5 mg/l) at the time of treatment of LFA was 45.0±14.1 mg/l in the comparison group and 45.9±13.5 mg/l in the main group. During the day, these indicators decreased and were significantly distinguishable – 39.3±14.2 and 32.2±13.4 mg/l, respectively (t=2.91; p<0.05), on day 3, the difference increased even more – 33.0±11.3 versus 27.2±4.6 mg/l (t=3.21; p<0.05), and on day 5, the C-reactive protein index was 28.8±5.2 versus 18.7±4.1 mg/l (t=6.34; p<0.05).The procalcitonin index (norm up to 0.5 ng/ml) at the time of minimally invasive LFA treatment was 9.8±5.9 ng/ml in the comparison group and 9.4±6.2 ng/ml in the main group. During the day, these indicators decreased and were significantly distinguishable – 8.4±5.8 and 6.1±4.2 ng/ml, respectively (t=2.62; p<0.05), on day 3, the difference also increased even more – 7.1±5.1 vs. 4.6±3.3 ng/ml (t=2.76; p<0.05), and on day 5, the procalcitonin index was 6.2±4.9 versus 2.4±1.6 ng/ml (t=3.52; p<0.05). A rapid clinical effect with early drainage removal allowed 14 (23.0%) patients in the comparison group and 31 (45.6%) patients in the main group to be discharged for outpatient observation on day 3. On day 4-5, 20 (32.8%) and 26 (38.2%) patients were discharged, respectively. Longer hospitalization was required in the main group of 8 (11.8% - on 6-7 days) and 3 (4.4% - on 8-10 days) patients. In the comparison group, 14 (23,050 patients were discharged on 6-7 days, 9 (14.8%) on 810 days and 4 (6.6%) after 10 or more days. According to this criterion, a significant difference was also obtained due to a faster clinical effect from the treatment in the main group (χ2=15,507; df=4; p=0.004).In general, the evaluation of the effectiveness of the undertaken minimally invasive LFA treatment showed that in the comparison group the average drainage time was 4.7±2.0 days, and in the main group 3.4±1.3 days (t=4.32; p<0.05).Taking into account the results obtained, the following can be noted. One-time drainage of the OHS with a favorable outcome was achieved in 38 (62.3%) patients in the comparison group and 59 (86.9%) patients in the main group. At various times after primary drainage, repeated accumulation on ultrasound, which regressed without the need for minimally invasive treatment, was detected in 4 (6.6%) and 2 (2.9%) patients. In turn, repeated accumulation, requiring only puncture treatment, was noted in 4 (6.6%) and 5 (7.4%). In these cases, the volume of accumulation exceeded 100 ml, but serous discharge was obtained during puncture, and the residual cavity subsided well, and therefore the manipulation was limited to puncture (Table 3).Table 3. Outcome of minimally invasive LFA treatment
 |
| |
|
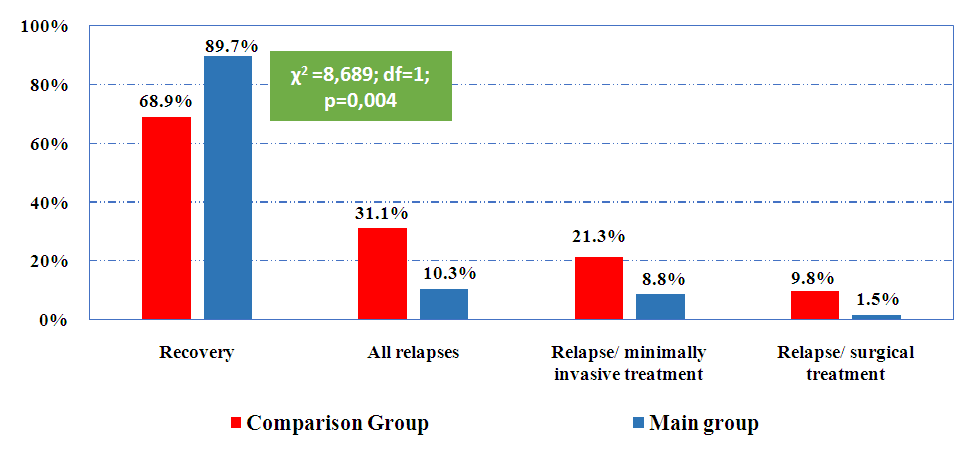
Relapsing course with the need for re-drainage was in 9 (14.8%) patients in the comparison group and only 1 (1.5%) in the main group. These patients underwent repeated drainage with a favorable outcome. In 6 (9.8%) cases in the comparison group and 1 (1.5%) case in the main group, minimally invasive treatment was ineffective. During repeated examination on ultrasound and MSCT, the LFA was more diffuse, while repeated drainage was unsuccessful due to irregularly shaped and complex foci with the presence of non-drained zones, additional drainage of which was impossible due to lack of access. The progress of clinical symptoms required performing open interventions in these patients with autopsy, sanitation and drainage of LFA. In all cases, these clusters were initially with purulent contents, and 3 had a suppurated hematoma. According to the outcomes of minimally invasive treatment, taking into account the distribution of patients according to the need for repeated minimally invasive or open interventions, a significant difference with higher efficacy was obtained among patients in the main group (χ2=14.960; df=4; p=0.005).In terms of 7-14 days after primary treatment, a relapse of acute respiratory failure developed in 4 (6.6%) patients in the comparison group and 1 (1.5%) in the main group, after 14-28 days in 7 (11.5%) and 4 (5.9%) patients, respectively, in terms of more than 28 days in 8 (13.1% and 2 (2.9%) patients.In general, the outcome of treatment with recovery was noted in 42 (68.9%) patients in the comparison group and 61 (89.7%) patients in the main group. The recurrence rate was 31.1% (19 patients) versus 10.3% (7 patients) (χ2=8,689; df=1; p=0.004), of which 13 (21.3%) complications were minimally eliminated in the comparison group and 6 (8.8%) in the main group, with open surgical access in 6 (9.8%) and 1 (1.5%) patients (Fig. 7).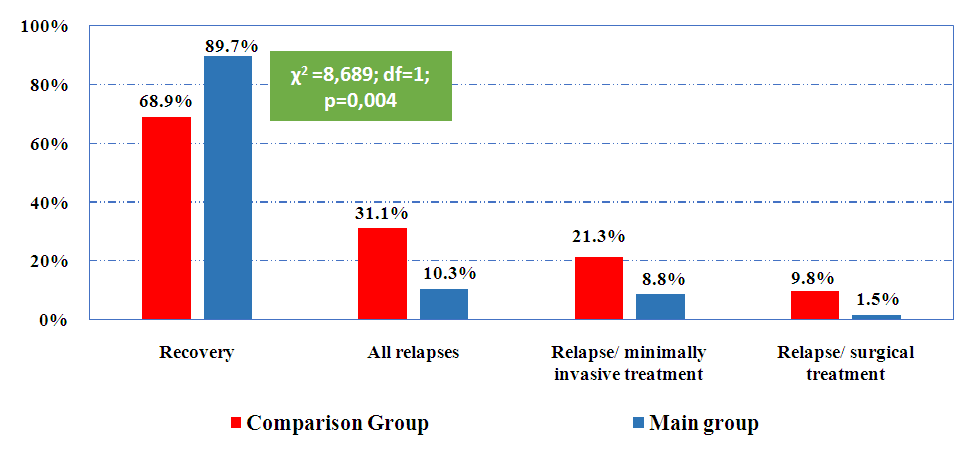 | Figure 7. Distribution of patients by LFA treatment outcomes |
Summary treatment results were distributed by outcome. Good results were attributed only to cases with effective primary intervention, with regression according to ultrasound of the residual cavity without repeated accumulation. Satisfactory results included cases with repeated accumulation, which was either independently resolved or eliminated by repeated minimally invasive treatment. Unsatisfactory results were considered in which there was a need to perform open surgical treatment.If we consider the entire cohort of patients, then in the comparison group, good results were obtained in 38 (62.3%) patients, and in the main group in 59 (86.8%). Satisfactory results were 17 (27.9%) and 8 (11.8%) cases, respectively. Unsatisfactory results were found in 6 (9.8%) and 1 (1.5%) patients (χ2=11,010; df=2; p=0,005).Summary results of minimally invasive treatment of infected LFA showed that in the comparison group, good results were obtained in 27 out of 46 (58.7%) patients, and in the main group in 44 out of 52 (84.6%) patients. Satisfactory results were 13 (28.3%) and 7 (13.5%) cases, respectively. Unsatisfactory results were found in 6 (13.0%) and 1 (1.9%) patients (χ2= 9.109; df=2; p=0,011).Summary results of minimally invasive treatment of sterile LFA showed that in the comparison group, good results were obtained in 11 out of 15 (73.3%) patients, and in the main group in 15 out of 16 (93.8%) patients. Satisfactory results were 4 (26.7%) and 1 (6.3%) cases, respectively. There were no unsatisfactory results in this sample (χ2= 2,386; df=1; p=0,123).
4. Conclusions
The introduction into clinical practice of a new method of treatment of LFA of the abdominal cavity allowed us to draw the following conclusion:Conducting minimally invasive LFA treatment in the abdominal cavity with washing of the residual cavity with FarGALS antiseptic and direct exposure to laser radiation accelerated the regression of hyperthermia from 3.1±1.7 to 2.1±1.0 days (t=3.45; p<0.05), reducing the average drainage time from 4.7±2.0 to 3.4±1.3 days (t=4.32; p<0.05), as well as the period of the rehabilitation hospital stage after drainage intervention from 5.7±2.8 to 4.0±1.7 days (t=4.21; p<0.05).A more rapid decrease in the activity of inflammatory markers was noted in the main group, in particular, the regression of the leukocyte level by 3 days was from 11.3±1.7 to 9.3±0.7 x 109, and in the comparison group from 11.1±1.9 to 10.2±1.4 x 109 (between groups - t=3.63; p<0.05), the indicator After a day, the C-reactive protein decreased 45.9±13.5 to 32.2±13.4 mg/l and from 45.0±14.1 to 39.3±14.2 mg/l, respectively (between groups - t=2.91; p<0.05), and the value of procalcitonin during this period decreased from 9.4±6.2 to 6.1±4.2 ng/ml and c in the comparison group from 9.8±5.9 only to 8.4±5.8 ng/ml (between groups - t=2.62; p<0.05), which characterizes a significantly higher clinical efficacy of local exposure to the residual cavity during minimally invasive treatment of LFS according to the proposed method. The combined use of the drug FarGALS and laser radiation in the minimally invasive treatment of LFA in the abdominal cavity, providing a cumulative effect of two interrelated pathogenetic physico-chemical factors, allowed to improve the proportion of good results from 62.3% to 86.8%, while the frequency of satisfactory results was 27.9% and 11.8%, and unsatisfactory – 9.8% and 1.5% (χ2=11,010; df=2; p=0,005).In turn, the overall effectiveness of treatment in the main group increased from 68.9% to 89.7%, and the proportion of recurrence of acute respiratory infections in the abdominal cavity, respectively, was 31.1% and 10.3% (χ2=8.689; df=1; p=0.004), in the structure of which repeated minimally invasive treatment was required in 21.3% of cases in the comparison group and 8.8% in the main group, and open surgical treatment in 9.8% and 1.5% (by factors: recovery, repeated minimally invasive treatment and repeated open intervention: χ2=9,303; df=2; p=0,010).
References
| [1] | Borodin, M.A. Minimally invasive interventions under ultrasound guidance in patients with diseases of the abdominal cavity and retroperitoneal space / М.А. M.A. Borodin, D.M. Krasilnikov, I.V. Zainullina // Endoskopicheskaya hirurgiya, 2006. – No 2. – pp. 11–20. (In Russ.). |
| [2] | Zhebrovskiy, V.V. Early and late postoperative complications in abdominal surgery / V.V. Zhebrovskiy. – Simferopol': Izdatel'skix centr KGMU, 2000. – P. 688. (In Russ.). |
| [3] | Bagi, P. Percutaneous drainage of appendiceal abscesses / P. Bagi, S. Dueholm, S. Karlstrup // Dis. Colon. Rectum, 1987. – V.30. N7. – P.532–535. |
| [4] | Alonceva, N.N. The role of laparoscopy in the diagnosis and treatment of early postoperative complications / N.N. Alonceva, V.Е. Sobolev, I.P. Dudanov // Vestnik hirurgii im. I.I. Grekova. – 2005. – V. 164. – No1. – pp. 95–99. (In Russ.). |
| [5] | Bertleff, M. Laparoscopic correction of perforated peptic ulcer: First choice. A review of the literature / M. Bertleff, J. Lange // Surg. Endosc. – 2010. – Vol. 24. – P. 1231–1239. |
| [6] | Diagnosis and treatment of postoperative intra-abdominal complications / A.G. Kriger, B.K. Shurkalin, P.S. Glushkov, I.L. Andrejcev // Hirurgiya. – 2003. – No3. – pp. 19–23. (In Russ.). |
| [7] | Zhebrovskiy, V.V. Complications in abdominal surgery: A Guide for doctors / V.V. Zhebrovskiy. – М.: ООО «Medicinskoe informacionnoe agenstvo», 2006. – P. 448. (In Russ.). |
| [8] | Bertleff, M. Laparoscopic correction of perforated peptic ulcer: First choice. A review of the literature / M. Bertleff, J. Lange // Surg. Endosc. – 2010. – Vol. 24. – pp. 1231–1239. |
| [9] | Brolin, R.E. Percutaneous catheter versus open surgical drainage in the treatment of abdominal abscesses / R.E. Brolin, J.L. Nosher, S. Leiman // Amer. J. Surg., 1984. – V. 50. – pp. 102–108. |
| [10] | Zaporozhets, A.A. Physical and biologic impermeability of intestinal sutures in the first twenty-four hours after operations on the gastrointestinal tract / A.A. Zaporozhets // Surgery. – 1992. – №112(5). – pp. 940–945. |
| [11] | Yakubov FR, Sapaev DS. Surgical treatment of liver echinococcosis. J Med Life. 2022 Nov; 15(11): 1409-1414. doi: 10.25122/jml-2022-0268. PMID: 36567844; PMCID: PMC9762364. |
| [12] | Glabay, V.P. Relaparotomy in abdominal surgery / V.P. Glabay, А.I. Sharov, А.V. Arharov // Sbornik trudov mezhdunarodnogo hirurgicheskogo kongressa. – Rostov-na-Donu. – 2005. – P. 117. (In Russ.). |
| [13] | Schein, M. Schein´s Common Sense Emergence Abdominal Surgery. Zdravyj smysl v neotlozhnoj abdominal'noj hirurgii. Per. s angl. – M. Gjeotar-Med. 2003. – P. 272. (In Russ.). |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML