-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(10): 1502-1505
doi:10.5923/j.ajmms.20231310.29
Received: Sep. 19, 2023; Accepted: Oct. 9, 2023; Published: Oct. 11, 2023

Study of the Effect of COVID-19 Infection on Thyroid Tissue in Adult Patients with Type 1 Diabetes Mellitus
Abdulazizkhozhieva R. B.1, Alimova N. U.2
1Fergana Public Health Medical Institute, Uzbekistan
2Republican Specialized Scientific and Practical, Medical Center of Endocrinology, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article under discussion studied the effect of COVID-19 infection on thyroid tissue and its functional status with type 1 diabetes mellitus in adults with and without a history of COVID-19 infection. According to the results, 45 patients with COVID-19 infection had increased thyroid size compared with 35 patients who did not have COVID-19 infection, the number of enlarged degree III goiter increased by 34%, and degree IV goiter increased by 2%. The analysis found that patients with COVID-19 infection in group 1 had forms of multinodular goiter, and no forms of multinodular goiter occurred in patients without COVID-19 infection.
Keywords: Coronavirus infection, COVID-19, Thyroid gland, Thyroiditis
Cite this paper: Abdulazizkhozhieva R. B., Alimova N. U., Study of the Effect of COVID-19 Infection on Thyroid Tissue in Adult Patients with Type 1 Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 13 No. 10, 2023, pp. 1502-1505. doi: 10.5923/j.ajmms.20231310.29.
Article Outline
1. The Relevance of the Research Topic
- According to the World Health Organisation (WHO) data for 2020, Convid-19 has spread very rapidly around the world and reached pandemic level, becoming a global problem for all countries [13]. Numerous clinical observations show that in patients with comorbidities this disease is more severe. Especially in people with diabetes, this infection was severe and led to serious complications. It affected not only the respiratory system, but also all the cells of the body as a whole. Thyroid dysfunction in diabetic patients, both in the acute phase of Covid-19 infection and in the recovery phase after Covid-19 has been shown in several literatures [7]. According to most authors, thyroid dysfunction caused by patients with Covid-19 is influenced by the "cytokine storm" that causes autoimmune thyroid diseases [18] and exacerbated Greaves' disease [2].In patients with thyroid diseases changes in the immune system, immunodeficiency are known from the very beginning [9]. For this reason, these patients have a higher incidence of Covid-19 infection and a more severe course of infection. In our region in Andijan province, iodine deficiency has been confirmed in a number of scientific papers [10], this deficiency will inevitably have its own characteristics in patients with Covid-19, especially in diabetic patients. In particular, since type 1 diabetes is an autoimmune disease, it has been shown in scientific studies that such patients very often develop thyroid disease.Also, scientific studies on the association of COVID-19 infection with thyroid disease that develops in diabetic patients have not been sufficiently conducted worldwide. Therefore, the study of thyroid function after Covid-19 infection in Andijan region, which is an iodine deficiency zone, is of great importance. More knowledge and scientific studies on this subject are needed to develop recommendations for effective treatment and clinical management of these diseases. Considering the above, the study of thyroid changes in elderly patients with type 1 diabetes mellitus caused by Covid-19 infection has been recognised as one of the urgent medical issues in our region, especially in Andijan region.
2. The Aim of the Research
- To evaluate the effect of COVID-19 infection on thyroid tissue by ultrasound and on hormonal background in elderly patients with type 1 diabetes mellitus living in Andijan region.
3. Objects and Methods of the Research
- 80 adult patients with type 1 diabetes mellitus who applied to the regional endocrinological dispensary in 2020-2022 living in Andijan region were analysed. Among the examined patients, 39 (49%) were females and 41 (51%) were males, whose age ranged from 18 to 48 years.The medical histories of the patients were studied in detail. Particular attention was paid to whether the patients were carrying a Convid-19 infection, evaluation of thyroid tissue by ultrasound and thyroid status of the patients. According to these parameters, the patients were divided into 2 groups.Group I consisted of 45 (56%) adult patients with type 1 diabetes who had a history of Convid-19 infection. Among these patients 22 (49%) were females and 23 (51%) were males whose age ranged from 19 to 40 years. Group II consisted of 35 (44%) adult patients with type 1 diabetes who had no history of Covid-19 infection. Among these patients 17 (48%) were females and 18 (52%) were males whose age ranged from 18 to 48 years. All patients underwent general clinical examination including palpation of thyroid gland, ultrasound of thyroid region and lymph nodes, IHLA examination of T4, TSH, anti-TPO count, fine needle aspiration biopsy if there were nodules in thyroid tissue.
4. Results Obtained
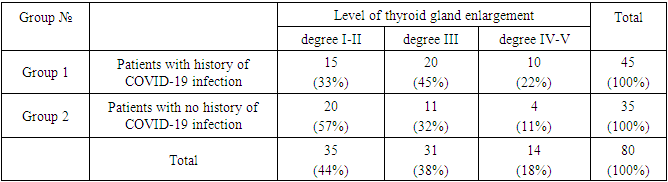
- According to the classification of Nikolaev O.V., 15 (33%) patients who underwent Covid-19 group 1 infection had I-II degree thyroid enlargement, 20 (45%) patients had III degree thyroid enlargement and 10 (22%) patients had IV-V degree thyroid enlargement.That is, 20 (57%) patients in group 2 with a history of not tolerating Covid-19 had thyroid enlargement of degree I-II, 11 (32%) - thyroid enlargement of degree III, and 4 (11%) - thyroid enlargement of degree IV-V (Table 1).
|
|
|
|
5. Conclusions
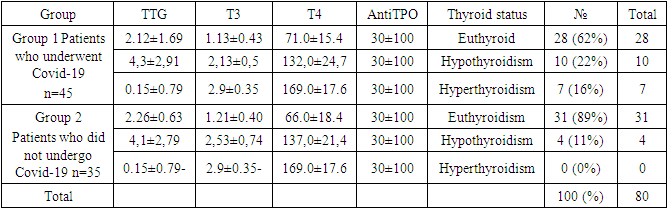
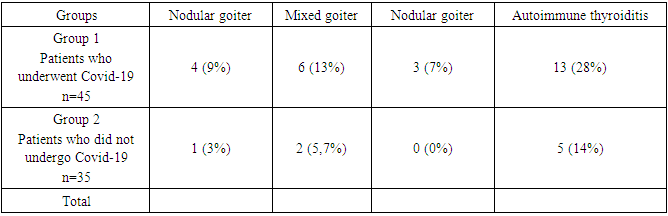
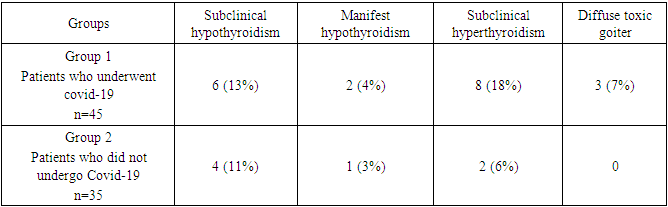
- 1. When analysing the patients examined by ultrasound, in group 1 of patients who underwent COVID-19 infection, AIT in the thyroid gland was detected in 13 (28%) patients, nodular goiter in 4 (9%), mixed goiter in 6 (13%) patients, multinodular goiter in 3 (7%). In group 2, i.e., patients without history of COVID-19 infection, autoimmune thyroiditis was detected in 15 (10%) patients, nodular goiter in 1 (3%), mixed goiter in 2 (5.7%). However, multinodular thyroid goiter was not detected in this group of non-COVID-19 infected patients. 2. When the thyroid status of the patients was analysed, 62% of patients in group 1 were euthyroid, 22% - hypothyroid and 16% - hyperthyroid. 89% of patients in group 2 were euthyroid and 11% were hypothyroid. The condition of hyperthyroidism was not observed in any patient in this group. 3. In comparative evaluation of thyroid diseases detected in the thyroid gland by ultrasonography, in group 1 patients, nodular goiter was diagnosed in 4 (9%) patients, mixed goiter in 6 (13%) patients and multinodular goiter in 3 (7%) patients, while autoimmune thyroiditis was diagnosed in 13 (28%) patients. In type 1 diabetic patients without COVID-19 infection, nodular goiter was diagnosed in 1 (3%) patient, mixed goiter in 2 (6%) patients and autoimmune thyroiditis in 5 (14%) patients, while multiple nodular goitre was not observed in any patient (0%).4. On analysing the thyroid status of group 1 patients who had undergone Covid-19 infection, 6 (13%) patients had subclinical hypothyroidism, 2 (6%) patients had manifest hypothyroidism and 8 (18%) patients had subclinical hyperthyroidism. However, 3 (7%) patients were diagnosed with diffuse toxic goiter. Of the patients in group 2 who did not have Covid-19 infection, 4 (11%) had subclinical hypothyroidism, 1 (3%) had manifest hypothyroidism, and 2 (6%) had subclinical hyperthyroidism. On the other hand, diffuse toxic goiter was not diagnosed in any patient.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML