-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(10): 1482-1487
doi:10.5923/j.ajmms.20231310.26
Received: Sep. 12, 2023; Accepted: Sep. 30, 2023; Published: Oct. 10, 2023

Left Atrial Size as a Predictor of Response to Cardiac Resynchronizationtherapy
Khalikova A. B., Abdullaev T. A., Tsoi I. A., Amirkulov B. Zh.
Republican Specialized Scientific and Practical Medical Center of Cardiology, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Heart failure (HF) is a common syndrome with an increasing incidence. Over time, HF progresses to the terminal stage, which is characterized by refractoriness to optimal medical therapy (OMT) and requires implantation of assistive devices or heart transplantation. One of the methods of adjuvant therapy is cardiac resynchronization therapy (CRT), which has recently become generally accepted for patients with сhronic heart failure of III-IV functional class (FC) according to the classification of the New York Heart Association (NYHA), with a reduced left ventricular ejection fraction (LVEF) less than 35% and the presence of a wide QRS complex ≥120 ms. The aim of this study was to study the state of the left atrium in conjunction with other morphofunctional parameters as a predictor of response to CRT in patients with CHF.
Keywords: Heart failure, Cardiac resynchronization therapy, Left atrial remodeling, Left atrial deformity, Reverse left ventricular remodeling
Cite this paper: Khalikova A. B., Abdullaev T. A., Tsoi I. A., Amirkulov B. Zh., Left Atrial Size as a Predictor of Response to Cardiac Resynchronizationtherapy, American Journal of Medicine and Medical Sciences, Vol. 13 No. 10, 2023, pp. 1482-1487. doi: 10.5923/j.ajmms.20231310.26.
1. Introduction
- The positive effects of cardiac resynchronization therapy (CRT) have proven themselves well in patients with congestive heart failure (HF), reduced left ventricular function (LV) and a wide QRS complex [1]. By restoring electrical synchrony, CRT leads to an improvement in the size and function of the heart, the so-called reverse LV remodelling [2]. The induced positive process of LV reverse remodeling using CRT has been identified as the main mechanism for reducing mortality, increasing exercise tolerance and reducing the frequency of hospitalizations in this category of patients [3,4]. Unfortunately, the response to CRT varies significantly among patients, a third of them do not have reverse LV remodeling after CRT [5]. The variability of the individual response to CRT requires a more careful selection of patients. Recently, there has been a growing interest in the volume and function of the left atrium (LA) in patients with CH, since they are known markers of disease severity in this population. LA expands due to chronically elevated high filling pressure over time. LA remodeling is a complex process that is defined as a persistent change in LA size (structural remodeling of LA) and/or function (functional remodeling of LA). One of the sections of the MADIT-CRT study showed that a smaller initial volume of the left atrium was independently associated with a positive response to CRT [6]. This highlights the importance of understanding the volume and function of the left atrium in these patients. Speckle-tracking echocardiography allows for a more complete analysis of the function of the left atrium, which may be of additional importance for predicting the response of CRT. Thus, the purpose of this study was to assess the prognostic value of the structural (LA volume) and functional (deformation of the LA reservoir) LA remodeling in response to LV CRT.
2. Materials and Methods
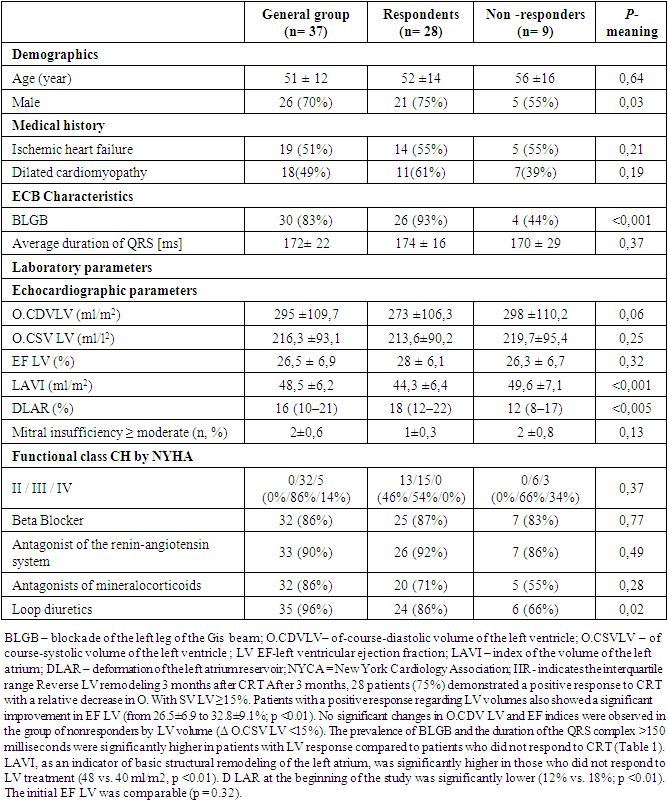
- A single-center retrospective non-randomized study included data from 37 patients with CH, class III-IV according to NYHA, refractory to optimal drug therapy for at least 6 months, severe violation of LV systolic function, with FV LV 18-40%, with the morphology of the QRS complex by the type of complete blockade of LNGP and PNPG and the duration of the QRS complex ≥130 ms in the period from October 2015 to November 2022. When determining the indications for surgery, the recommendations of the All-Russian Scientific Society of Arrhythmologists (BNOA), the European Society of Cardiology were used, and they also focused on the presence of echocardiographic criteria for myocardial dissynchrony. Patients underwent echocardiographic examination before CRT and after CRT after 6 months. The average age of patients was 51±12 years; at the time of CRT, 76% had a sinus rhythm; 21% had a permanent form of atrial fibrillation; 3% had complete atrioventricular blockade on the background of atrial fibrillation. The analysis of LV remodeling parameters according to transthoracic echocardiography (EchoCG), as well as the analysis of the valvular apparatus of the heart, in comparison with the functional class (FC) of CHF of the New York Heart Association (NYHA).The criteria for inclusion in the study were:• age over 18 years;• XCH II-IV FC according to NYHA classification at the outpatient stage of treatment;• EF LV ≤35% (Simpson);• QRS complex width >120 ms;• sinus rhythm, complete blockade of the left leg of the Gis bundle;• optimal drug therapy of XCH;• signed informed consent to participate in the study.The exclusion criteria were:• acute cerebrovascular accident <3 months before the start of the study;• patients who were scheduled to undergo myocardial revascularization or heart transplantation during the follow-up period;• congenital and acquired defects, as well as heart tumors, LV aneurysm, when their surgical correction was planned during the follow-up period;• active inflammatory and autoimmune diseases of the myocardium;• thyrotoxicosis at the time of inclusion in the study;• anemic syndrome: blood hemoglobin level <90 g/l;• diseases that limit life expectancy (<1 year).Implantation techniqueStandard methods were used for implantation of the CRT device. Three trans venous electrodes were inserted for stimulation: one into the right atrium, the other into the high interventricular septum or the apex of the right ventricle, and the electrode from the coronary sinus was located near the free LV wall through the supply vein of the coronary sinus. The leads for stimulation were connected to a two-chamber biventricular device with a programmable interventricular delay. The device was programmed in DDD mode, and the atrioventricular (AV) delay was adjusted during simultaneous stimulation.Echocardiographic evaluationEchocardiograms were obtained before and 3 months after CRT implantation. The Philips clear vue 350 ultrasound machine was used for the study. Transthoracic echocardiographic evaluation was performed in accordance with the recommendations of the American Society of Echocardiography and the European Association of Cardiovascular Imaging, including end-systolic and end-diastolic LV volume (O.CSV and O.CDVLV) [8]. The ejection fraction LV (E FLV) was calculated using a modified bi-plane Simpson rule. The maximum volume of LA related to the body surface area (IVLA) was calculated by the biplane disk method at the end of the systole. Commercially available software (QLAB 13, Philips Healthcare, Eindhoven, the Netherlands) was used to measure LV reservoir deformation (RDLA) on apical four- and two-chamber LV projections with stable ECB recording and frame rate >60 frames per second. [9,10]. The endocardial border of the left atrium was performed automatically, followed by manual adjustment, if necessary. The zero strain standard was set at the end of the diastole to determine RDLA [9].Statistical analysisStatistical analysis and construction of information models was carried out using the IBM SPSS 23 program. For quantitative variables, arithmetic averages and standard deviations (m±sd) were calculated if the normality of the attribute distribution was confirmed, or the median and [25%; 75%] percentiles otherwise. The critical level of statistical significance was assumed to be 0.05. The normal distribution of features was checked using the Shapiro-Wilk criterion. The nonparametric Wilcoxon Signed Ranks Test was used to conduct paired comparisons. The comparison of two independent groups was carried out using the Mann-Whitney Test. Ischemic heart failure was observed in 19 (51%) patients. The patients were predominantly male (n = 26, 70%), with an average age of 51 ± 12 years. The main concomitant diseases were arterial hypertension (n = 18, 48%) and diabetes mellitus (n = 6, 16%). The delay of intraventricular conduction was most often associated with the blockade of the left leg of the Gis bundle (n = 31, 83%) with an average duration of QRS 172 = 22 ms. More than half of the patients (83%) initially had NYHA Class III. Initially, the mean O.CDVLV was 216.3±93.1 ml/m2, LVEF 26.5 ± 7%, LAVI 48.5±6.2 ml/m2. Most patients were prescribed beta-blockers (86%), renin-angiotensin antagonists (90%), mineralocorticoid antagonists (86%) and loop diuretics (96%).
|
|
3. Discussion and Results
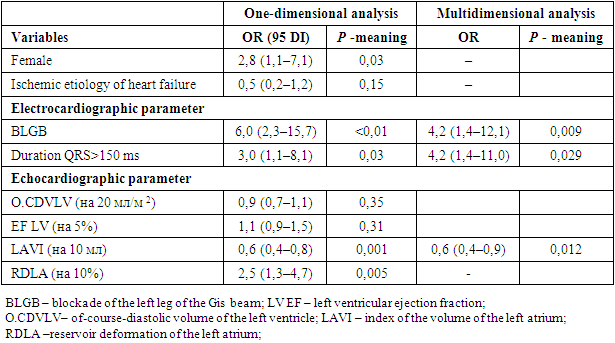
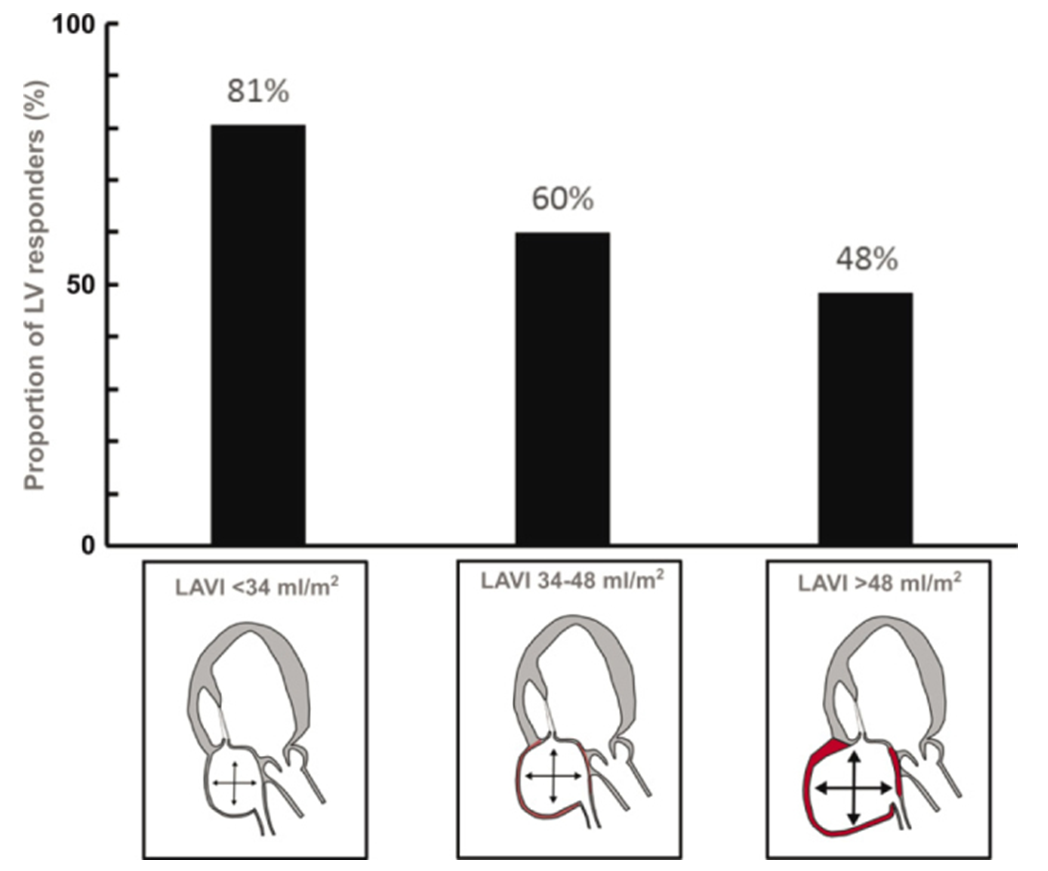
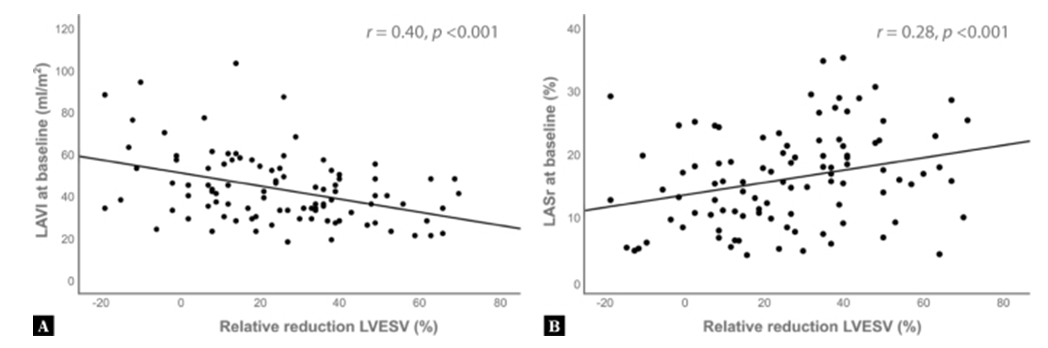
- Numerous studies have shown a direct relationship between the size of LA and the development of atrial fibrillation, thromboembolism, respiratory disorders and CH [1,6,8]. This dependence is explained by a violation of the electrophysiological properties of the atrial myocardium with overgrowth of its wall, stagnation of blood in the enlarged and fibrillating atrium, compression of adjacent anatomical structures with increased LA. According to large population studies, atriomegaly is a risk factor (RF) for sudden death [5]. The giant left atrium is a significant factor in the surgical correction of mitral valve defect for the reasons mentioned above. Some authors define left atriomegaly as an increase in anteroposterior LA size of more than 5 cm [7], 6 cm [1,3-5] or 6.5 cm [5,8]. Other authors understand left atriomegaly as a condition when LA has a diameter of more than 8 cm [5] or 8.5 cm [5,9,10]. Kawazoe et al [11,12] atriomegaly is defined as a condition in which the presence of dilated LA causes symptoms of LV compression and/or bronchopulmonary compression. The development of left atriomegaly has a number of consequences. Enlargement of the LA cavity and overstretching of its walls are accompanied by the development of atrial fibrillation, as a consequence-a decrease in cardiac output and an increase With LA dilatation, the atrial septum in some cases may shift towards the mouth of the inferior vena cava, causing its partial obstruction, which is manifested by an increase in the peak blood flow rate at the mouth of the inferior vena cava and a decrease in venous return to the right atrium. In our study, both the typical BLGB and the broad duration of the QRS complex were associated with a positive response to CRT; both indicators are well-known predictors of a positive response to CRT [13]. The novelty of our study was that LAVI was an independent predictor and was inversely proportional to the positive response after CRT. This data is consistent with the previous CRT study. The MADIT study has already shown that the smaller size of the left atrium is a significant predictor of the response to CRT [14]. It is noteworthy that a close relationship between LAVI and the response to CRT persisted after remodeling of the initial end-diastolic volume and LV function, whereas the latter parameters had no independent prognostic value.There is more and more evidence of the importance of left atrial function increasing with atrial dilation in patients with CH. Left atrial deformity analysis is a relatively new, reliable and affordable method for quantifying left atrial function [9]. In this study, we used a prospective database of single-center CT implantations for 2015-2022 to assess the prognostic value of this new echocardiographic parameter. In our study, reservoir deformation of LA (RDLA) was not associated with reverse LV remodeling in multivariate analysis. Notably, this observation is inconsistent with a previous study by Feneon et al. [15] In this small study with 79 patients, RDLA was an independent predictor of LV remodeling response. A larger prospective multicenter study by Galli et al. [16] also provided evidence that R DL A is an independent predictor (p = 0.049). However, the correlation between RDLA and reverse LV remodeling was weak (r = -0.27, p <0.001), as in our study (r = -0.28, p <0.001). Nevertheless, the results of these studies emphasize the importance of assessing the state of the left atrium in candidates for CRT, which is consistent with our results. A retrospective evaluation was made of 37 patients with NYHA class III-IV HF refractory to optimal medical therapy for at least 6 months who underwent echocardiography before and 3 months after implantation of a cardiac synchronizing device. A positive response to cardiac resynchronization therapy was defined as a relative decrease in left ventricular end-systolic volume by ≥15%.Indexed left atrial volume, left atrial reservoir strain, left ventricular end-diastolic volume and left ventricular ejection fraction along with other known predictors of response to cardiac resynchronization therapy (gender, etiology of heart failure, presence of a typical pattern of left bundle branch block, QRS complex) duration >150 ms) were included in a multivariate logistic regression model to determine predictors of response to cardiac resynchronization therapy.A positive response to cardiac resynchronization therapy was observed in n = 28 (76%) patients out of 37 candidates. Presence of typical left bundle branch block (OR 4.2, 95 CI: 1.4–12.1, p = 0.009), QRS complex duration > 150 ms (OR 4.2, 95 CI: 1.4–11, 0, p = 0.029) and the left atrial volume index (OR: 0.6, 95 CI: 0.4–0.9, p = 0.012) remained the only significant predictors of a positive response to cardiac resynchronization therapy after 3 months.
4. Conclusions
- Left atrial size at baseline is an independent predictor and is inversely related to left ventricular volume remodeling in candidates for cardiac resynchronization therapy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML