-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(10): 1473-1476
doi:10.5923/j.ajmms.20231310.24
Received: Aug. 10, 2023; Accepted: Sep. 15, 2023; Published: Oct. 10, 2023

Open Surgery versus Endovascular Surgery Results on Lower Limb Arterial Thrombosis after Coronavirus Infection
A. A. Irnazarov 1, U. A. Asrarov 1, V. R. Khasanov 2, J. K. Matmuradov 1, R. I. Kurbanbaev 1, Sh. Sh. Shamshiddinov 1
1Tashkent Medical Academy, Uzbekistan
2Multidisciplinary Clinic of Tashkent Medical Academy, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The research reflects the result of different types of surgical interventions on patients with lower limb arterial thromboses, who had had coronavirus infection. 42 patients were divided into 2 groups: the primary group patients underwent to endovascular thrombaspiration and systemic thrombolysis; and control group patients – thrombectomy. The results demonstrate applying of endovascular thromaspiration and thrombolysis significantly decreases frequency of complications, rethromboses and mortality over the thrombectomy.
Keywords: Lower limb arterial thrombosis, Acute ischemia, Thrombectomy, Endovascular thrombaspiration and systemic thrombolysis, Coronavirus infection
Cite this paper: A. A. Irnazarov , U. A. Asrarov , V. R. Khasanov , J. K. Matmuradov , R. I. Kurbanbaev , Sh. Sh. Shamshiddinov , Open Surgery versus Endovascular Surgery Results on Lower Limb Arterial Thrombosis after Coronavirus Infection, American Journal of Medicine and Medical Sciences, Vol. 13 No. 10, 2023, pp. 1473-1476. doi: 10.5923/j.ajmms.20231310.24.
1. Introduction
- Information regarding the incidence of acute lower limb ischemia is scarce, but several national registries and regional surveys give figures of 140,000,000 per year. According to I. N. Bokarev, one case of acute ischemia occurs annually per 6,000 people [1,2,3]. The incidence of acute ischemia associated with embolism has decreased in recent years, probably because of a decrease in rheumatic valvular heart disease, improved monitoring of such patients, and progress in the treatment of patients with cardiac arrhythmias. On the contrary, cases of acute thrombotic ischemia have become more common [4,5].The most common cause of acute thrombosis is atherosclerosis, in which thrombosis can develop as a primary thrombosis against the background of an asymptomatic ulcerated plaque, or as a secondary one against the background of a long-term occlusive-stenotic process [6]. Primary acute thrombosis (up to 42% of the total number of cases of acute thrombosis) clinically differs little from arterial embolism - a sudden onset is characteristic. Coronavirus affected pandemic significantly had spread the frequency both arterial and venous thrombosis due to the systemic endothelial dysfunction and initiating hypercoagulation over hemorrhagic complications [7-13]. Identification of acute arterial thrombosis due to the coronavirus-assosiated coagulopathy and it’s further complications, their possible ways of managing and recovering still has their actuality and in demand. The aim of the research is to improve the results of treatment of patients with lower limbs arterial thrombosis, who have had coronavirus infection, by optimizing the tactics of surgical intervention.
2. Materials and Methods
- The research includes 42 patients with acute lower limbs’ arterial thromboses for the period from September 2021 to January 2022 at the Emergency Surgery Department of the Multidisciplinary Clinic of the Tashkent Medical Academy. The average age was 56±0.7 years. 28 (66.7%) of them were male, 14 (33.3%) female. There were 2 groups depending on the applied treatment tactics: the primary group - 22 (52.4%) and the control one - 20 (57.6%) patients. All of patients, underwent to the research had anamnesis of coronavirus infection. An average duration of recovering from COVID-19 was 2 months. Diagnosis included standard clinical laboratory and instrumental examinations, supplemented by ultrasound dopplerography (USDG), ultrasound duplex scanning (USDS) of the lower limbs’ vessels, multisliced CT with contrasting angiography of the lower limbs’ arteries. Confirmation of positive coronavirus infection anamnesis included enzyme-linked immunosorbent assay technique. All patients had standard preoperative preparation, including double anticoagulant, infusion therapy, improving of blood circulation in the microvasculature.
3. Results and Discussion
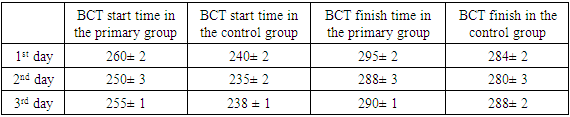
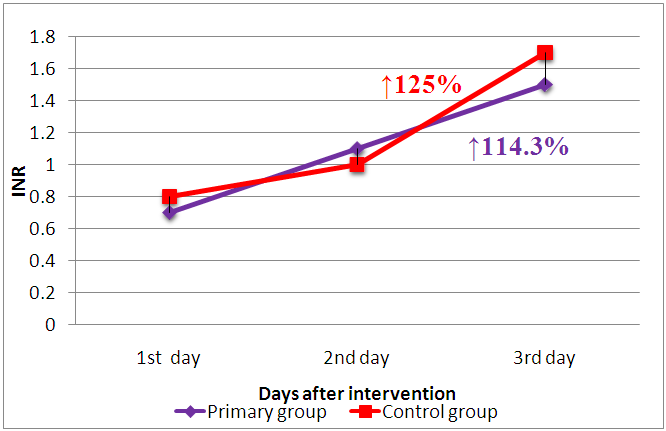
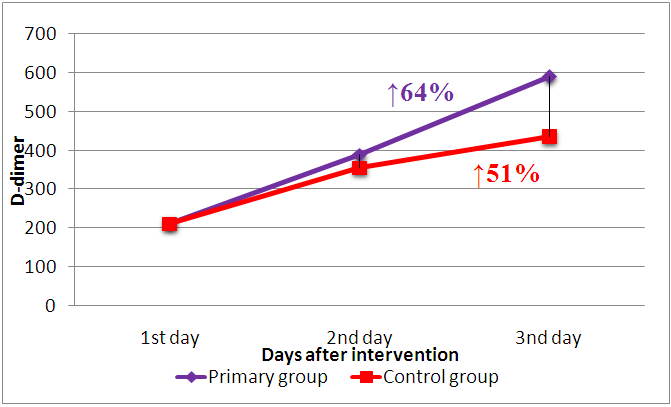
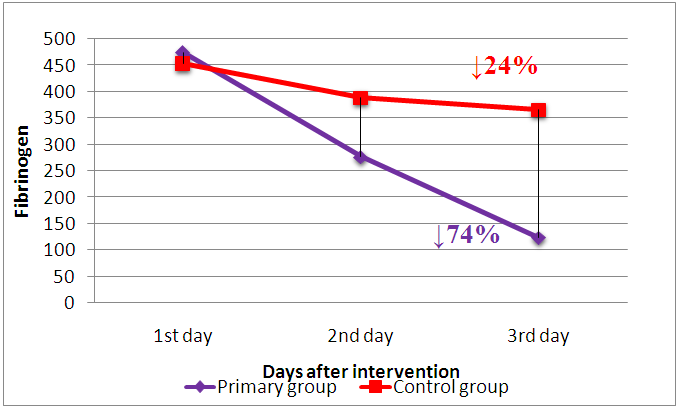
- The degree of ischemia was determined according to A.S. Saveliev’s classification; and there were 7 (31.8%) patients in the primary group, whom were diagnosed II-a degree of acute ischemia; 12 (54.5%) — II-b; 3 (13.6%) — III-a. In the control group, the distribution according to the degree of acute ischemia next: 8 (40%) patients — II-a degree; 10 (50%) — II-b; 2 (10%) - III-a. According to the level of arterial damage: in the primary group, 12 (54.5%) patients had thrombothic lesion at femoral segment, 10 (45.5%) patients had thrombosis of the femoral-popliteal segment. In the control group: 13 (65%) patients had thrombothic lesion at femoral segment, 7 (35%) patients had thrombosis of the femoral-popliteal segment. According to the ratio of concomitant diseases, a significant preponderance of a certain nosology was not determined in any of the researched groups.Surgical interventions were performed within 24 hours after admission with further hospitalization to the department. Patients in the control group underwent thrombectomy at the affected arterial segment and fasciotomy (according to indications), while patients in the primary group underwent endovascular thrombaspiration and thrombolysis. In cases where it was impossible to puncture the femoral artery on the affected limb, access was approched through the contralateral lower limb. Urokinase was used as a thrombolytic drug. The effectiveness of the method was determined on the basis of a number of subjective and objective criteria. Changes in clinical dynamics were considered as subjective criteria: limb warming, skin color change, improvement in motor and sensory functions, and the appearance of pulsation distal to thrombosis. The objective criteria included changes in USDG parameters in the form of an improvement in the ankle-brachial index (ABI), changes in speed indicators and visual sonographic control of thrombolysis. However, the main objective criterion for thrombolysis was angiography data during and after the procedure.After performed thrombectomies on patients of the control group, regression of ischemia detected in 16 (80%) patients. In 2 (10%) cases, rethrombosis was noted within 12 hours after the surgical intervention and therefore these patients underwent repeatedly thrombectomy. In addition, in 2 (10%) cases, after thrombectomy, there was no regression of ischemia, and a following secondary high amputation of the lower limb was performed. No lethality in the control group was observed. In all 2 (10%) patients with 3rd stage ischemia, thrombectomy was mandatory supplemented with anterior and posterior fasciotomy. Thrombectomy was performed in all cases with an incision along the Ken line.In the patients of the primary group, who underwent endovascular thromboaspiration and thrombolysis, no episodes of retrombosis were observed. However, in 1 (4.54%) case, a partial regression of ischemia was detected with irreversible necrotic changes, limited in the foot by a demarcation line, which was subsequently disarticulated. To perform endovascular thrombaspiration and thrombolysis, femoral angiography was performed by antegrade puncture of the femoral artery with the installation of a catheter for subsequent lysis.After completion of mechanical thrombaspiration in arterial lumen, due to selective administration, in most cases it was possible to obtain positive results with a systemic effect of fibrinolytics. The dose of urokinase ranged from 300,000 to 900,000 IU. The efficiency monitoring of performed system thrombolysis was estimated by levels of INR (2-3), D-dimer (>500 ng/ml) and fibrinogen (100-150 mg%) concentration. The catheter for system usage was removed after the normalization of the parameters of the blood coagulation system (on the 3rd day after the procedure).Despite the advantage of thrombolysis in peripheral arterial thrombosis, not all patients managed to completely lyse thrombi. However, even with successful thrombolysis, the causative factors of thrombosis were not eliminated. Therefore, peroral anticoagulant medicament for prolonged taking was prescribed for 10 (45.5%) patients.To determine the correlation between the incidence of complications, the blood coagulation system was assessed every 24 hours after the interventions.
|
 | Chart 1. INR in the groups |
 | Chart 2. D-dimer concentration in the groups |
 | Chart 3. Fibrinogen concentration in the groups |
4. Conclusions
- In the course of diagnostic measures, thrombosis was detected against the background of an atherosclerotic process in combination with a passable tibial segment; primary reconstructive surgery is indicated for such patients.Indirect thrombectomy is indicated for thrombosis of the main arteries without significant atheromatous lesions or emboli.Indications for endovascular thrombolytic therapy are peripheral forms of thrombosis or long-standing thrombosis against the background of a pronounced atherosclerotic lesion with an unsatisfactory peripheral vascular bed, i.e. when indirect thrombectomy is unfavorable prognostically, and reconstructive surgery cannot be performed.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML