-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(10): 1469-1472
doi:10.5923/j.ajmms.20231310.23
Received: Aug. 7, 2023; Accepted: Sep. 16, 2023; Published: Oct. 10, 2023

Correlation Analysis in Assessing the Development of Pulmonary Hypertension in Children with Congenital Heart Defects
Mamura Shokir Kizi Rakhmatillayeva, Aliyeva Nigora Rustamovna
Department of Hospital Pediatrics No. 1, Folk Medicine, Tashkent Pediatric Medical Institute, Uzbekistan
Correspondence to: Mamura Shokir Kizi Rakhmatillayeva, Department of Hospital Pediatrics No. 1, Folk Medicine, Tashkent Pediatric Medical Institute, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Pediatric hypertensive vascular lung disease associated with congenital heart defects (CHD) is a condition in which the average pressure in the pulmonary artery (PA) at rest, determined by cardiac catheterization, is ≥2.0 mm Hg, and the general pulmonary resistance (OLS) is ≥ 3 U/ m2 for CHD with biventricular hemodynamics. [2,5].
Keywords: Pulmonary hypertension, In children, Congenital heart defects, Endothelin-1, VEGF, NT-proBNP, Interleukin 1, Mean pulmonary artery pressure
Cite this paper: Mamura Shokir Kizi Rakhmatillayeva, Aliyeva Nigora Rustamovna, Correlation Analysis in Assessing the Development of Pulmonary Hypertension in Children with Congenital Heart Defects, American Journal of Medicine and Medical Sciences, Vol. 13 No. 10, 2023, pp. 1469-1472. doi: 10.5923/j.ajmms.20231310.23.
1. Introduction
- The development of hypertensive pulmonary vascular disease in CHD with abnormal intracardiac blood discharge depends on the anatomical variant, the size of the defect, and the volume of blood discharge through the defect. Children with не корригированнымиuncorrected common arterial trunk, transposition of great vessels with DMV, non -restrictive DMV and OAP are at risk for the earliest development of pulmonary vascular disease. The late-risk group consists of children with an atrial septal defect. The rate of development of pulmonary vascular disease also depends on the genetic predisposition. [8,9,10]Numerous biomarkers have been shown to carry prognostic significance in PH and to correlate with other predictors of outcome. As CHD–PH differs significantly to other types of PH in terms of cardiac physiology and prognosis, it is indeed a worthwhile endeavor reviewing the evidence related to this expanding group of patients. In the present systematic review, we sought to evaluate the literature on the role of NT-proBNP, ED-1, and VEGF in the diagnosis, clinical management and prognosis of patients with CHD–PH. [6]Objective: to analyze immunological and echocardiographic data using correlation.
2. Materials and Methods
- For the period from 2019 to 2022, 139 children with congenital heart defects were examined and dynamically monitored (clinical base clinic TashPMI). Clinical symptoms of the disease, PH degree and functional class, hematological parameters, coagulogram, echocardiography, markers of endothelial dysfunction were analyzed at the beginning of the study - when the patient was admitted to the observation in the TashPMI clinic.EchoCG diagnostics of heart damage was mainly performed at the TashPMI clinic, with color Doppler mapping performed on the Logic 400 device, according to an extended protocol, including assessment of the right heart using tissue pulse Dopplerography, standard approaches and positions were used, in accordance with ESC/ASE recommendations.For the immunological study, blood was centrifuged at 3000 rpm. for 5 minutes to produce plasma, which was stored in a deep-freeze freezer (-80 gr. C) until the study is conducted: Todetect markers of endothelial dysfunction (ET-1, VEGF, IL - 1) and the concentration of the N-terminal fragment of the brain natriuretic peptide in the blood serum of patients by ELISA test systems, we used an automated HUMAREADER HS immunochemiluminescence analyzer (Biomedica, Germany).Correlation analysis correlation dependence was performed to identify the statistical relationship of two or more random variables using the Pearson (r) method.
3. Research Results
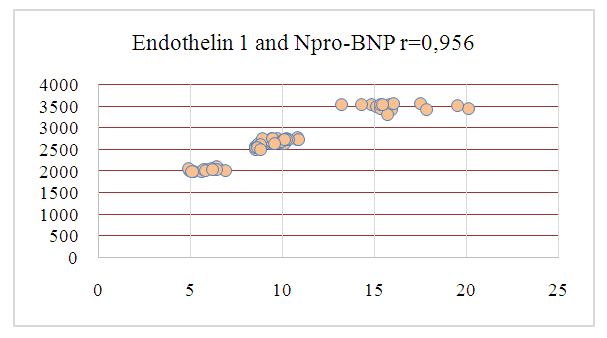
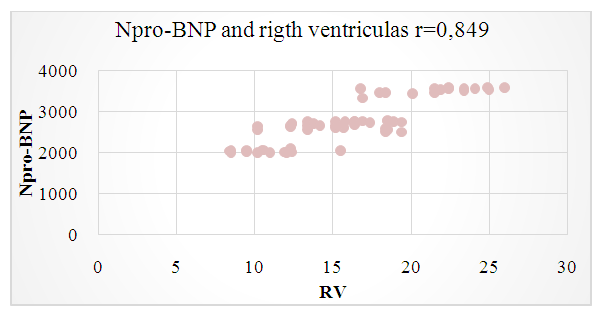
- The analysis of the parameters of the right heart was carried out using ultrasound assessment of the heart and large vessels, determining the severity of pulmonary vascular resistance. It was found that as the severity of arterial hypoxemia increases and the level of Npro-BNP increases, the stiffness of the vascular wall in the channel of the small circle increases and, accordingly, the increase in blood pressure in the pulmonary artery (Fig. 1).
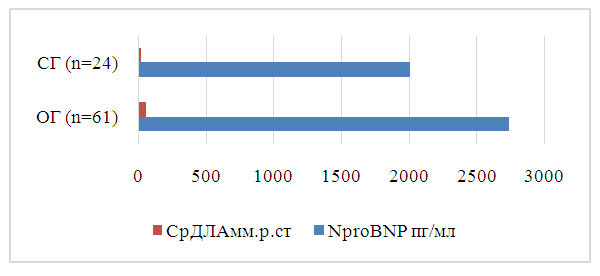 | Figure 1. Indicators of pulmonary hypertension in children with congenital heart defects |
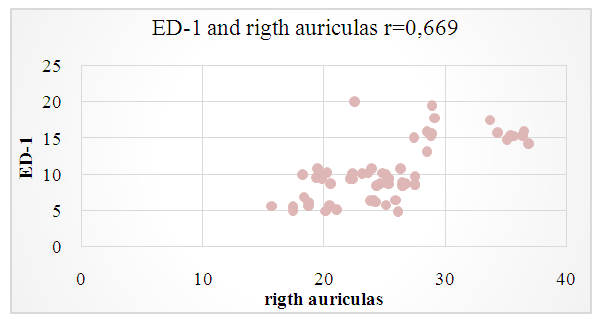
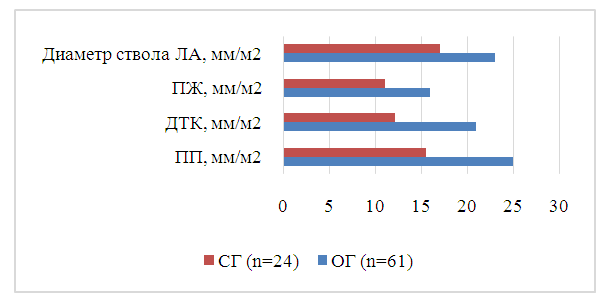 | Figure 2. Morphological characteristics of the right heart in children with congenital heart defects |
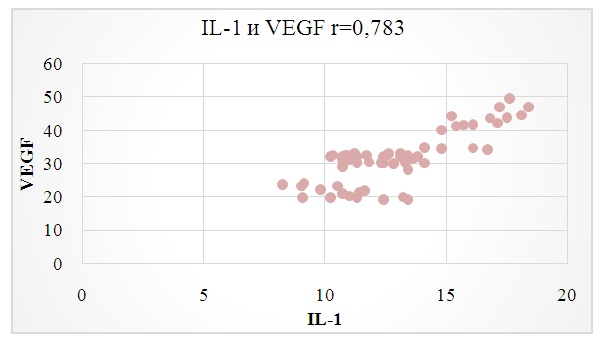
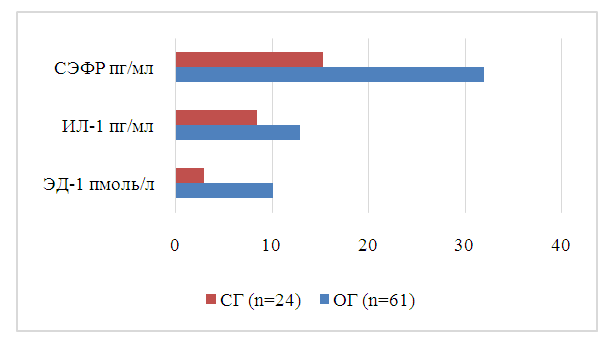 | Figure 3. Markers of endothelial dysfunction in children with PH-CHD |
|
 | Figure 4 |
 | Figure 5 |
 | Figure 6 |
 | Figure 7 |
 | Figure 8 |
4. Conclusions
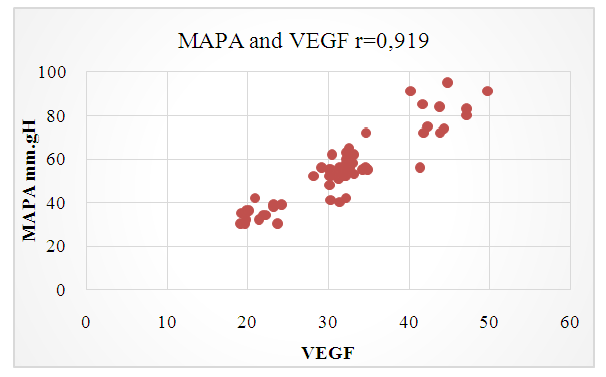
- Our research has shown that immunological biomarkers and morphofunctional parameters of the right heart can be a prognostic indicator of the development of pulmonary hypertension in children with CHD.Markers of endothelial dysfunction: ET-1, VEGF, IL-1, and NproBNP revealed strong positive and negative correlations between the morffunctional indicators of the right heart, which allows for early diagnosis of pulmonary hypertension in children with congenital heart disease and allows for early detection in polyclinic care.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML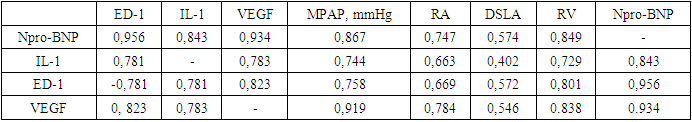
 /mTitle..., Int J Cardiol (2014), http://dx.doi.org/10.1016/j.ijcard.2014.04.156.
/mTitle..., Int J Cardiol (2014), http://dx.doi.org/10.1016/j.ijcard.2014.04.156.