-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(10): 1462-1466
doi:10.5923/j.ajmms.20231310.21
Received: Sep. 13, 2023; Accepted: Sep. 30, 2023; Published: Oct. 10, 2023

Structural Analysis of Urological Complications after Renal Transplantation from a Living Related Donor
F. R. Nasirov, F. A. Akilov, Sh. T. Mukhtarov, S. S. Kariev, D. Kh. Mirkhamidov, Z. T. Matkarimov, N. M. Rakhimov, M. M. Khasanov
Republican Specialized Scientific and Practical Medical Center of Urology, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Aim of the research was to study the frequency and structure of urological complications in the early and long-term period after related renal transplantation. Material and methods. The study was based on the results of examination and treatment of 162 adult recipients (≥ 18 years) with urological complications after a related renal transplantation, who were on outpatient and inpatient treatment at the Republican Specialized Scientific and Practical Medical Center of Urology and at the Republican Specialized Scientific and Practical Medical Center of Surgery named after acad. V. Vakhidov for the period from June 2010 to May 2023. The features of the spread and structure of the major (ureteral stenosis/stricture, vesicoureteral reflux, urine leakage, transplanted kidney lithiasis) and minor (urinary tract infection, asymptomatic bacteriuria, lymphocele) urological complications in the early and long-term period after a related renal transplantation were studied. Results. We analyzed a cohort of 840 recipients after related renal transplantation and determined that the prevalence of urological complications after related renal transplantation is 19.3%, with a higher frequency of occurrence (14.3%) in the early and near (0-3 months) period, manifested by the main (ureteral stenosis/stricture (1.3%), urine leakage (0.5%) and vesicoureteral reflux (2.1%)) and small (urinary tract infection (7.6%), asymptomatic bacteriuria (2.4%), lymphocele (5.2%) and stone formation (0.1%)) complications. Conclusion. Urological complications are frequent complications of related renal transplantation and represent a serious burden for the patient and the healthcare system, and may require invasive procedures or repeated surgeries. At the same time, they often have an asymptomatic course, clinical manifestations are nonspecific and often delay from the moment of onset.
Keywords: Renal transplantation from a living related donor, Urological complications, Prevalence, Structure
Cite this paper: F. R. Nasirov, F. A. Akilov, Sh. T. Mukhtarov, S. S. Kariev, D. Kh. Mirkhamidov, Z. T. Matkarimov, N. M. Rakhimov, M. M. Khasanov, Structural Analysis of Urological Complications after Renal Transplantation from a Living Related Donor, American Journal of Medicine and Medical Sciences, Vol. 13 No. 10, 2023, pp. 1462-1466. doi: 10.5923/j.ajmms.20231310.21.
1. Introduction
- Renal transplantation (RT) is the gold standard for the treatment of chronic kidney disease (CKD) and has a significant impact on the life quality [1]. Renal transplant recipients are at risk of developing various postoperative complications against the background of receiving immunosuppressive drugs and concomitant pathologies associated with long-term CKD [2-3].Major and minor urological complications (UCs) are the second cause of morbidity after RT and rejection episodes, and may be associated with graft loss and mortality [3-6]. Main or major UCs include urine leakage, ureteral stenosis, bladder outlet obstruction, vesicoureteral reflux (VUR) and graft lithiasis [6-7]. The development of UOs is associated with a longer hospital stay, higher overall costs and often requires additional interventions. [1,8-9]. They can develop at any time after RT with a favorable prognosis in cases where the disease has been detected and timely treatment has been initiated [5,10]. The total recorded incidence of UCs after RT varies from 2.5% to 14%, depending on the series and the criteria used to determine them [2,3-4]. Numerous predictors of UCs have been documented, such as donor age, renal artery variants, recipient male sex, cytomegalovirus (CMV) infection, delayed graft function and extensive periureteric connective tissue dissection [11]. This incidence has decreased in recent years due to the use of double J-stents, adaptation of the extravesical ureteroneocystostomy technique by Leach-Gregoire, improvements in perfusion-preserving kidney harvesting techniques and decreased use of steroids [10,12-14]. Aim of the research was to study the frequency and structure of urological complications in the early and long-term period after related renal transplantation.
2. Material and Methods
- The study was based on the results of examination and treatment of 162 adult recipients (≥ 18 years) with urological complications after a related renal transplantation, who were on outpatient and inpatient treatment at the Republican Specialized Scientific and Practical Medical Center of Urology and at the Republican Specialized Scientific and Practical Medical Center of Surgery named after acad. V. Vakhidov for the period from June 2010 to May 2023. The mean age of recipients with UOs was 34.5 years (from 20 to 63 years). Young patients (from 18 to 44 years) predominated among the recipients – 84.0% (136 from 162). Middle-aged recipients (45-59 years) made up 15.4% (25 from 162). Only 1 (0.6%) recipient was elderly. In most cases, the surgeries were performed on male recipients – 124 (76,5%) observations. The mean age of donors was 40.4 years (from 18 to 63 years). Young patients also predominated among donors (from 18 to 44 years) – 62.9% (102 from 162). Middle-aged donors (from 45 to 59 years) made up 34.0% (55 from 162). Всего 5 (3,1%) доноров были пожилого возраста. Male donors accounted for slightly more than half of the (50.6%; 82 from162) cases. Kidney donors were most often first-line relatives – fathers (17.3%), mothers (24.7%), brothers (24.1%) and sisters (21.0%). A significant majority of patients (90.7%; 147 from 162) were operated on due to end-stage CKD as a result of chronic glomerulonephritis. In other cases, indications for RT, i.e. the cause that led to the terminal stage of CKD, were polycystic kidney disease (2.5%; 4 from 162), chronic pyelonephritis (1.2%; 2 from 162), type 2 diabetes mellitus (0.6%; 1 from 162), various abnormalities of the urinary system (0.6%; 1 from 162) and in 4 (2.5%) recipients the etiology of CKD was not established.
3. Results
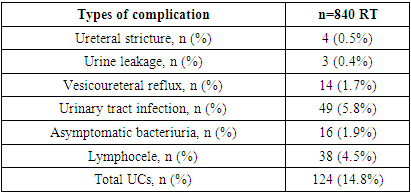
- UCs had a greater occurrence frequency in the early and immediate period after the related RT. In total, the prevalence of UCs after related RT was 19.3% (162 from 840), which determined them as a significant factor affecting the clinical course of the post-transplant period. The early and immediate period (0-3 months after RT) was characterized by the development of UCs in 14.8% (124 from 840) of cases, the frequency of which in the long-term period (more than 3 months after RT) made up 4.5% (38 from 840) (Fig. 1).
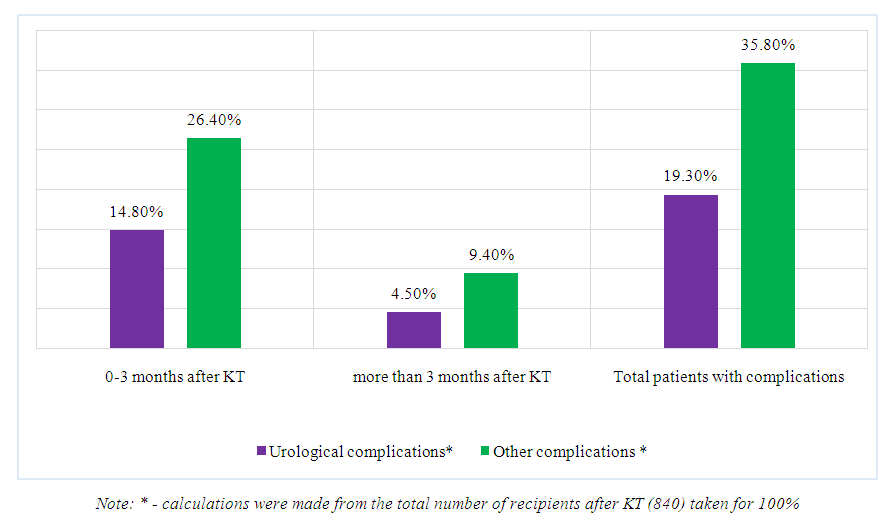 | Figure 1. The frequency of complications in the early and long-term period after related RT |
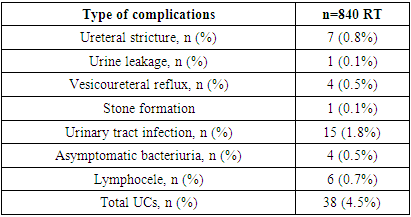
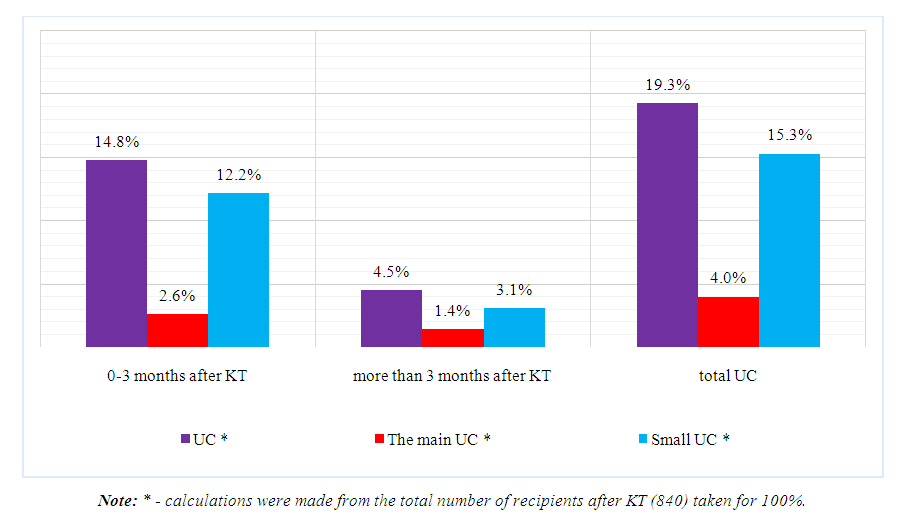 | Figure 2. Prevalence of major and minor UCs at various times after related RT |
|
|
|
4. Discussion
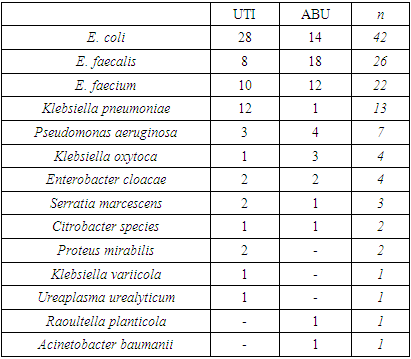
- Thus, the frequency, nature and features of the clinical course of UCs after related RT were studied, which allowed to carry out their structural analysis, the role and place in the cohort of all complications of the post-transplant period. It is reported that new RT surgical methods have reduced the incidence of UCs [8,11]. We analyzed a cohort of 840 recipients after related RT and determined that the prevalence of UCs after related RT was 19.3%, with a higher incidence (14.3%) in the early and immediate (0-3 months) period, manifested by the main (ureteral stenosis/stricture (1.3%), urine leakage (0.5%) and vesicoureteral reflux (2.1%)) and minor (UTI (7.6%), ABU (2.4%), lymphocele (5.2%) and stone formation (0.1%)) complications, which was comparable to the data presented in other publications [7,11,15]. Ureteral stenosis/stricture is one of the most formidable UCs after RT and may be associated with previous urinary incontinence or be an independent manifestation. A total of 11 cases of ureteral stenosis/stricture were registered (1.3%), which were diagnosed within 0-3 months (0.5%) or with late treatment (0.8%) for more than 3 months after RT. Ciancio et al. identified urine leakage and ureteral stenosis as the main UCs when analyzing 500 RT results [8]. Another study with 635 RTs confirmed similar results [4]. Urine leakage and UTI occur more in the early stages of the disease and are most common. Graft lithiasis can be present at any time after RT and has been reported in the literature with an incidence ranging from 0.4% to 4.4% [16]. In our study, ureteral stenosis/strictures were surgically restored using a new ureteroneocystostomy with a double J-catheter laparoscopically and by open methods. Lithiasis of the transplanted kidney was not accompanied by complete obstruction, and our approach was drug treatment. We conducted a detailed analysis of UTI and ABU, and determined that the most common pathogens found in urine samples after RT were Escherichia coli, Enterococcus faecalis, E. faecium and Klebsiella pneumoniae.
5. Conclusions
- UCs are frequent complications of related RT and pose a serious burden to the patient and the healthcare system and may require invasive procedures or repeated surgeries. At the same time, UCs after related RT are often asymptomatic, clinical manifestations are nonspecific and often delay from the moment of onset. The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML