-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(10): 1385-1389
doi:10.5923/j.ajmms.20231310.05

Optimization of Early Diagnosis of Odontogenic Osteomyelitis Based on Clinical and Immuno-Microbiological Research
Nodir K. Sharipov
Maxillofacial Surgeon of Bukhara Regional Multidisciplinary Medical Center, Uzbekistan
Correspondence to: Nodir K. Sharipov, Maxillofacial Surgeon of Bukhara Regional Multidisciplinary Medical Center, Uzbekistan.
Copyright © 2023 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

All over the world, for many years, research has been carried out to study the clinical, medico-social, experimental and laboratory aspects of acute and chronic odontogenic osteomyelitis. Treatment-diagnostic, preventive aspects of these pathological conditions are being successfully solved, and methods for treating complications of these diseases in various age categories have been developed.
Keywords: Treatment-diagnostic, Maxillofacial region, Medical problem, Periodontal diseases, Escherichia, Klebsiella
Cite this paper: Nodir K. Sharipov, Optimization of Early Diagnosis of Odontogenic Osteomyelitis Based on Clinical and Immuno-Microbiological Research, American Journal of Medicine and Medical Sciences, Vol. 13 No. 10, 2023, pp. 1385-1389. doi: 10.5923/j.ajmms.20231310.05.
1. Introduction
- The development of purulent-inflammatory diseases (PID) of the maxillofacial region (MAF) is accompanied by a change in a number of clinical parameters characterizing the state of homeostasis of the body, both systemic and local [1]. Diagnosis and treatment of GVH of the MFA, including odontogenic osteomyelitis of various forms, is still extremely relevant due to the large number of complications that do not tend to decrease [2].Given the high frequency of acute odontogenic periodontal diseases, they are an important medical problem in the clinical practice of surgical dentistry. In the general structure of stomatological diseases, the frequency of the processes of gingivitis is 55-65%. YuJSin the composition of acute CKD, it reached 69.5%, and currently, an increasing trend is observed among the population [8].Increase in the number and severity of patients with acute odontogenic infection is related to the change in the microflora caused by odontogenic infection, the decrease in the effectiveness of antibiotics, and the imperfection of conservative treatment methods for complex forms of caries. He explained that the reasons for this situation are that the population is not sufficiently aware of the consequences of caries, its prevention is still unsatisfactory, and doctors do not properly evaluate the role of focal odontogenic infection in the formation of somatic pathology. [3].The main causative agent of osteomyelitis in adults is Staphylococcus aureus, which is identified in 30% to 75% of cases. Streptococcus agalacticae, Escherichia coli, Haemophilus influenzae, Kingella kingae prevailed in late osteomyelitis in children. Staphylococcus aureus produces adhesive proteins, which contribute to the adhesion of the pathogen to the macroorganism matrix, which is a necessary condition for the further development of the infectious process.Enterobacteriaceae representatives of the family (Escherichia, Klebsiella, Enterobacter, Genera Citrobacter, Proteus, Providencia, Serratia) also caused osteomyelitis formation in 23%. They were followed by Pseudomonas spp (9%) and Streptococcus spp (9%) [8].The reasons for the increase in the number of patients suffering from acute odontogenic infection (O'OI) and the increase in the severity of its course are, firstly, the change of the microflora that causes purulent-inflammatory diseases of odontogenic origin; secondly, a decrease in the therapeutic effectiveness of broad-spectrum antibiotics; thirdly, the growth of the group of elderly and elderly patients with various "background" diseases; fourthly, it is related to the imperfection of conservative treatment methods of complex forms of caries. The authors explain the reasons for this situation with three cases: insufficient awareness of the population about the consequences of untreated caries; unsatisfactory development of caries prevention methods, insufficient assessment of the role of focal odontogenic infection by doctors in the formation and development of somatic pathology [9].These factors according to classification different suggestions cause come out bro. Current at the time of the authors according to his opinion, YuJS fire diseases according to classification b three main scientific to look there is Of a school representatives all odontogenic fire diseases of the process of osteomyelitis that he will die count a di, they are sharp periodontitis of osteomyelitis start drinking stage, that counted, they are sharp periostitis yeah _ of osteomyelitis limited shape as interpretation they did Other school representatives independent nosological forms as periodontitis and osteomyelitis distinguish between gan and periostitis odontogenic of osteomyelitis abortive to the shape they said it is relevant. Third point of view look supporters died most scientists group periodontitis, periostitis, osteomyelitis, phlegmons,abscesses and the lymphatic system damage independent nosological to forms separated [5-6].Azimov M.I. and all. According to [2019], this classification includes diseases that require urgent surgical intervention. In the classification, pulpitis, which is the starting point of the development of all other acute odontogenic inflammatory diseases, is not taken into account. The inflamed pulp, especially its chronic forms, is a source of sensitization of all tissues of the body and the nervous system. Untreated pulp sooner or later covers the periodontium in the process of tooth decay. Acute serous periodontium, then purulent periodontitis develops after the infection enters through the hole in the apex. The treatment is completed by ensuring the replacement of dead periodontium with scar tissue, which performs a support function. But if the treatment is delayed or not completed, the process continues to develop, the pus accumulated in the periodontal crack leads to the destruction of the compact alveolar plate with the spread of infection to the bone (the focus of inflammation moves to the bone).The purpose of the study clinical and immuno-microbiological studies, determining the prognosis of the disease.
2. Research Material and Methods
- Based on the above, this scientific research work was planned and conducted on this basis. It consisted of preparation, implementation and final stages.At the preparatory stage, the topic, goals and objectives of the research work were determined, the object and subject of the research were determined. During the study, chronic odontogenic osteomyelitis was studied, and acute odontogenic osteomyelitis was taken as a comparative group. Later, the material-technical, methodological and theoretical base of the scientific work was prepared. The place of research was the maxillofacial surgery department of the Bukhara regional multidisciplinary medical center, all bacteriological studies were conducted in the bacteriological laboratory of this center, as well as in the educational and scientific bacteriological laboratory of the Department of Microbiology, Virology and Immunology of the Bukhara State Medical Institute. Bacteriological and bacterioscopic, as well as immunological methods required by the doctoral student were conducted at the preparatory stage. For this purpose, research was continued when all nutrient media and reagents, as well as test systems and reagents for studying local immunity were ready.At the stage of research, the dental status, microbiological and immunological aspects of patients with acute and chronic odontogenic osteomyelitis were studied. From this, pathogens were identified to the generation and type, humoral immune factors in patients' saliva were determined, the results of all clinical, microbiological and immunological studies were recorded in special cards and journals. Research was stopped when all material was sufficient for statistical processing, interpretation and analysis, reliable results, and valid conclusions. There were no obstacles during the research.
3. Research Results
- This research, clinical material was collected from the maxillofacial surgery department of the multidisciplinary medical center of Bukhara region. Bacteriological studies were carried out in the bacteriological laboratory of the center and the educational scientific bacteriological laboratory of the department of microbiology, virology and immunology of the Bukhara State Medical Institute, and immunological studies were also carried out on the basis of this laboratory. All inspections were carried out on the basis of relevant contracts.A total of 117 adult patients diagnosed with acute and chronic odontogenic osteomyelitis were involved in the research. 76 of them were men (64.96±4.41%) and 41 were women (35.04±4.41%).The gender distribution by group is presented in Figure 1.
 | Figure 1. Results of gender distribution of patients with confirmed chronic (A) and acute (B) odontogenic osteomyelitis, % |
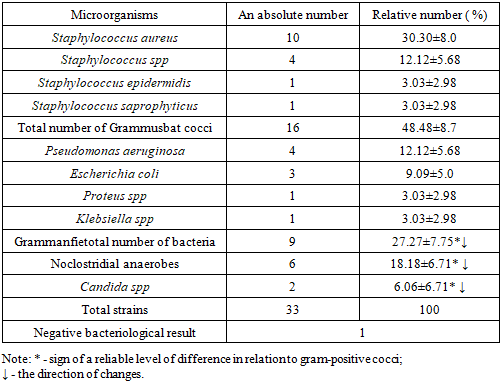
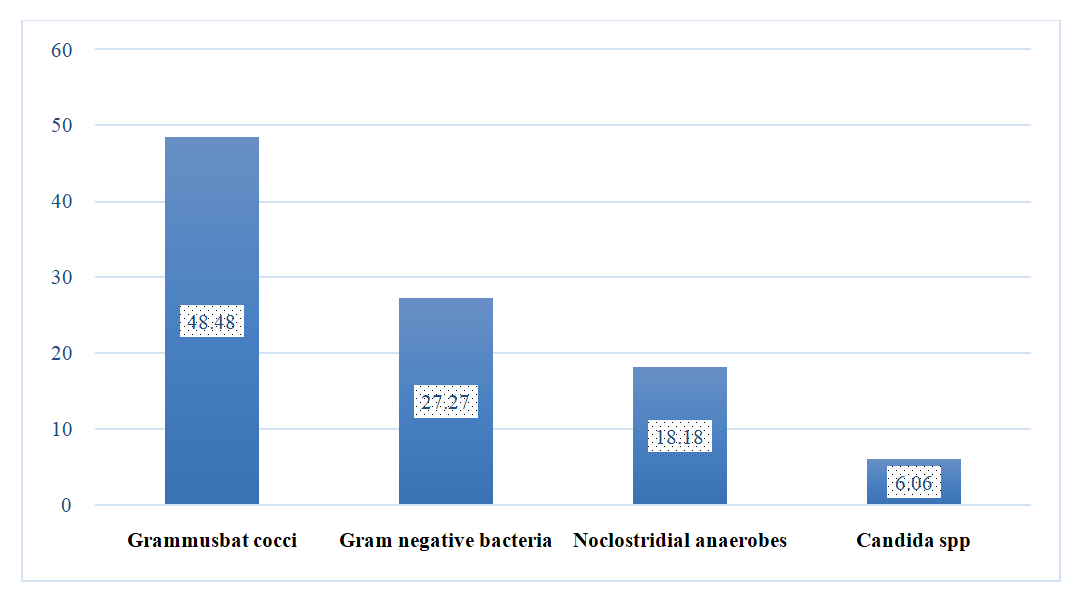 | Figure 2. Indicators of the microbial landscape of acute odontogenic osteomyelitis diagnosed in patients, % |
|
|
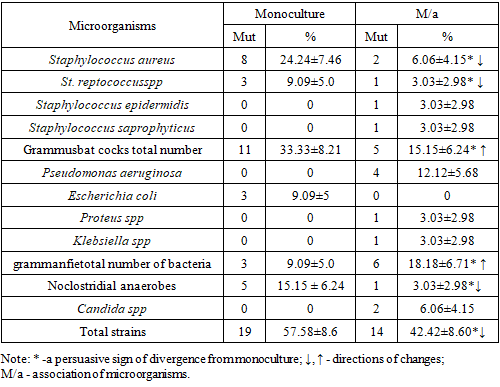
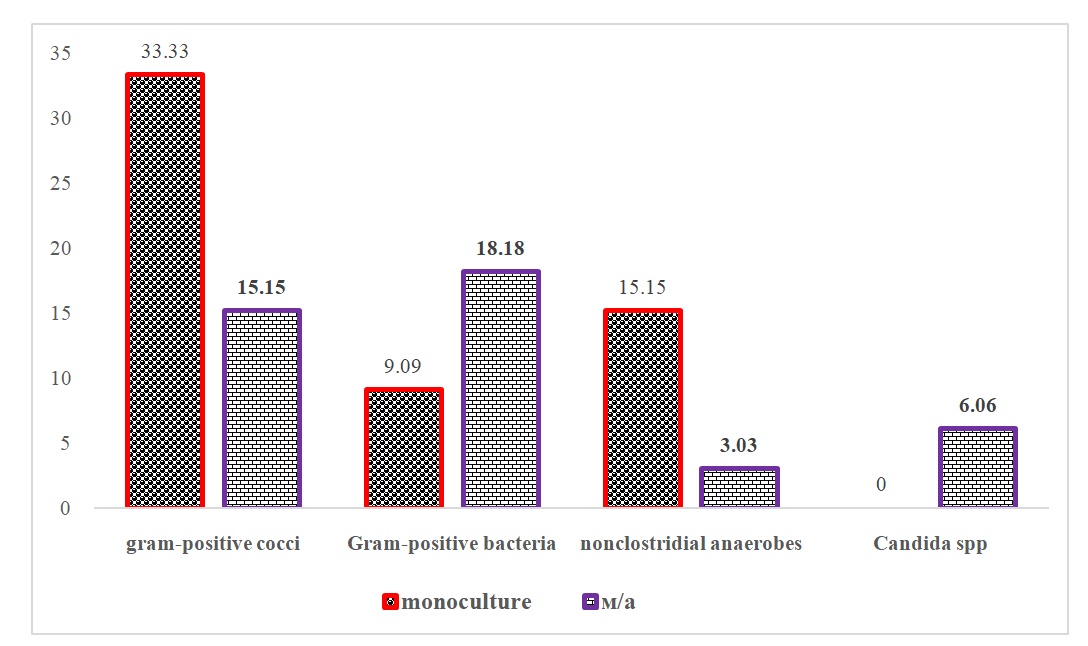 | Figure 3. Indicators of distribution of monoculture and association of microorganisms among causative agents of acute odontogenic osteomyelitis, % |
4. Conclusions
- In the last 10 years (2012-2021), odontogenic osteomyelitis occurred in 2.09-3.61% of cases among other UJS-related cases, the average length of stay in the hospital was 7.7 days, and the performed operations made up 4.22-4.31% of all operative interventions. was determined. It is noteworthy that chronic osteomyelitis was found in 85.47% of cases, acute form in 14.53% of cases, chronic pathology was more common in the lower jaw (62.38%), less in the upper jaw (7.69%), bilateral odontogenic osteomyelitis was found in 15.39% of cases. Symptoms identified in 98.0-100% of cases were confirmed by clinical examinations in 52.94-100.0% of cases.In acute odontogenic osteomyelitis, gram-positive cocci are 1.78 times more common than gram-negative bacteria, 2.67 times more than non-clostridial anaerobes, 8.0 times more than Candida spp, and 1.77 times less common than gram-negative bacteria in chronic odontogenic osteomyelitis. In the chronic form, the microbial spectrum expanded, and representatives of the normal microflora of the oral cavity appeared as the causative agent. This condition has been proven to be important in early diagnosis of diseases, determining the perspective of the end of the course and determining secondary preventive measures in chronic odontogenic osteomyelitis.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML