-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(9): 1340-1342
doi:10.5923/j.ajmms.20231309.36
Received: Aug. 25, 2023; Accepted: Sep. 19, 2023; Published: Sep. 28, 2023

Comparative Evaluation of the Results of Traditional and Endoscopic Correction of Congenital Pyloric Stenosis in Newborns and Infants
Muхtarov J. U., Ergashev B. B., Kamolov Sh. B.
Republican Training, Medical and Methodical Center of Neonatal Surgery in the Republican Perinatal Center, Tashkent Pediatric Medical Institute, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Congenital hypertrophic pyloric stenosis (CHP) is a malformation of the gastrointestinal tract (GIT), characterized by organic narrowing of the pyloric part of the stomach adjacent to the duodenum. The pathogenesis is based on an acute violation of patency in the pyloric region of the stomach due to hypertrophy of the circular fibers of the pyloric muscle, the development of connective tissue, and thickening of the mucosa in the pyloric region.
Keywords: Congenital hypertrophic pyloric stenosis, High intestinal obstruction, Pyloric stomach, Endoscopy, Endoscopic pyloromyotomy, Hypertrophy
Cite this paper: Muхtarov J. U., Ergashev B. B., Kamolov Sh. B., Comparative Evaluation of the Results of Traditional and Endoscopic Correction of Congenital Pyloric Stenosis in Newborns and Infants, American Journal of Medicine and Medical Sciences, Vol. 13 No. 9, 2023, pp. 1340-1342. doi: 10.5923/j.ajmms.20231309.36.
Article Outline
1. Introduction
- CHP is the most common surgical pathology of the neonatal period, requiring immediate surgical treatment. CHP is of great interest to surgeons and pediatricians. In the last decade, a decrease in incidence has been noted in many developed countries, such as the USA, Denmark, Great Britain, Scotland, Germany, and Sweden. In addition, the incidence of births of children with pyloric stenosis may be influenced by racial and ethnic differences. The disease most often occurs in people of the white race, especially of Northern European origin, somewhat less frequently in people of the Negroid race, and very rarely in eastern peoples [3,5].Morphologically, pyloric stenosis is manifested by a thickening of the wall of the pyloric canal up to 3-7 mm (normal 1-2 mm). In healthy children in the first weeks of life, the pylorus has a pink color and a rounded shape, resembling an onion; with this disease, it lengthens and acquires an olive-shaped shape, cartilaginous density and a white color. These changes develop over time. Histologically, hypertrophy of muscle fibers (mainly the circular layer), thickening of connective tissue septa, edema, and subsequently sclerosis of the mucous and submucosal layers with impaired differentiation of connective tissue structures are revealed [1,5].Nursing of the patient after the operation directly depends on his condition before the operation. Immediately after the operation, the child is considered healthy, but concomitant lesions of the mucous membrane of the digestive tract are often not taken into account. The multifactorial model of inheritance of congenital pyloric stenosis suggests a pronounced clinical polymorphism.Prolonged regurgitation and vomiting with functional disorders can also lead to metabolic disorders and the development of malnutrition, therefore the problems of diagnosis and differential diagnosis of congenital hypertrophic pyloric stenosis and pylorospasm are relevant for pediatricians. Vomiting can also be a symptom of a number of other diseases: infectious, inflammatory and metabolic (adrenogenital syndrome, etc.), which requires a careful approach to differential diagnosis. Carrying out an endoscopic examination and comparing data from the compared groups will allow us to identify features and choose the right approach to therapy [2,7].Extensive experience in the surgical treatment of CHP allows us to achieve good long-term results and complete recovery of patients. Over the past decades, significant advances in pediatric surgery have been noted, which have made it possible to perform endoscopic (laparoscopic) operations in pediatric patients whose age exceeds 3 months of age. The extraordinary progress of endosurgery has led to the fact that almost all interventions in childhood have been transformed into minimally invasive procedures, practically no different from those used in the adult patient population [4,6].
2. Objective
- Improvement of treatment outcomes by comparative evaluation and methods of correction of congenital pyloric stenosis in newborns and infants.
3. Materials and Methods
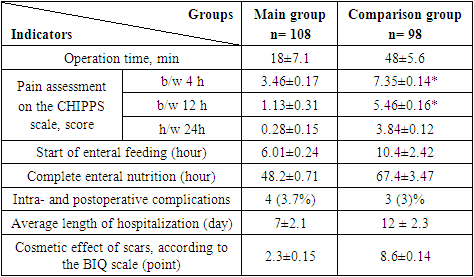
- In the period from 2014 to 2022. 206 patients with congenital pyloric stenosis, aged from 2 weeks to 3 months, were diagnosed and treated at the Republican Educational-Treatment-Methodological Center of Neonatal Surgery at the Russian Orthodox Church, 170 (82.5%) boys, 36 (girls) 17.4%.All patients underwent the following instrumental studies: ultrasound of the abdominal organs - 206 (100%), EchoCG-90 (44%), NSG-206 (100%), X-ray of the abdominal organs - 109 (53%).After instrumental studies, congenital comorbidities were detected in 9(4.3%) patients. Such as heart defects - 4(33.3%): of them ASD-2 (50%), VSD -2(50%); pathology of the kidneys - 3(33.3%) of which hydronephrosis - 2(66.6%), hydrocephalic syndrome 1(11%), as well as Ledd's syndrome (11%).Depending on the severity of exicosis and malnutrition upon admission, we performed infusion therapy.Depending on the method of surgical correction, the patients were divided into 2 groups.The first group of patients was operated on by the traditional method until 2017 - 98 (47.5%) patients. The second group included 108 (52.5%) children who underwent endoscopic pyloromyotomy from 2017 to the present day.First of all, we assessed the duration of surgery, postoperative pain syndrome and noted the time of start of enteral feeding, the time of complete transition to enteral feeding, early postoperative complications and the duration of hospitalization. Postoperative pain was assessed using the CHIPPS (Children's and Infant's Postoperative Pain Scale) scale 4, 12, and 24 hours after pyloromyotomy. The scale is intended for use in newborns and children under 5 years of age (Table 1).
|
4. Results and Discussions
- During the study period, among all patients, the average age at the time of surgical treatment was 28 days (16–64 days).The average duration of the pyloromyotomy operation with the traditional method was 48±5.6 minutes. With the use of laparoscopy, the average duration of the operation was reduced to 18±7.1 minutes. All operated patients began to feed on the first postoperative day. After undergoing laparoscopic surgery, gastrostasis phenomena were the least pronounced in children, which made it possible to start feeding with formula or breast milk 6.01 ± 0.24 hours after surgery. In open surgery, this indicator differed significantly and the start of enteral feeding became possible only after 10.4±2.42 hours (p <0.05) (Table 2).
|
5. Conclusions
- Our study showed a significant advantage of the laparoscopic method compared to the traditional one in terms of the duration of surgical intervention, restoration of gastrointestinal tract functions, severity of postoperative pain syndrome, as well as a decrease in bed days. The endoscopic method makes it possible to minimize the presence of postoperative complications due to the high detail of anatomical structures, magnification and resolution of objects over which surgical manipulations are performed. In terms of cosmetics, the traditional method is inferior to the endoscopic method.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML