-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(9): 1314-1316
doi:10.5923/j.ajmms.20231309.30
Received: Aug. 5, 2023; Accepted: Sep. 3, 2023; Published: Sep. 28, 2023

Surgical Treatment of Colon Cancer in Patients Operated in an Emergency Case
Tulyaganov D. B., Yarov J. B., Shukurov B. I., Mustafaev A. L.
RRCEM "Republican Research Center for Emergency Medicine" of the Ministry of Health of the Republic of Uzbekistan, Str. Little Ring Road 2, Tashkent, Republic of Uzbekistan
Correspondence to: Yarov J. B., RRCEM "Republican Research Center for Emergency Medicine" of the Ministry of Health of the Republic of Uzbekistan, Str. Little Ring Road 2, Tashkent, Republic of Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

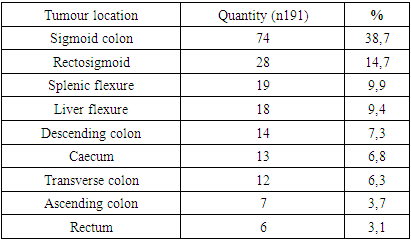
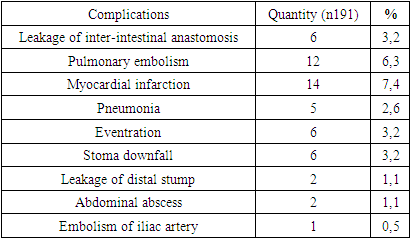
Due to its high prevalence in our country colorectal cancer (CRC) is one of the three malignant tumours along with breast, cervical in women and lung cancer in men, for which screening is promoted by the Ministry of Health. Despite this, CRC screening is not routinely used due to lack of access to health care for the population. According to the literature, between 7% and 40% of patients with CRC undergo emergency surgery, mainly due to obstruction or perforation. Mortality in these patients is high, ranging from 16% to 38%, which is 2 to 4 times higher than in patients undergoing emergency surgery. Objective: to study postoperative complications and mortality in patients with obstructive colonic obstruction of tumour aetiology operated in emergency case. Materials and methods: we analysed 191 patients with acute colonic obstruction of tumour etiology (ACO TE) between January 2012 and December 2022. We analysed the following parameters: age, gender, clinical data, TNM staging, tumour location and types of surgery. Results: There were 36 deaths (19%) during this period. Various postoperative complications were reported in 111 (58.1%) patients. The most common tumour location was sigmoid colon 72 (37.7%), followed by rectosigmoid -28 (14.7%), splenic flexure-19 (9.9%), hepatic flexure -18 (9.4%), caecum-13 (6.8%), transverse colon -12 (6.3%), ascending colon - 7 (3.7%), rectum - 6 (3.1%) patients. Conclusion: high mortality and postoperative complications were observed in patients with colorectal cancer operated as an emergency.
Keywords: Colorectal neoplasms, Intestinal obstruction, Colorectal surgery, Emergency conditions
Cite this paper: Tulyaganov D. B., Yarov J. B., Shukurov B. I., Mustafaev A. L., Surgical Treatment of Colon Cancer in Patients Operated in an Emergency Case, American Journal of Medicine and Medical Sciences, Vol. 13 No. 9, 2023, pp. 1314-1316. doi: 10.5923/j.ajmms.20231309.30.
Article Outline
1. Introduction
- CRC is the third most common cancer in men and second in women [1,13]. When diagnosed at early stages, it has a good prognosis with an overall mortality rate of 8.5% [1]. Mortality and morbidity are relatively low in patients operated on routinely, but patients operated on emergently have a significant increase in these rates as well as a decreased five-year survival [2-4]. The most common clinical presentation in patients with CRC admitted to the emergency department of surgery is acute intestinal obstruction [5,15]. Approximately 10-19% of patients with CRC are expected to develop obstruction at some point in the natural course of the disease [6,14]. This condition is a risk factor for worsening prognosis, mortality in the immediate postoperative period and ranges from 15 to 30% compared to elective patients (1% to 5%) [7,8]. This fact is explained not only by the worsening of the clinical condition of patients due to the obstructive condition in emergency, but also by the progression of the disease. The most commonly used surgical technique in patients undergoing urgent surgery for CRC is the Hartmann operation, especially in patients at high surgical risk [9]. However, this technique causes a number of problems both psychosocial and colostomy related. In addition, it requires another surgical procedure to restore intestinal transit [10]. Although this type of cancer has a relatively favourable prognosis, its overall mortality rate remains high [11], especially among patients operated in emergency case [8]. This reflects a failed screening policy for CRC, with diagnosis often being made at late stages, with complications such as bowel obstruction [12].The aim - is to study the high mortality and postoperative complications and to more actively introduce modern minimally invasive bowel decompression techniques into practice.
2. Materials and Methods
- 191 patients diagnosed with CRC who underwent emergency surgery were treated at the RRCEMS from January 2012 to December 2022. We excluded patients operated for colonic tumor decay or perforation due to other diseases or tumours not confirmed by anatomopathological examination. The following parameters were analysed: age, sex, clinical data, tumour location, type of surgery (curative or palliative), TNM staging, presence of metastases, and primary bowel repair. The main outcomes were death and postoperative complications in the postoperative period. All data were collected and entered into a customised data collection form and MS Excel® spreadsheet. Quantitative parameters are presented as mean ± standard deviation and qualitative parameters are presented as frequency and percentage.
3. Results and Discussion
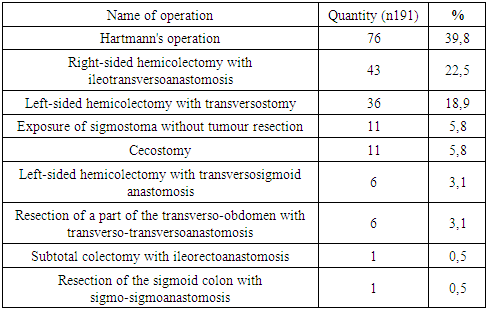
- The patients were predominantly male 98 (51.3%) and 93 (48.7%) females. The mean age was 63.4±14.7 years. The most frequent clinical presentation on admission was pain (100%), followed by nausea (93.7%) and vomiting (78%) and absence of stool (63.3%). Also constipation in 134 (70.2%) patients and weight loss -113 (59.2%). Regarding TNM staging, all patients had stage IV. All patients at admission, along with general clinical and laboratory methods of examination, a review radiography of abdominal cavity organs was performed. This allowed to detect fluid and gas levels in the colon in 74 (38.8%) patients with clinical manifestations of ACO on admission. On radiographs in 73(38,2%) patients small intestinal levels were noted, in 35(18,32%) patients ileum and colonic intestinal levels were detected, in 8(4,2%) patients pneumatosis of the intestine was detected. It should be noted that to clarify the tumour localisation in 110(57,6%) of 191 patients it was necessary to additionally perform irrigoscopy, due to the fact that these patients had only indirect signs of obstruction in the right parts of the colon. Intestinal ultrasound was performed in all patients: 166(86,9%) patients showed bowel dilation, peristalsis was not detected in 42(22%), pendulous bowel movement was detected in 88(46%). The tumour locations are presented in Table 1.
|
|
|
4. Conclusions
- Our study allowed us to make sure that mortality and postoperative complications among patients with CRC operated in emergency procedure are still quite high, and the disease manifests itself at late stages. This fact requires strengthening of measures on early diagnostics of this disease and its timely treatment. It is necessary to introduce more actively modern methods of minimally invasive intestinal decompression in ACO, which will potentially contribute to the reduction of the number of postoperative complications and lethality. In this respect, the rapidly developing and widely spreading technique of stenting the tumour-obstructed part of the colon is promising.
Information about the Source of Support in the Form of Grants, Equipment, Drugs
- The work was carried out in accordance with the plan of scientific research of the Republican Scientific Center for Emergency Medical Aid of the Republic of Uzbekistan. The authors did not receive financial support from drug manufacturing companies.
Conflict of Interest
- The authors declare that there is no conflict of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML