-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(9): 1309-1313
doi:10.5923/j.ajmms.20231309.29
Received: Apr. 5, 2023; Accepted: May 25, 2023; Published: Sep. 28, 2023

Assessment of the Efficiency of Methods of Diagnosis of Different Types of Polyangiitis Granulematosis
Berdieva D. U.1, Rizamukhamedova M. Z.1, Tashpulatova M. M.1, Ziyayeva F. K.1, Nurmukhamedova N. S.2, Ibragimova N. X.3
1Department of Faculty and Hospital Therapy №1 with Course of Professional Pathology of Tashkent Medical Academy of Uzbekistan
2Department of Internal Disease №2 with Endocrinology of Tashkent Medical Academy of Uzbekistan
3PhD, Head of Military Polyclinic of Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Early diagnosis of polyangiitis granulomatosis (PAG) is a difficult clinical task and requires a thorough examination of the patient using modern research methods to identify pathognomonic symptoms. With rhinoscopy, laryngoscopy, nasopharyngeal cavity and computed tomography of the lungs, it is necessary to purposefully look for damage to the respiratory tract, because for a long time the disease can be asymptomatic or accompanied by little clinical symptoms. In only 50% of patients, the diagnosis is made within the first 3-6 months from the onset of the disease, and in 7%, PAG remains undiagnosed for 5-16 years from the onset of the first symptoms. In the active period of the disease, non-specific signs are revealed in the laboratory examination: normochromic anemia, thrombocytosis, neutrophilic leukocytosis and increased ESR, rheumatoid factor, positivity of C-reactive protein. In the clinical analysis of urine: hematuria, erythrocyte cylinders, proteinuria. Along with urinary syndrome, azotemic indicators increase and glomerular filtration rate rapidly decreases.
Keywords: Granulomatosis with polyangiitis, Diagnosis, ANСA
Cite this paper: Berdieva D. U., Rizamukhamedova M. Z., Tashpulatova M. M., Ziyayeva F. K., Nurmukhamedova N. S., Ibragimova N. X., Assessment of the Efficiency of Methods of Diagnosis of Different Types of Polyangiitis Granulematosis, American Journal of Medicine and Medical Sciences, Vol. 13 No. 9, 2023, pp. 1309-1313. doi: 10.5923/j.ajmms.20231309.29.
1. Introduction
- ANCA is a group of immunoglobulin G (IgG) antibodies directed against the cytoplasm of neutrophil granulocytes and monocytes, whose presence in blood serum can be detected by indirect immunofluorescence. Antigens to proteinase 3 (PR3) and myeloperoxidase (MPO) are detected in the PAG. ANCA against these antigens are therefore called PR3-ANCA and MPO-ANCA. Identification of ANCA is important. Immunofluorescence and enzyme immunoassays are widely used to detect ANCA among serological methods. Antibodies specific to proteinase-3 and myeloperoxidase in the presence of neutrophils conjugated with ethanol produce different flashes: they are C-ANCA (cytoplasmic antineutrophil cytoplasmic antibodies) and p-ANCA (perinuclear antineutrophil cytoplasmic antibodies). C-ANCA is mainly associated with sera harboring PR3-ANCA and is specific (>90%) for PAG. C-ANCA has 91% sensitivity and 99% specificity for active GPA [1-7,12]. At the same time, ANCA is an important diagnostic marker of PAG and is not of high value for monitoring the activity of the disease, because they can be in the blood serum during the period of complete clinical remission and may not be detected in the relapse of the disease despite the high activity of vasculitis. Although high activity of ANCA is widespread in the PAG, ANCA may not be the main factor in the development of the disease [8-11,13]. In systemic PAG, ANCA is found in approximately 90% of patienC, and in 80-95% of these patients, antibodies are directed against PR3. C-ANCA has 91% sensitivity and 99% specificity for active GPA.
2. Purpose
- To evaluate the effectiveness of methods of diagnosis of various variants of polyangiitis granulomatosis.
3. Materials and Methods
- 60 patients with PAG who were treated in inpatient conditions in the rheumatology and cardiorheumatology department of the multidisciplinary clinic of the Tashkent Medical Academy in 2018-2022 and were observed and treated in the outpatient department of the arthrological IATC department were taken as the object of the study.As the subject of the study, patients' blood serum, x-ray and ultrasound methods, as well as materials for determining the level of disease activity (BVAS) and vasculitis damage index (VDI) were taken.The research used clinical questionnaire, laboratory analysis, immunological (ANCA), bacteriological inoculation from the nasopharynx, BVAS and VDI indicators, instrumental (MSCT of the nasal cavities and lungs, X-ray examination) and statistical methods.General examination of patients was carried out according to the plan adopted in the clinic. In studying the anamnesis, special attention was paid to the activity of the disease, damage to various organs and systems.In the detailed anamnesis study, the premorbid background more than 6 months before the onset of PAG and before the appearance of symptoms of PAG and the conditions that may have caused its development were analyzed. Manifest symptoms of the first month of the disease, clinical manifestations of the exacerbation phase and subsequent relapses were compared.The BVAS scale (Birmingham Vasculitis Activity Index) was used to assess activity. Remission of the disease was considered to have a score of 1 or less on the VVAS scale, PAG exacerbation was considered to be a score of 2 or more on the VVAS scale. Evaluation of organ damage was performed in all patienC using the VDI index. Damage index assessment takes into account damage to organs observed since the onset of vasculitis. Patients often have additional diseases that occurred before the development of vasculitis, which should not be taken into account.
4. Results
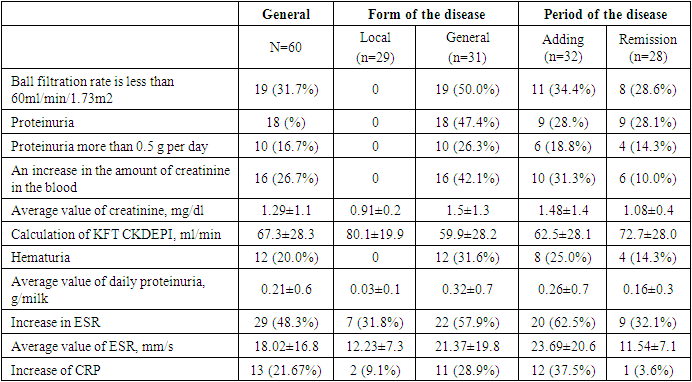
- ESR and C-reactive protein levels were most elevated in patients with PAG exacerbation compared to patients with PAG remission. The main laboratory indicators are presented in Table 1.
|
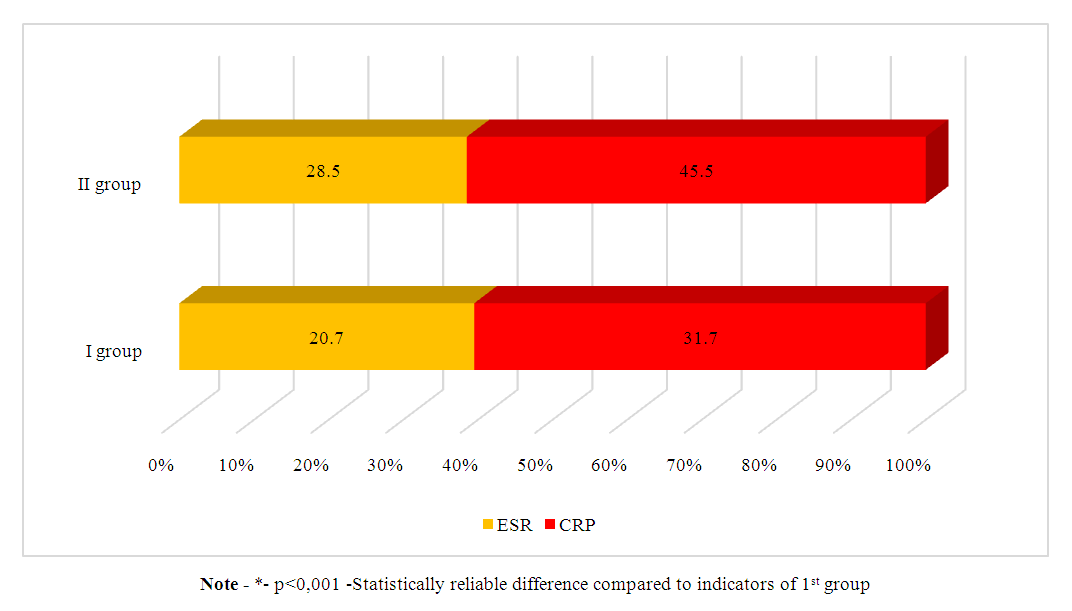 | Picture 1. Changes of amounts of ESR and CRP according to the clinical type of PAG |
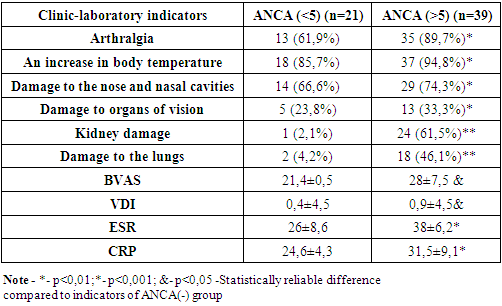
 | Picture 2. ANCA score according to clinical type of PAG |
|
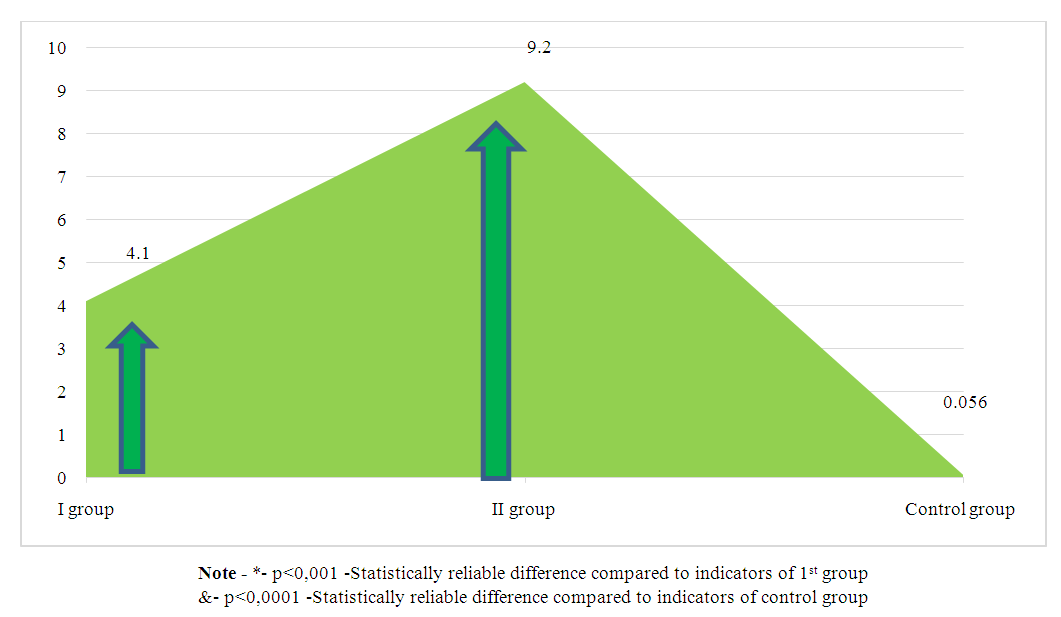
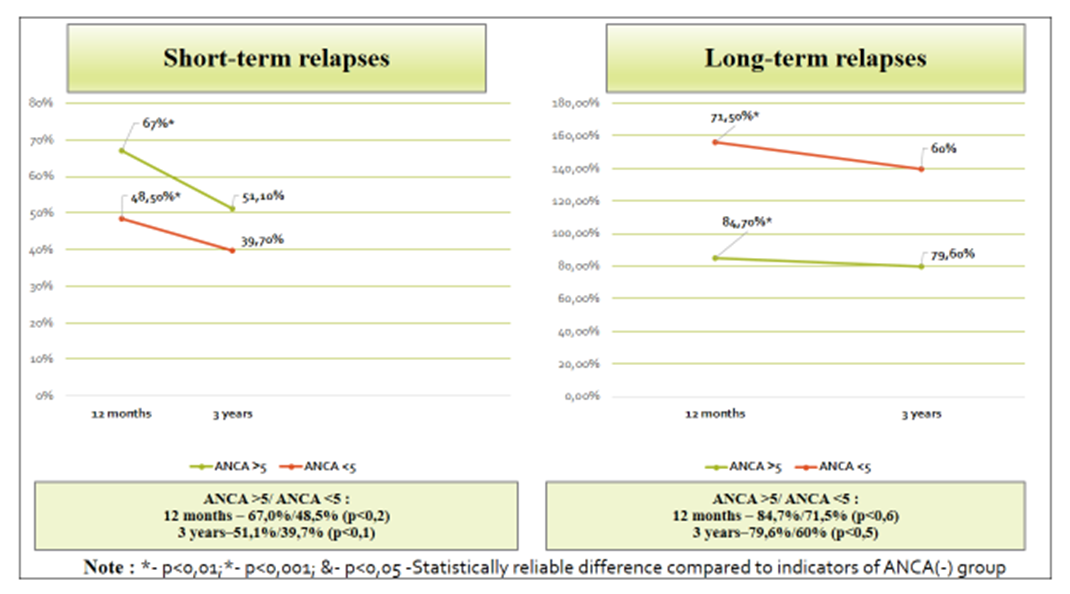 | Picture 3. Assessment of disease relapse in patients with PAG by ANCA titer (%) |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML