-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(9): 1285-1288
doi:10.5923/j.ajmms.20231309.23
Received: Sep. 3, 2023; Accepted: Sep. 16, 2023; Published: Sep. 23, 2023

Comparative Analysis of Reproductive Function Restoration Methods in Women with Uterine Myoma
Kurbanova Surayyo1, Babadjanova Guljakhan2, Sultanov Safronbek3, Karimov Sherzod4, Kadyrov Khairulla4
1Tashkent Medical Academy, Tashkent, Uzbekistan
2Professor, Tashkent Medical Academy, Tashkent, Uzbekistan
3Doctor, Tashkent City Clinical Hospital, Tashkent, Uzbekistan
4Doctors, LLC "IKHLOS DOKTOR MT" Clinic, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In this study, clinical and laboratory analyzes of methods of restoring reproductive function in women with uterine fibroids were studied. For the study, 35 women with uterine fibroids were studied. The age of the respondents was from 32 to 45 years, and the average was 37.6±3.7 years. Complaints of women during the interview: AMK, hyperpolymenorrhea, infertility: primary, secondary, algomenorrhea, women without clinical symptoms. According to the results of the study, it was found that combined oral contraceptives, a progesterone receptor modulator, levonorgestrel-containing intrauterine devices for restoring reproductive function in women with uterine myoma are less effective than uterine artery embolization.
Keywords: Uterine fibroids, Combined oral contraceptives, Progesterone receptor modulator, Levonorgestrel-containing intrauterine device, Uterine artery embolization, Infertility
Cite this paper: Kurbanova Surayyo, Babadjanova Guljakhan, Sultanov Safronbek, Karimov Sherzod, Kadyrov Khairulla, Comparative Analysis of Reproductive Function Restoration Methods in Women with Uterine Myoma, American Journal of Medicine and Medical Sciences, Vol. 13 No. 9, 2023, pp. 1285-1288. doi: 10.5923/j.ajmms.20231309.23.
1. Introduction
- Uterine fibroids are the most common benign tumors of the female genitalia and are monoclonal benign tumors of smooth muscle cells. Uterine fibroids occur in 20–50% of women of reproductive age [1] and can be detected by ultrasound in approximately 80% of African American women and approximately 70% of black American women. [2]. Approximately 175,000 hysterectomies and 20,000 myomectomies are performed to treat fibroids in the United States each year [3].The purpose of this study is to investigate the relationship between fibroids and reproductive function and to review current methods of their management. Each fibroid originates from the vessel wall or the smooth muscles of the uterus. Fibroids arise from genetic exchange in a single myometrial cell and are therefore often described as clonal [4]. Although estrogen can stimulate fibroid development and growth, fibroids can also grow if circulating estrogen levels are low because ovarian and adrenal androgens can be converted. With aromatase activity in fibroid cells to estrogens, the growth of fibroids is also clearly regulated by the hormone progesterone and a number of local growth factors [5], and the genetic basis of fibroid growth may be primarily related to these factors and their receptors. Although most women with uterine fibroids are asymptomatic, many may have significant symptoms such as pelvic and abdominal pressure or pain and excessive bleeding. Other symptoms of fibroids can occur when they affect neighboring organs, such as the bladder [urinary frequency] or the rectum. In reproductive age, fibroids can also be the cause of infertility. Studies have shown that uterine fibroids can be detected in about 5-10% of infertile women, excluding all other causes, only 2-3% of infertility can be attributed to fibroids [6]. In the past, the impact of fibroids on women's reproductive function may have been underestimated, because at that time the diagnosis of fibroids was based on bimanual examination rather than ultrasound or other imaging. In a prospective study of women with unexplained infertility, 11% of women with fibroids became pregnant without intervention, compared to 25% of women without fibroids and 42% of women who underwent laparoscopic myomectomy [7]. Other evidence shows that fibroids can also have a negative effect on the results achieved with the female reproductive function. While some researchers have found that uterine fibroids do not affect the results of women's reproductive function unless they disrupt or displace the uterine cavity, [8], other researchers have noted that women with intramural fibroids have a lower success rate of female reproductive function, especially if they are larger than 5 cm in diameter [9]. There are several mechanisms by which fibroids can adversely affect fertility:- Cervical displacement can reduce the effect of sperm.- Enlargement or deformation of the uterine cavity can interfere with sperm migration and transport.- Obstruction of the proximal fallopian tubes.- By changing the anatomy of the tubo-tubo-ovaries, it interferes with the capture of the egg.- Increased or impaired uterine contractions, which may prevent sperm or embryo transport or embryo implantation.- Disruption or disruption of the endometrium and implantation due to atrophy or venous ectasia over or opposite the submucous fibroid Endometrial blood flow disturbance.- Inflammation of the endometrium or secretion of vasoactive substances.Symptoms of fibroids include pelvic pressure or pain, abdominal distension, urinary or rectal symptoms, and reproductive dysfunction. Abnormal bleeding is common and is usually accompanied by increased or prolonged periods, often with dysmenorrhea. An increase in the size of the uterus is usually detected by clinical examination. The size, number and location of fibroids were determined using ultrasound. Transvaginal ultrasonography combined with sterile saline injection [sonogysterography] can determine whether a centrally located fibroid directly affects the uterine cavity and can be treated with hysteroscopic resection rather than abdominal myomectomy. Intramural or subserosal myomas are more likely to cause pressure, pain, and disruption of adjacent organs, while submucosal and interstitial myomas are often associated with menorrhagia and intermenstrual bleeding and, as mentioned above, may adversely affect reproductive function. Although not usually necessary, computed tomography or magnetic resonance imaging [MRI] may be helpful in planning surgery in selected cases, especially when considering laparoscopic myomectomy [which does not allow palpation to detect deep intramural fibroids]. Infertile women with uterine fibroids should undergo a thorough investigation to rule out other common and possible causes of infertility before concluding that specific treatment options for fibroids are indicated [10]. Hysterosalpingography [GSG] is indicated to evaluate uterine cavity and tubal patency. If a balloon catheter is used to perform hysterosalpingography, it should be removed at the end of the procedure to fully evaluate the cavity. Hysteroscopy is not necessary if the contour of the uterine cavity is normal. Women with unexplained infertility due to uterine fibroids and other causes can be seen. Previously, surgical treatment of asymptomatic fibroids was usually recommended for women whose uterus size exceeded 12 weeks [11]. Several medical treatments have been shown to reduce the size of fibroids and relieve their symptoms. Gonadotropin-releasing hormone [GnRH] agonists cause fibroid shrinkage by inducing hypoestrogenemia and have been the standard medical treatment for fibroids for the past two decades. Androgen therapy with gestrinone or danazol has been effective in small studies, but the frequency of side effects has limited its use. A decrease in the size and symptoms of fibroids was observed after receiving a progesterone receptor modulator [12]. Other agents currently under investigation include selective estrogen and progesterone receptor modulators and aromatase inhibitors, but none are currently approved or recommended for clinical use. Although the size of fibroids can be reduced by about 50% with medical treatment, the uterus usually returns to its pre-treatment size after the medication is stopped. There is no evidence that medical therapy improves fertility. Medical therapy can also delay more effective treatment and is therefore not recommended for treating infertility. The effect of fibroids on reproductive function outcomes is not well defined. Overall, the evidence suggests that fibroids are the primary cause of infertility in a relatively small proportion of women. Fibroids that disrupt the uterine cavity and larger intramural fibroids can adversely affect fertility. Medical treatment of fibroids does not improve infertility. Preoperative medical treatment with a GnRH agonist should be considered for anemic women and women who may be candidates for a less invasive procedure if their fibroid[s] are moderately smaller in size. Myomectomy is a relatively safe surgical procedure associated with few serious complications. However, postoperative adhesions are common after abdominal myomectomy and represent a serious potential risk for subsequent births. Because hysterectomy or amputation are often used in the treatment of fibroids, this not only affects women's reproductive function, but also negatively affects their quality of life. Today, uterine fibroids can be treated without surgery. Uterine artery embolization is a minimally invasive, effective method that is performed under local anesthesia, reduces the symptoms of uterine fibroids and eventually disappears completely, restores the reproductive function of women and restores the quality of life of patients in a short period of time. Therefore, the most effective invasive method for restoring reproductive function and improving the quality of a woman's life today is uterine artery embolization. Uterine artery embolization [BAE] has been used to treat fibroids since the early 1990s. Several small series have reported that uterine artery embolization reduces total uterine volume and total volume of dominant fibroids by 40%–50% in approximately 90% of cases. Up to 80% of women treated with uterine fibroid embolization experienced visual acuity, but the follow-up period was short. Kungil experienced frequent nausea, vomiting, pain, and fever within 48 hours of the procedure. Adverse events after cervical embolization include infectious complications requiring hysterectomy, transcervical removal of myoma, pelvic pain, non-purulent vaginal discharge, delayed work-up, and soiling of leiomyosarcoma, according to reports. Described after embolization of the uterus in women, however, data regarding fertility and pregnancy outcomes after uterine artery embolization are still very limited, and therefore the procedure is not recommended for women planning subsequent pregnancies. [13]. However, for the successful implementation of this method, it is important to correctly select patients, determine indications and contraindications, prepare for the procedure and monitor the health of patients after its implementation.
 | Figure 1. Ultrasound examination (type and size of uterine fibroids are seen) |
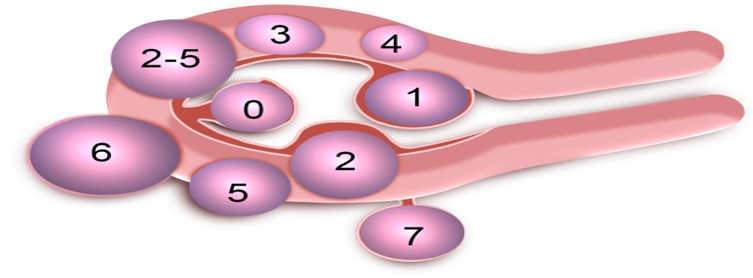 | Figure 2. Leiomyoma sub classification system |
2. Research Materials and Methods
- For our study, a total of 35 women were randomly divided into 4 groups according to treatment methods:Group 1: 9 women taking combined oral contraceptives.Group 2: 3 women receiving a progesterone receptor modulator.Group 3: 3 women using intrauterine devices containing levonorgestrel.Group 4: 20 women who underwent uterine artery embolization.Research methods include:1. Anamnestic and clinical methods.2. Ultrasound examination [type and size of uterine fibroids are seen].3. Checking blood flow in nodular vessels and uterine arteries using Doppler methods, identifying the type of nodules.4. MRI.
3. Results
- Complaints of uterine myoma patients: hyperpolymenorrhea 29% [10 cases], primary infertility 17% [6 cases], secondary infertility 25% [9 cases], algomenorrhea 20% [7 cases], no clinical symptoms observed in 9% [3 cases] women. Types of nodules according to vowel signs: patients with a single nodule were 62.85% [22], patients with multiple nodules were 3715% [13]. According to nodular topography: subserosal nodules 29% [10], submucosal nodules 31% [11], intramural nodules 40% [14] did not occur. Reproductive function was restored in 16 of 35 women with uterine fibroids within a year after treatment: 8% of women using OC [3], 6% of women taking progesterone receptor modulators [2], 3% of women using levonorgestrel intrauterine device [1], women who underwent uterine artery embolization accounted for 29% [10].
4. Conclusions
- Infertility was noted in high rates in the complaints of patients with uterine fibroids. According to the results of the study, it was found that the number of patients with a single nodule was more than that of patients with multiple nodules. According to the nodular topography, the number of patients with intramural nodes in the uterus was high. As a result of the treatment, uterine artery embolization was effective in restoring reproductive function in women who received OC drugs, progesterone receptor modulators, and intrauterine drugs with levonorgestrel, and numerically higher rates were observed.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML