Sadykov Rustam Abrarovich1, Yakubov Farkhod Radjabovich2, Ruzibaev Rashid Yusupovich2, Niyazmetov Sevarbek Bakhtiyorovich2, Sapaev Duschan Shukhratovich2
1Republican Specialized Scientific and Practical Medical Center for Surgery named after academician V.Vakhidov, Tashkent, Uzbekistan
2Urgench Branch of Tashkent Medical Academy, Urgench, Uzbekistan
Correspondence to: Sapaev Duschan Shukhratovich, Urgench Branch of Tashkent Medical Academy, Urgench, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The article presents the results of experimental morphological studies on the comparative evaluation of the effectiveness of wound coatings for aero- and hemostasis. Experimental studies included three series: in vitro, to assess the degree of adhesion of coatings in a humid environment; ex vivo, to study the effectiveness of wound coatings to achieve aerostasis on isolated sheep lungs; in vivo, to study the reaction of biological tissues and lung wound healing in an experiment on laboratory rats. 3 types of coatings were used: Biological glue (based on cyanoacrylate) in liquid form, using a syringe. Collagen sponge (LLC Turon Silk Pharm) size 4x4 cm. Hemostatic implant Hemoben in the form of a powder of cellulose derivatives. In studies, it was found that the new method of aerostasis, along with hemostasis, promotes rapid healing of a wound defect of the lungs, reduces the likelihood of formation of mooring and adhesions in the pleural cavity with the restoration of the functional ability of the operated lung.
Keywords:
Aero- and hemostasis, Experimental morphological study, "Hemoben", Hemostatic effect
Cite this paper: Sadykov Rustam Abrarovich, Yakubov Farkhod Radjabovich, Ruzibaev Rashid Yusupovich, Niyazmetov Sevarbek Bakhtiyorovich, Sapaev Duschan Shukhratovich, Comparative Evaluation of the Effectiveness of Wound Coatings for Aero and Hemostasis – Experimental Morphological Study, American Journal of Medicine and Medical Sciences, Vol. 13 No. 9, 2023, pp. 1277-1284. doi: 10.5923/j.ajmms.20231309.22.
1. Introduction
In modern lung surgery, the issues of achieving sustainable aero- and hemostasis remain an urgent problem. Air discharge after lung resection can reach 25-50% immediately after surgery and up to 20% in the early stages after the intervention [1]. At the same time, air discharge that persists for more than 5 days after surgery is defined as a postoperative complication called prolonged air leakage. The development of this complication can lead to more severe consequences, in particular, to pleural empyema [2,3,4]. This factor also requires prolonged drainage of the pleural cavity, which increases and prolongs postoperative pain, and a decrease in the patient's mobility is accompanied by a high risk of thromboembolic complications [5,6]. Postoperative hemorrhagic complications also contribute significantly to the deterioration of the results of lung operations [7]. This complication may require repeated intervention and, even in the case of conservative resolution, may lead to the need for long-term rehabilitation with an increase in the cost of recovery of the patient [8]. The complexity of preventing the development of hemorrhagic syndrome is associated not only with the surgical intervention itself or the patient's condition, but also with the fact that in thoracic surgery the possibility of using various local hemostatic agents is limited.Taking into account these factors, in this study, an experimental analysis was carried out to assess the features of the use of various implants on a model of lung tissue damage in terms of providing aero- and hemostasis.
2. Materials and Methods of Research
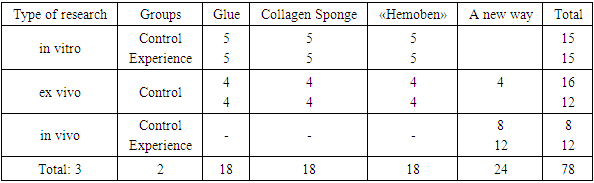
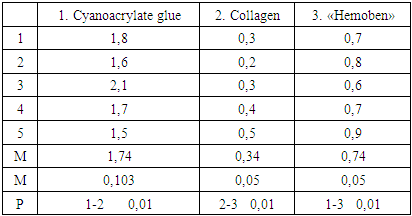
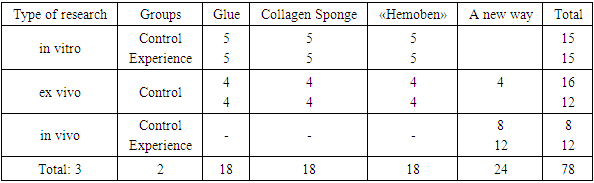
Experimental studies were carried out in the Department of experimental Surgery of the State Institution "Republican Specialized Scientific and Practical Medical Center for Surgery named after academician V.Vakhidov". The research involved three series of experiments:1- in vitro, to assess the degree of adhesion of coatings in a humid environment;2- ex vivo, to study the effectiveness of wound coatings to achieve aerostasis on isolated sheep lungs;3- in vivo, to study the reaction of biological tissues and the healing of lung wounds in an experiment on laboratory rats (Table 1).Table 1. The number and type of studies in the experiment
 |
| |
|
3 types of coatings are used:Biological glue (based on cyanoacrylate) in liquid form, using a syringe. Before applying the lung to the wound, the latter was thoroughly drained of blood, fluid, and reached the dry wound surface. Glue was applied drop by drop until the contacting surfaces of the lung stuck together, followed by control of the degree of air seepage. After the onset of complete polymerization of the adhesive and the cessation of its adhesion to the surrounding tissues (3-7 min), the lung was immersed in a container with phys.with a solution and started the research as indicated above.Collagen sponge (LLC "Turon Silk Pharm") size 4x4 cm. Taking into account the porosity of the sponge, it was pre-pressed to the state of a film with a uniform density. A film was applied to the damaged lung tissue and held under pressure for 10 minutes. Subsequently, the lung was immersed in a container with a solution for conducting experiments.Hemostatic implant "Hemoben" in the form of a powder of cellulose derivatives was evenly applied to the wound surface. Upon contact with wound fluid and blood, polymerization occurs with the formation of a transparent film on the surface of the wound. The polymerization time is 2-3 minutes. Subsequently, the lung was immersed in a container with saline.Determination of the strength parameters of wound coatingsStrips with a width of 20 mm and a length of 70 mm were cut out of the coatings. The tensile strength and elongation at rupture of the "Hemoben" films were determined on the "Zwick" bursting machine (Germany).Determination of the surface structure of filmsThe surface structure of the films was determined using a digital light microscope, and the size of nanocellulose particles was determined using an Agilent Technologies (USA) atomic force microscope.The method of determining the adhesion strength of a composite polymer materialTo determine the adhesion strength of the composite polymer material, we used a standard technique. To do this, a device is taken, which is an equal–shoulder rocker arm, on one of the shoulders of which a glass plate is suspended, on the other - a cup for the load. 1 drop of distilled water is applied to the fixed surface of the glass plate, 10 mg of coating is applied to the surface of the liquid, we cover it with a similar glass plate connected to a rocker arm and place it under a load of 100 g for 10 seconds. Then we place the weights in the cup until the glass plate is completely pasted. The obtained result of the adhesion force (F) in h is calculated by the formula: F = m* q, where m is the mass q is the acceleration of gravity equal to 9.8 n/ kg.The animals were kept in vivarium conditions in accordance with the requirements of GOST ISO 10993-11-2011 on proper conditions for the preparation and observation of experimental animals. The experiments were conducted in strict accordance with the International Ethical and Scientific Quality Standards for Planning and Conducting Animal Research TPC 125-2008 (02040).Experimental studies of the new composite hemostatic material "Hemoben" were conducted in accordance with GOST R ISO 10993-6-2011. The operations were performed under isoflurane inhalation anesthesia with modeling of a lung wound.. The hemo- and aerostatic effect was achieved by applying the HEMOBEN implant. White sexually mature male mongrel rats weighing 198 + 2.7 g were used. Morphological changes were studied on the 1st, 3rd, 7th and 14th days after surgery. Macroscopic and microscopic studies were carried out.Morphological studies were carried out in the laboratory of pathological anatomy of the State Institution "Republican Specialized Scientific and Practical Medical Center for Surgery named after academician V.Vakhidov", as well as the Department of Cell Technologies with electron Microscopy of the Interuniversity Research Laboratory of the Tashkent Medical Academy.Euthanasia was carried out according to the Provisions of ISO 10993 – 2 under general anesthesia. The corpse of an experimental animal was subjected to section. During the experiment, a macroscopic assessment of changes in the abdominal cavity during the autopsy of animals after euthanasia was analyzed.To prepare morphological preparations, the lung tissue, including the wound, was excised and fixed in a 10% solution of neutral formalin. After the fixation period expired, the biopsy was poured into paraffin. Paraffin blocks were made. Serial sections with a thickness of 3-4 microns were made. Histological preparations were stained with hematoxylin and eosin.Experimental studies were conducted in compliance with the rules adopted by the European Convention for the Protection of Vertebrates Used for Experiments or Other Scientific Purposes (ETS N 123), Strasbourg, 03.18.1986.For light microscopy, tissue samples were fixed in a 10% formalin solution on a phosphate buffer. Paraffin sections were stained with hematoxylin and eosin. Light-optical micrographs were obtained using a “DN-300M” microscope coupled with a digital camera and a computer.All micrographs were processed and stored on a computer using Microsoft application programs-"Windows 10 pro".
3. Results and Discussion
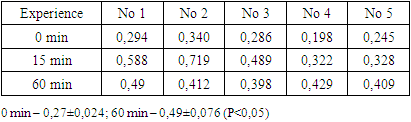
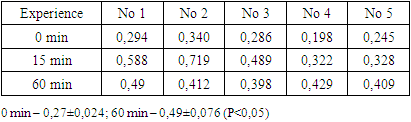
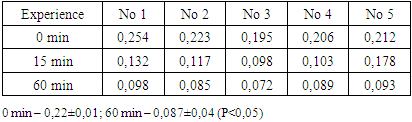
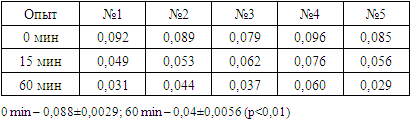
To evaluate the properties of implants, the following physicochemical parameters were studied in vitro: - adhesion; - density; - hemostatic effect.The comparative assessment of the implants for adhesion provided for taking into account some features. In particular, taking into account the peculiarity of the lung tissue, a glass with a moistened surface is taken as the base on which the film is attached. To assess the strength of adhesion on the slide after drying, a fragment of a 1 cm2 polyethylene mesh in the shape of a square was placed. The diameter of the grid cells was 500 microns. Glue was applied from a syringe tube in an amount of 30 mg to a surface up to 1 cm2. The time of complete polymerization of the glue is up to 5 minutes. After that, the glass with an alloyed coating was placed in a container with a saline solution at room temperature. In terms of 1, 15, 30 minutes, the studied glasses were removed and with the help of a bursting machine, the force at which the film moved away from the glass surface was determined. This value was taken as the limiting strength of the adhesion of the biofilm to the glass surface.When using "Hemoben", the time required for adhesion was up to 1 minute, after which the study was carried out in a standard test mode. Collagen sponge, has a weak adhesion force. In this regard, the sponge was pressed against the glass surface for 5 minutes and only after that the study was continued in the prescribed manner. The experiments were carried out five times to obtain more objective information. The results of comparative studies of the adhesion of biofilms are presented in Tables 2-4.Table 2. Adhesion strength of cyanoacrylate medical glue, N/cm²
 |
| |
|
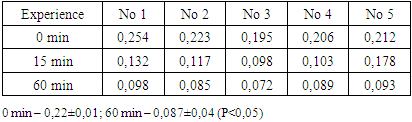
Table 3. Adhesion strength of "Hemoben", N/cm2
 |
| |
|
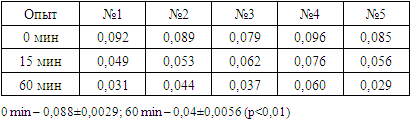
Table 4. The strength of adhesion of the collagen film to the glass, N/cm2
 |
| |
|
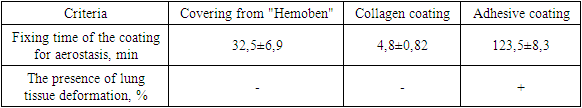
The results of the studies demonstrated that the greatest adhesion took place in the case of biological glue (p<0.05). The smallest with a collagen sponge coating (p<0.01). "Hemoben" occupied an intermediate position (p<0.05). It should be noted that the presence of the coating in saline significantly reduced the strength of adhesion. The degree of adhesion reduction was greatest in the case of collagen (by 2 times) and lowest in the adhesive coating (less than 20%).Density – this indicator characterizes the strength of the film coating, but at the same time reflects the ability to elasticity and the ability to stretch. A comparative analysis of the density of film and adhesive coatings is presented in Table 5.Table 5. Determination of coating density
 |
| |
|
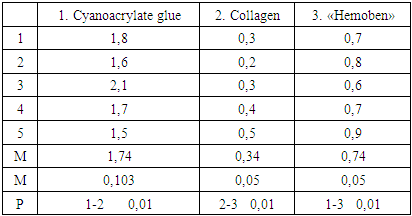
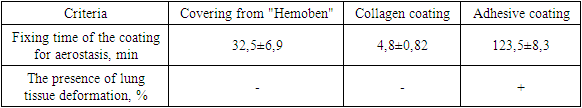
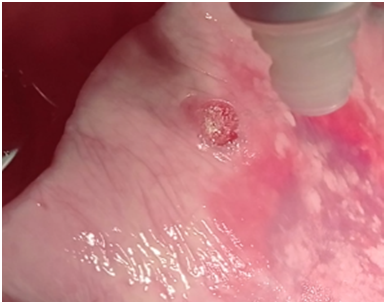
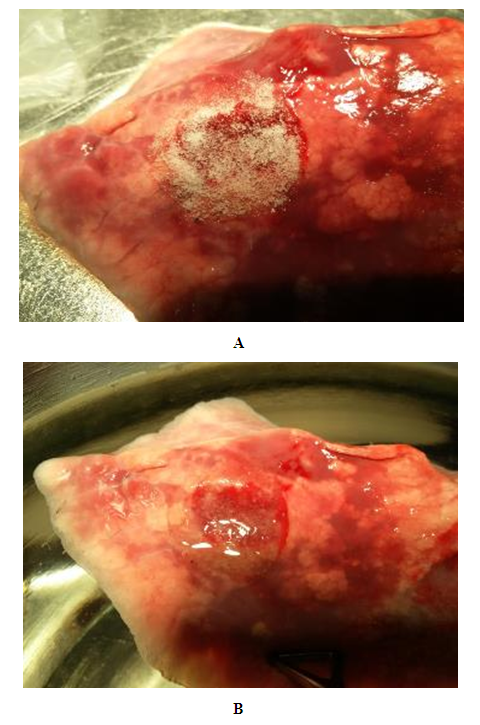
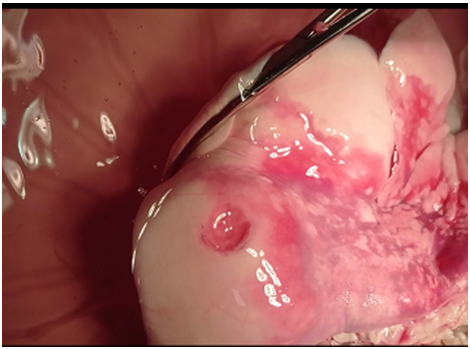
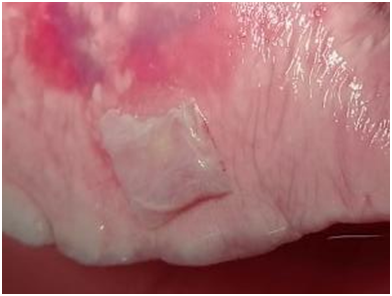
According to the research results, biological glue has the highest density – 1.74, "Hemoben" – 0.74 and the lowest collagen – 0.34. Hence, it should be assumed that the highest density of the adhesive can, with sufficient adhesiveness, provide maximum resistance to air pressure from damaged lung tissue. At the same time, high density implies less elasticity of the coating and sufficient heaviness when applied to a large surface with a thick layer.Ex vivo studies with lung wound modeling.28 studies were conducted, 8 for each type of coatings.The bioclay withstood the standard inhalation pressure with short-term observation in 3 cases out of 4. With long-term observation, the tightness of the lung wound turned out to be consistent in 2 cases out of 4. In 2 cases, air intake occurred due to the glue peeling off the surface of the lung. When using an adhesive coating, deformation of the lung took place in almost all cases (Fig. 1). | Figure 1. Macro-picture of coatings on the surface of a sheep lung wound. After applying the seam and bio-glue |
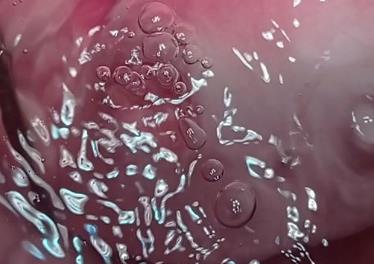
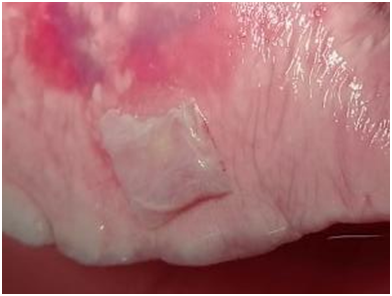
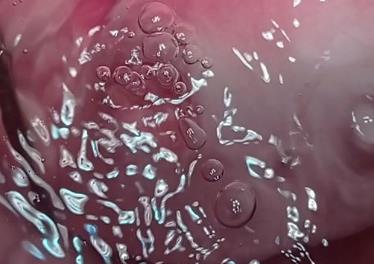
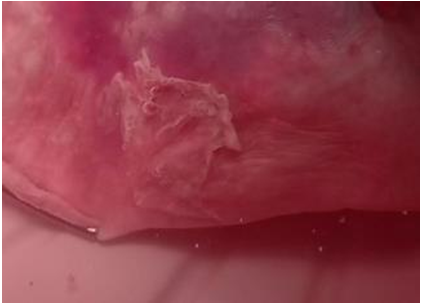
The Hemoben film withstood air pressure during short-term observation in 3 out of 4 cases. During long-term observation, air intake was observed starting from 10 minutes of observations and in a 30-minute period, hermeticism was not achieved in any case. In the short-term observation, the hermeticism is broken due to insufficient adhesion in 1 case, and in the long-term due to the destruction of the coating and its transformation into a thick gel. It should be noted that the decrease in pressure during inspiration created conditions for maintaining hermeticism in later observation periods. Due to its elasticity, the Hemoben film did not prevent the stretching of the lung surface and did not lead to its deformation (Fig. 2).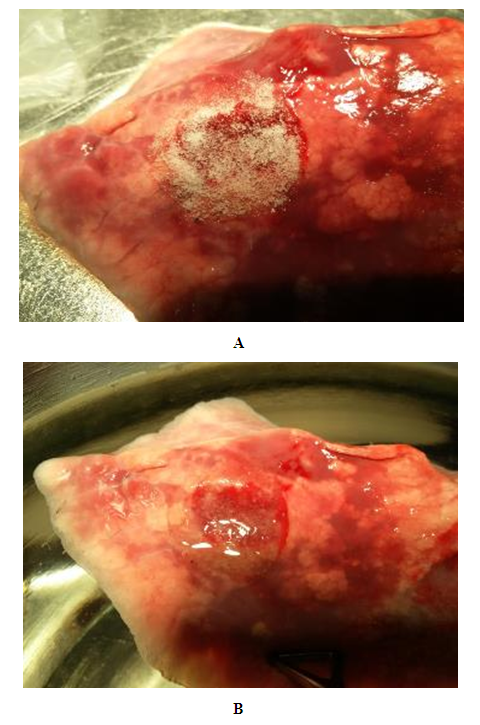 | Figure 2. Macro-picture of coatings on the surface of a sheep lung wound. (A) – the moment of application of the polymer powder; (B) - the formation of a film on the wound surface |
The collagen film maintained the tightness of the lung tissue only for 15 minutes of observation. In subsequent periods, the collagen film slipped and shifted from the wound surface during respiratory movements. Repeated fixation of the film to the wound surface was not effective due to loss of adhesion (Table 6).Table 6. Comparative results of the effectiveness of coatings for aerostasis from lung parenchyma
 |
| |
|
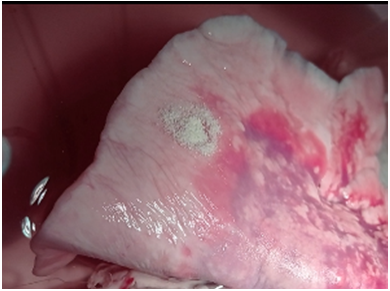
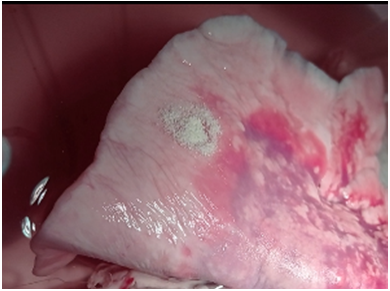
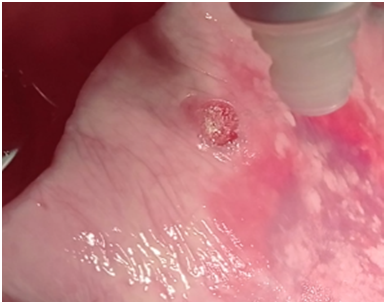
Evaluation of the effectiveness of a new method of coating formation during lung operationsConsidering the positive qualities of the Hemoben wound coating when used for lung surgery: rapid and persistent hemostasis, the formation of a film on the wound surface with high adhesion, elasticity, strength and density in the immediate period after application and the comparative short duration of the effect achieved, which begins to decrease after 15 minutes after application and completely stops within 20-30 minutes we have developed a new method of forming a wound coating on the wound surface of the lungs, which, along with the positive qualities of "Hemoben", performs a long-term effect of aerostasis.To implement the described method, a domestic bioabsorbable surgical hemostatic agent was used from a composite polymer material from cotton cellulose derivatives "Hemoben", developed at the State Institution "Republican Specialized Scientific and Practical Medical Center for Surgery named after academician V.Vakhidov". Local production and the low price of the drug ensures its availability for medical and preventive institutions and for a wide segment of the population.The method is performed as follows.After performing the stages of lung resection with suturing of the bronchial lumen, an aerostasis check is performed, if there is an air supply from the lung parenchyma, then a fine Hemoben powder is applied to the wound surface of the lung using insufflation (particle size no more than 100 microns) at the rate of 200 micrograms of Hemoben per 10 cm2 of the lung parenchyma. Further, 2-3 minutes after the formation of the film, the excess powder is removed by washing with an antiseptic jet for 5 seconds, after which the "Hemoben" powder is reapplied at the rate of 100 micrograms of powder per 10 cm2 of lung parenchyma with the expansion of the powder spraying zone in all directions by 1.5-2.0 cm from the edge of the initially formed film. Then a free flap of the parietal pleura is applied to this area, the latter is pressed tightly for 2 minutes, which contributes to the tight fixation of the pleura to the wound surface. The surgical wound is sutured with the drainage tube left (Fig. 3-8).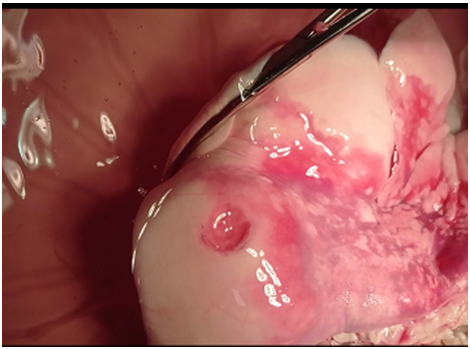 | Figure 3. Formed wound defect of the lung |
 | Figure 4. Intake of air from the damaged lung parenchyma |
 | Figure 5. Hemoben powder is applied to the lung defect |
 | Figure 6. Formation of the "Hemoben" film on a wound defect of the lung |
 | Figure 7. A free pleural flap fixed to a wound defect |
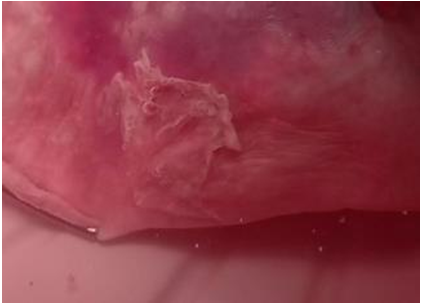 | Figure 8. Experience. Tightness of the aerostasis using a pleural flap on the background of artificial lung ventilation after 30 minutes |
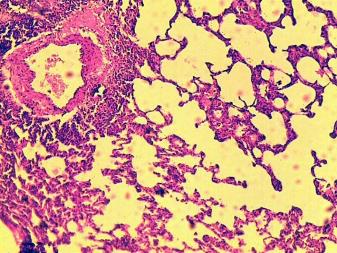
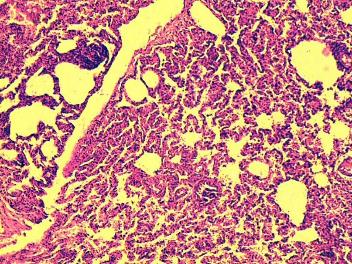
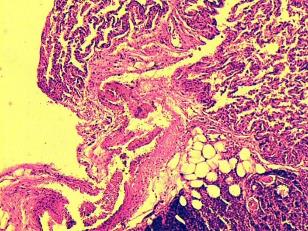
Applying a free pleural flap to the wound surface of the lung provides temporary hemostasis until the lung is immersed in a saline solution. However, after immersion in water, the detachment of the pleural flap occurs even without air supply to the lungs.In ex vivo studies, it was found that due to the high adhesion of the Hemoben powder, the free pleural flap is well fixed to the wound surface and provides complete aerostasis. When the lung is placed in a saline solution and a ventilator is performed, the pleural flap does not shift, air intake is not noted. At the same time, attention is drawn to the good extensibility of the pleural flap, in studies there were no cases of the formation of a "sail" due to the intake of air under the pleural flap. The pleural flap prevented the dissolution of the Hemoben film, thereby short-term aerostasis when using only Hemoben powder became long-term and the engraftment of the flap to the wound surface prevents the formation of adhesions.Data from in vivo studiesTo evaluate the effectiveness of a new method of hemo- and aerostasis using “HEMOBEN” powder and a free pleural flap in vivo, experiments were conducted on mature used white rats weighing 220-280 g. The method of application was identical. In the control group, hemostasis was achieved using gauze balls.In vivo studies have found that the new method of aerostasis, along with hemostasis, promotes rapid healing of a wound defect of the lungs, reduces the likelihood of formation of mooring and adhesions in the pleural cavity with the restoration of the functional ability of the operated lung. When attaching a part of the pleura taken for aerostasis to the area of lung damage, a dense fusion occurs under the influence of powder, resulting in stable aerostasis. The reconstruction of the damaged tissue in the wound area under the action of static aerostasis is manifested by obvious morphological signs, starting from the 3rd day of the experiment and ending with the 7th day (Fig. 9-10). The detection of homogeneous masses in the spaces of injured alveoli is a sign of persistent hemostasis in the area of damage. In the control group, the different level of adhesions between the lung injury zone and the pleural cavity persisted up to 14 days of the experiment, depending on the injury zone. In the experimental group, adhesions between the parietal pleura in the area of injury and the parietal pleura in the chest were not observed (Fig. 11-12).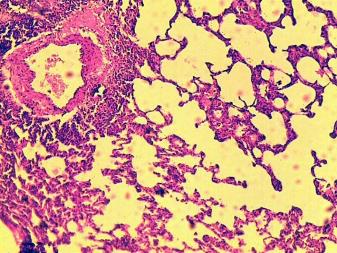 | Figure 9. Adhesions between lung injury and pleura. Reduction of the lumen of the alveoli of the lung. The control group is 7 days old. Colored by hematoxylin-eosin 10х10 |
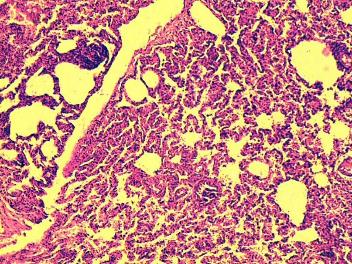 | Figure 10. A section of the lung covered with pleura. Restoration of damaged alveoli and bronchioles. An experienced group. 7 days. Colored by hematoxylin-eosin 10х2 |
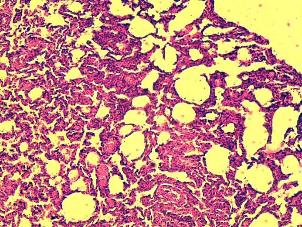
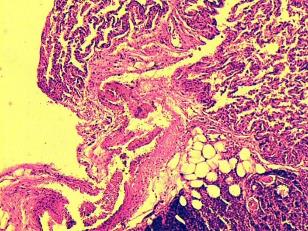 | Figure 11. The formation of connective tissue in the area of lung damage and areas of adhesions is determined. The control group. 14 days. Colored by hematoxylin-eosin 10х10 |
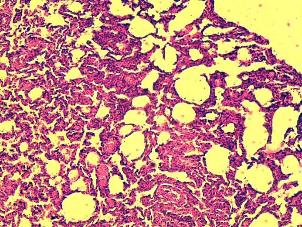 | Figure 12. The area of the injured lung. Normalization of the structure of the alveoli. An experienced group. 14 days. Colored by hematoxylin-eosin 10х10 |
Thus, in vitro, ex vivo and in vivo studies, it was found that the new method of aerostasis, along with hemostasis, promotes rapid healing of a wound defect of the lungs, reduces the likelihood of formation of mooring and adhesions in the pleural cavity with the restoration of the functional ability of the operated lung.
4. Conclusions
The problem of aerostasis after surgical interventions on the lungs remains unresolved. Methods of achieving aerostasis must meet many requirements, among which the most important is biological compatibility, fast and stable aerostasis, the coating should not interfere with the excursion of the lungs. The durability of the coating is of great importance. Conducting experiments on laboratory animals is a certain difficulty, since lung operations are traumatic and performing a large number of comparative studies is a difficult problem to achieve. In this regard, we have conducted in vitro, ex vivo and in vivo studies.In vitro studies have found that:- the greatest adhesiveness and strength, as well as durability, provided that the test sample is immersed in water, is achieved using biological glue;- the next value for adhesion was achieved by the Hemoben coating, however, the degree of adhesion strongly depended on the time the coating was in water because the drug is water-soluble;the weakest coating to reach the balloon was a collagen sponge, which has weak adhesion, and also easily slips off when the sample is immersed in water.In ex vivo experiments, sheep lungs were used, which in their physiological and anatomical parameters correspond to human lungs. The test of the effectiveness of the coatings showed that the formation of a lung wound and the subsequent artificial ventilation of the lungs with immersion of the lungs in a saline solution bring the experiment closer to clinical conditions to a greater extent. These studies have confirmed the results of in vitro studies, however:- the use of an adhesive coating led to deformation of the lung, limiting its excursion, and also required a significant amount of glue to achieve a film coating on the wound surface;- the durability of the aerostasis turned out to be the highest when using cyanoacrylate glue. However, it should be taken into account the fact that the glue becomes glassy and does not dissolve, as a result it becomes a foreign body that contributes to infection of the wound;- Hemoben powder quickly forms a dense and effective coating on the surface of the lung wound with the achievement of complete hemo- and aerostasis, however, the effect was short-lived due to the solubility of Hemoben in water;- the collagen coating proved ineffective in achieving aerostasis from the lung wound.The new method of aerostasis consisted in attaching a light free flap of the parietal pleura to the wound surface. Moreover, its fixation was ensured due to the high adhesive ability of the Hemoben powder. Ex vivo studies have demonstrated the high efficiency of the new method, which is characterized by the rapid formation of the coating within 1 minute, whereas the adhesive coating is formed within 5-7 minutes. The advantage is also the ability to form a coating in a humid environment of tissues, which is unacceptable in the case of using biological glue. The next advantage is the elasticity of the coating, which does not interfere with the excursion of the lungs and does not deform the tissues. The durability of the coating is ensured by the fact that the fixed free flap of the pleura prevents the penetration of fluid onto the wound surface and the dissolution of the Hemoben coating.In vivo studies have found that:- the new method of aerostasis, along with hemostasis, promotes rapid healing of a wound defect of the lungs, reduces the likelihood of formation of mooring and adhesions in the pleural cavity with the restoration of the functional ability of the operated lung;- when attaching a part of the pleura taken for aerostasis to the area of lung damage, a dense fusion occurs under the influence of powder, resulting in stable aerostasis. The reconstruction of the damaged tissue in the wound area under the influence of static aerostasis is manifested by obvious morphological signs, starting from the 3rd day of the experiment and ending with the 7th day;- the detection of homogeneous masses in the spaces of injured alveoli is a sign of persistent hemostasis in the area of damage;- in the control group, the different level of adhesions between the lung injury zone and the pleural cavity persisted up to 14 days of the experiment, depending on the injury zone. In the experimental group, adhesions between the parietal pleura in the area of injury and the parietal pleura in the chest were not observed. The main reason for this is that the pleura in the affected area is the same histological tissue, and the anatomical and physiological state is restored. As a result, there is no spike formation between them.
References
| [1] | Есаков Ю.С., Жестков К.Г., Кармазановский Г.Г., Макеева-Малиновская Н.Ю. Факторы риска недостаточности аэростаза при резекции легкого. Хирургия 7, 2014. С – 38-43. |
| [2] | Bronstein ME, Koo DC, Weigel TL. Management of air leaks post-surgical lung resection. Ann Transl Med. 2019 Aug; 7(15): 361. doi: 10.21037/atm.2019.04.30. PMID: 31516907; PMCID: PMC6712254. |
| [3] | Yakubov F.R., Sapaev D.S., & Niyazmetov S.B. (2023). The treatment of the results of pleural empyema complicated with bronchopleural fistula. Research Journal of Trauma and Disability Studies, 2(4), 241–246. Retrieved from http://journals.academiczone.net/index.php/rjtds/article/view/748. |
| [4] | Якубов Ф.Р., Сапаев Д.Ш., Ниязметов С.Б. Бронхоплеврал оқма билан асоратланган плевра эмпиемасини даволаш натижалари // Проблемы биологии и медицины. - 2023. №3. Том. 3. - С. 237-240. |
| [5] | Dugan KC, Laxmanan B, Murgu S, et al. Management of persistent air leaks. Chest 2017; 152: 417-23. 10.1016/j.chest.2017.02.020. |
| [6] | Якубов Ф.Р, Сапаев Д.Ш, & Ниязметов С.Н. (2023). Ўпканинг анатомик резекциясидан кейинги асоратлар. Journal of Universal Science Research, 1(5), 10–12. Retrieved from https://universalpublishings.com/index.php/jusr/article/view/602. |
| [7] | Iyama S, Sato T, Murase K, et al. Successful treatment of fibrin glue sealant for pneumothorax with chronic GVHD resistant to autologous blood patch pleurodesis. Intern Med 2012; 51: 2011-4. 10.2169/internalmedicine.51.7355. |
| [8] | Broekema FI, van Oeveren W, Boerendonk A, Sharma PK, Bos RR. Hemostatic action of polyurethane foam with 55% polyethylene glycol compared to collagen and gelatin. Biomed Mater Eng. 2016; 27 (2-3): 149-59. |




 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML