-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(9): 1270-1273
doi:10.5923/j.ajmms.20231309.20
Received: Sep. 7, 2023; Accepted: Sep. 19, 2023; Published: Sep. 23, 2023

Dynamics of Cytokine Profile in Young Children with Acute Severe Pneumonia on the Background of Acute Herpetic Stomatitis before and after Treatment
Doniyor Abdullaev1, Zaynitdin Kamalov2, Akhmatdjan Aliev3
1Andijan State Medical Institute, Andijan, Uzbekistan
2Institute of Immunology and Human Genomics, Tashkent, Uzbekistan
3Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The purpose of this study was to study the content of pro- tumor necrosis factor alpha (TNFa) and anti-inflammatory interleukin-10 (IL-10) cytokines in peripheral blood serum in dynamics before and after conventional and combined therapy in young children with acute pneumonia on the background of acute herpetic stomatitis (OGS). Youngsters were included in the present study. The 1st group consisted of 28 young children with acute bacterial pneumonia without OGS, the 2nd included 54 children with acute pneumonia with OGS. The control group (consisted of 22 practically healthy children of analogical age). The analysis, clinical observations, X-ray, immunological. An imbalance in the production of pro- and anti-inflammatory cytokines has been established in all groups with OGS, leading to a weakening of anti-infective protection and the progression of infection. A comparative assessment of the effectiveness of traditional therapy and the significance of the use of the drug Cycloferon was carried out.
Keywords: Young children, Pneumonia, Stomatitis, Herpes simplex virus, Cytokines, Immunity
Cite this paper: Doniyor Abdullaev, Zaynitdin Kamalov, Akhmatdjan Aliev, Dynamics of Cytokine Profile in Young Children with Acute Severe Pneumonia on the Background of Acute Herpetic Stomatitis before and after Treatment, American Journal of Medicine and Medical Sciences, Vol. 13 No. 9, 2023, pp. 1270-1273. doi: 10.5923/j.ajmms.20231309.20.
1. Introduction
- Respiratory diseases occupy a leading place in the structure of the overall morbidity of children. Despite great achievements in the fight against this pathology, the incidence of pneumonia in children of the first three years of life remains widespread, the pneumonic process often proceeds heavily, sometimes ends fatally.An unfavorable background for the course of the pneumonic process in young children is rickets, protein-energy deficiency, anemia, dysbiosis, etc. They largely determine the recurrence of pneumonia in a child, the duration of their course, the tendency to exacerbations, relapses and complications.Infection caused by the herpes simplex virus (HSV) is the most common among people (80-95% of the population are lifelong carriers of the virus). Seroepidemiological studies have shown that by the age of 15, about 83% of children are infected with HSV, and at the age of 30 and older, more than 90% of the population have antibodies to HSV of one type or another [2,4].Most people come into contact with the virus in early childhood. The manifestation of primary herpetic infection is more often acute herpetic stomatitis (OGS), the most common in children aged 6 months to 3 years [4]. This is due to the disappearance of antibodies obtained interplacentally from the mother, with the structural features of the oral mucosa, high permeability of histohematological barriers, insufficient activity of local immunity, as well as with frequent natural violations of the integrity of the mucous membrane as a result of teething and microtrauma [3,5].The state of the immune system plays an important role in the occurrence and nature of the course of herpetic infection. The production and secretion of proinflammatory cytokines (interferons, interleukins) belong to the earliest events in HSV infection [8,9] and influence the subsequent specific immune response.The mutually inhibitory effect of cytokines produced by T-helpers of one type on the formation of cytokines by T-helpers of another type is widely known (for example, Th1-cytokines inhibit the formation of Th2-cytokines; and Th1- and Th2-cytokines inhibit the synthesis of Th17-cytokines) [7].Despite the huge amount of research in this direction, today the question of the implementation of the immune response in young children with acute pneumonia against the background of OGS g remains open. In connection with the above, the purpose of this study was to study the content of pro- (TNFa) and anti-inflammatory (IL-10) cytokines in peripheral blood serum in dynamics before and after conventional and combination therapy, in children aged 6 months to 3 years with stomatitis.
2. Material and Methods
- 92 young children were included in the present study. The 1st group consisted of 28 young children with acute bacterial pneumonia without HSV, the 2nd group included 54 children with acute pneumonia with OGS. The control group (consisted of 22 practically healthy children of the same age).Immunological studies in the examined children were conducted in the laboratory of immunoregulation of the Institute of Human Immunology and Genomics of the Academy of Sciences of the Republic of Uzbekistan.The concentration of tumor necrosis factor alpha (TNF) and interleukin-10 (IL-10) in the oral fluid was determined by solid-phase enzyme immunoassay using the test systems of VECTOR-BEST JSC (Russia, Novosibirsk). The quantitative evaluation of the results was carried out by constructing a calibration curve or using a commercial computer program "Microplate manager", reflecting the dependence of the optical density on the concentration for a standard antigen and allowing comparison of the studied samples with it. Statistical processing of the obtained data was carried out using the computer program Statistica 6.0. The reliability of the differences in the average values (p) of the compared indicators was evaluated by the Student's criterion (t).
3. Results and Discussions
- The body's immune response to the virus consists of two phases, where Th1/Th2 activated cells are involved, respectively. In the first phase, interferon production is stimulated and natural killer cells and other immunocompetent cells are activated [5]. Macrophages play a central role in immune defense and are involved in both nonspecific and specific immune responses against HSV infection. They respond to viral infections with rapid secretion of proinflammatory cytokines [7], which include tumor necrosis factor alpha (TNFa), which is important for primary protection.Tumor necrosis factor α (F) is a representative of another family of immunologically significant proteins. The main producers of TNF are monocytes and macrophages. It is also secreted by neutrophils, endothelial and epithelial cells, eosinophils, mast cells, B- and T-lymphocytes when they are involved in the inflammatory process. TNFa is detected in the bloodstream before other pro—inflammatory cytokines - already 20-30 minutes after the induction of inflammation. TNFa is involved in the formation of all major local, as well as some systemic manifestations of inflammation. It activates endothelial cells, stimulates angiogenesis, enhances migration and activates leukocytes [1,7].Significantly elevated serum TNF values were established in all groups of children. Thus, in the group of children without HSV, the range of fluctuations was revealed from 14 to 31 pg/ml with an average value of 23.3±1.05pg/ml (p<0.001), which is almost 2 times, and in the group of children with HSV, the range of fluctuations was from 17 to 39 pg/ml, with an average of 26.8± 0.94 pg/ml (p<0.001), which is almost 2.3 times higher than the control values of 11.7±0.57pg/ml (Fig. 1).
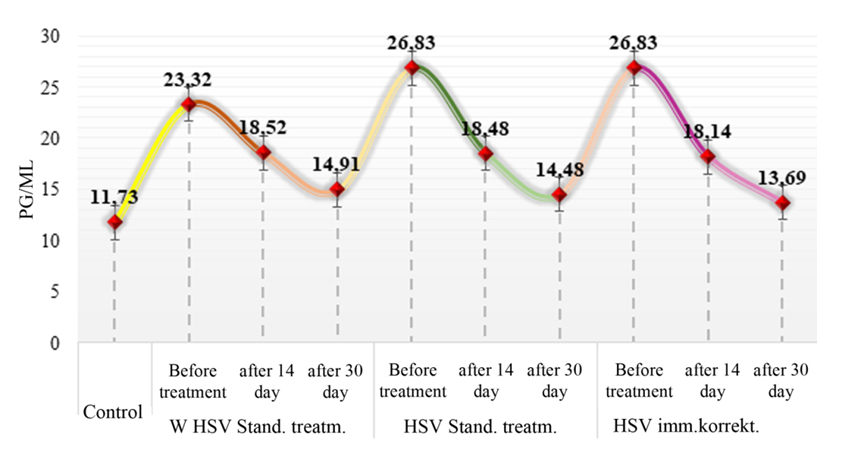 | Figure 1. Dynamics of serum TNF in groups of children before and after treatment |
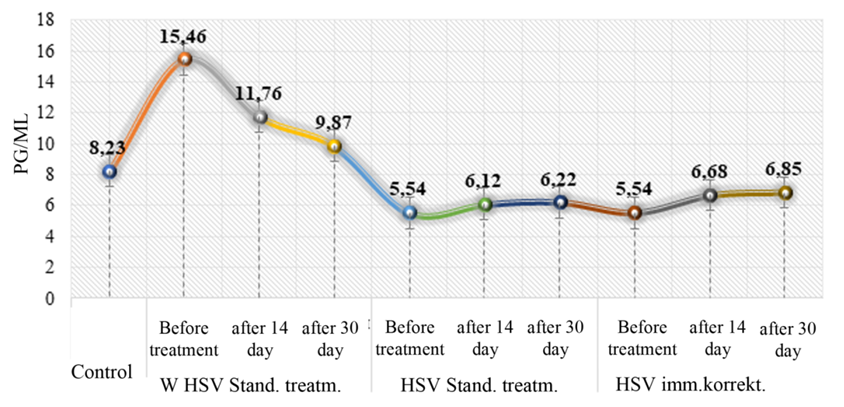 | Figure 2. Dynamics of serum IL-10 in groups of children before and after treatment |
4. Conclusions
- 1. An imbalance of Th1/Th2 cytokine production was established in children with stomatitis with pneumonia of various etiologies before treatment.2. Significantly increased serum TNF content was revealed in all groups of children with stomatitis before treatment.3. The study of IL-10 concentration established multidirectional indicators before treatment in a group of children without MIC and with HSV.4. Analysis of the data obtained after the start of treatment determined that in groups of children without HSV with traditional treatment, the level of TNF and IL-10 decreased.5. Assessment of TNF and IL-10 levels in the group of children with HSV with combined immunocorrecting therapy established a significant decrease in pro-inflammatory and a significant increase in anti-inflammatory cytokines.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML