-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(9): 1265-1269
doi:10.5923/j.ajmms.20231309.19
Received: Sep. 10, 2023; Accepted: Sep. 20, 2023; Published: Sep. 23, 2023

Hirschsprung's Disease: Complexity of Diagnosis and Treatment
S. N. Navruzov, B. S. Navruzov, S. T. Rakhmonov, A. M. Khakimov
Surgical Clinic Named after Yangi Hayat, Uzbekistan, Tashkent, Uzbekistan
Correspondence to: S. N. Navruzov, Surgical Clinic Named after Yangi Hayat, Uzbekistan, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

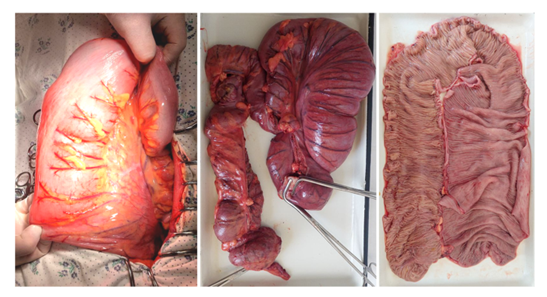
The purpose of this article is to consider the relationship between the basic scientific principles of Hirschsprung's disease and its predisposing factors, disease mechanisms, clinical manifestations, as well as persistent functional problems after surgical correction based on a case from practice. Analysis of the clinical case of a patient admitted to the clinic for differential diagnosis. According to the conducted examinations, the collection of a detailed anamnesis, visual examination of clinical and biochemical laboratory tests with video colonoscopy and irrigography, the patient was diagnosed with a preliminary diagnosis - Hirschsprung's disease? with subsequent surgical intervention in the volume of the BAR with the reduction of the rectum, subsequent examination of macro and microscopic surgical material confirmed the diagnosis, the patient was discharged in a satisfactory condition with nutritional recommendations. The diagnosis of this pathology presents certain difficulties, therefore it is necessary to pay attention to the collection of anamnesis, as well as possible functional disorders that occur due to the absence of the intestinal nervous system during fetal development. It is also necessary to take into account genetic factors and possible hereditary disorders. In childhood, pay attention to asymmetry and bloating, problems with growth, prolonged constipation with the phenomena of enterocolitis.
Keywords: Hirschsprung's disease, Intestinal nervous system, Comb-like cells nervous system, Aganglionic megacolon
Cite this paper: S. N. Navruzov, B. S. Navruzov, S. T. Rakhmonov, A. M. Khakimov, Hirschsprung's Disease: Complexity of Diagnosis and Treatment, American Journal of Medicine and Medical Sciences, Vol. 13 No. 9, 2023, pp. 1265-1269. doi: 10.5923/j.ajmms.20231309.19.
1. Introduction
- Hirschsprung's disease (HD) is a congenital anomaly of the innervation of the lower intestine (usually the colon) resulting in partial or complete functional obstruction. This pathology causes an impaired development of the enteric nervous system, which is caused by defective proliferation, proliferation, differentiation, and survival of neural crest cells, leading to agangliosis in the intestinal wall with the development of the corresponding clinical picture.The neural crest is an embryonic structure that gives rise to a diverse spectrum of cell populations that are the basis of the enteric nervous system. Considering that the etiopathogenetic factor of HD is the pathology of the neural crest, leading to the condition of neurocristopathies [13]. Due to the almost complete absence of ganglia in the affected part of the intestine, there is a functional obstruction, which manifests itself only after birth. This pathology was described in 1886 by the Danish physician Harald Hirschprung, but historically the first mention of this pathology was made in 1691 by the Dutch anatomist and botanist Frederick Ruysch, who described the disease of a 5-year-old girl in his report [2].
2. Epidemiologic Features
- According to available statistical data, the incidence of HD among live births is 1:4400 to 1:7000, males are the most affected with a ratio of 3:1-4:1 to females [1]. Sex variation decreases in subtotal and total forms of the disease and the ratio is 1:2 to 2:1 [8]. In case of suspicion of HD it is always necessary to pay attention to the presence of concomitant possible malformations, one of the early noticeable signs of this pathology is the delay of the first born stool (meconium), if detected, further clinical-instrumental and histologic examination is carried out in order to confirm the diagnosis.Large intestine (LC), the main function of which is evacuatory, when it is violated constipation occurs - delayed, difficult or insufficient emptying, sometimes there may be complications in the form of involuntary fecal discharge (encopresis). The development of chronic constipation may be associated with TC dysfunction, tumor or malformation (BG, dolichosigma). Given the heterogeneity of signs and diseases, there are no accurate statistics on the occurrence of constipation in children [10].This poses a great problem among pediatricians because there are no uniform criteria for assessing the normal frequency of stools, which depends on various factors such as age, feeding of the child, and the nature of the child. There are opinions of researchers who observe constipation in 10-25% of the pediatric population and 3 times more often in preschoolers [6;13]. According to the studies of gastroenterologists, the frequency of constipation among children is 25-70%, and in the presence of various pathological conditions in which there is a delay in psychomotor development, cerebral palsy, they are 50-75% [12]. Among all existing causes of chronic constipation in young children, the most frequent are functional disorders of motor and evacuatory function of the intestinal tract due to discoordination of tonic and propulsive muscle contractions of the intestinal wall. It should be noted that posthypoxic and traumatic damage of the central nervous system (CNS) is of great importance in the formation of constipation, which is characterized by the presence of hypertension-hydrocephalic syndrome with the subsequent development and formation of psycho-emotional and neurogenic disorders associated with impaired function of both the CNS and the autonomic nervous system (ANS) with further damage to humoral systems (kinin, prostoglandin, enteric) that provide motor function of the intestine. One of the causative factors may be morphofunctional immaturity leading to delayed activation of intestinal enzymes; muscle hypotonia observed in children with rickets, as well as the consequences of perinatal hypoxia [11]. Some children may have immunity to cow's milk proteins with the development of food allergy, immaturity of the digestive system, early introduction of complementary foods, and impaired functional activity of the immune system. Functional constipation among preschool children can occur in the violation of defecation as a result of the absence or weakness of the reflex (conditionally reflex, psychogenic constipation). When the act of defecation occurs, there is a thickening of fecal masses, the mucosa of the rectum is traumatized and reactive proctitis, proctosigmoiditis is formed. At the same time, it is worth paying attention to the behavior of the child, who has fear and fear of "sitting on the potty". When the child grows older, they can be alimentary, dyskinetic, psychogenic, conditionally reflexive. One of the main factors of its formation is hypodynamia, which is caused by bed rest in the presence of various congenital malformations [3,15]. On this basis, for practical use, the following classification should be recommended, dividing constipation into organic and functional. If the cause of constipation is organic (HD, dolichosigma), it is recommended to conduct a special examination of the child for accurate differential diagnosis and rational tactics of its treatment - surgical or therapeutic. If the organic lesion of the intestine is excluded, constipation has a functional character, which is most common among young children.
|
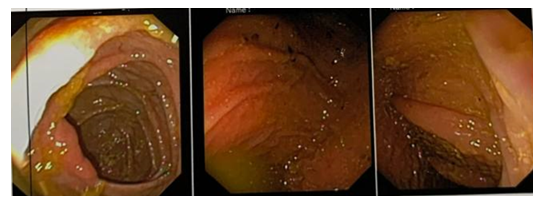
3. Main Diagnostic Measures
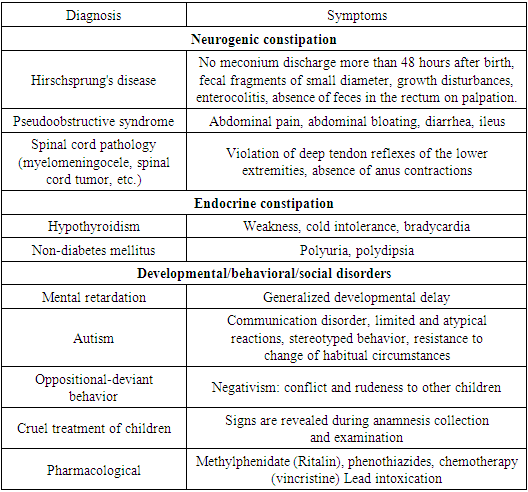
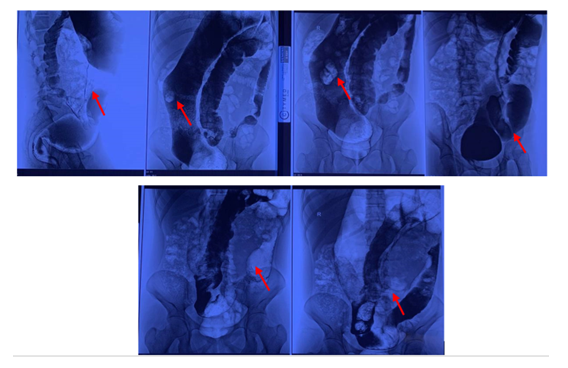
- Irrigography with barium; rectal biopsy; rectal manometry. The diagnosis of the disease should be established at early stages, as the lack of long-term targeted treatment of the disease contributes to the development of EG (toxic megacolon), sometimes leading to immediate lethal outcome. Usually the disease is diagnosed in childhood. In the neonatal period, there are no characteristic signs of HD, therefore radiological studies should be performed within 24 hours after bowel emptying, and if barium is retained in the colon, HD may be suspected. Rectal aspiration biopsy may indicate the absence of ganglion cells. In large centres, rectal monometry may be performed for diagnostic purposes, which helps to detect motor dysfunction due to abnormal innervation. The final diagnosis can be made by biopsy of the rectum (Swenson) or colon to assess the degree of pathology and to decide on the extent of surgical treatment [16,17].Treatment of the disease consists of reconstructive surgery to bring the intestine with normal innervation to the anus with preservation of the anal sphincter. In newborn children this operation is performed in two stages, in the first stage colostomy to the aganglionic segment is performed to decompress the TC, in the second stage, when the child grows up the whole aganglionic part of the colon is resected with the operation of relegation. Some operations are performed laparoscopically, in the absence of contraindications, as well as open access. Usually, the prognosis after surgical intervention is favourable, but there may be chronic motility disorders with constipation, obstruction, or both. As a clinical example, the case history of a patient treated at “Yangi Hayot” private surgical clinic is presented.Patient N.J, 18 years old, came to the clinic with the following complaints: abdominal bloating, delayed stools for more than 4 days, urges for defecation, but no defecation when going to the toilet, pain of a diffuse nature in the abdomen, no vomiting.Anamnes vite: Pregnancy I (only child) was accompanied by multivagina with the presence of inflammatory diseases (salpingo-ophoritis). Term delivery, cesarean section, newborn's condition: weight 2900 g, height 49 cm, Apgar scale 7/10, meconium did not come off. He cried not immediately, was born with umbilical cord entanglement. Genetic diseases are denied, marriage is unrelated. Breastfeeding up to 1 year of age, introduction of complementary food from 4 months, subsequently the history is not aggravated, grew and developed according to age, denies allergic reactions and diseases, had medical withdrawal from vaccinations, which were first received after 3 years of age. Based on the anamnesis, receiving vaccinations contributed to the development of clinical manifestations of the disease, which consisted in the absence of stool for a long time, its constant delay, defecation difficulties, psychomotor disorders (lack of contacts with others, peers, relatives), fear of the dark, tendency to loneliness.Anamnes morbi: sick since the age of 4, but without obvious clinical manifestations from the intestine with characteristic signs of lesions of the nervous system and psyche, the child was observed by a paediatrician, the therapeutic treatment was not received. First applied in August 2022 to a private surgical clinic with complaints of bloating and abdominal pain, absence of stools for a long time, abdominal wall asymmetry, panic fear, diagnosed with coprostasis, intestinal obstruction, was hospitalised in the clinic.The patient underwent diagnostic videocolonoscopy for differential diagnosis. The anal canal is passable, the ampullary part of the rectum is dilated, the sigmoid colon is distended and enlarged. The descending transverse colon - the haustrae are preserved, the cavity is dilated, the splenic angle is passable. Transverse colon - haustrae are preserved, the cavity is dilated, the hepatic angle is passable..
 | Figure 1. Videocolonoscopy of patient N.J. |
 | Figure 2. Irrigogram of patient N.J. in different projections |
 | Figure 3. Postoperative material of patient N.J. |
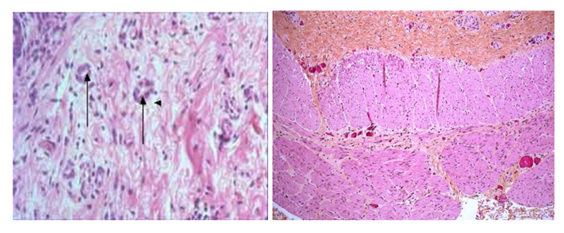 | Figure 4. Microscopy of the obtained material |
 | Figure 5. Patient N.J. in the postoperative period (at the time of discharge) |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML