-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(8): 1166-1167
doi:10.5923/j.ajmms.20231308.28
Received: Aug. 11, 2023; Accepted: Aug. 26, 2023; Published: Aug. 28, 2023

Functional State of the Kidneys in Patients with Arterial Hypertension with Chronic Heart Failure Functional Class II–III in the Post-Covid Period
Giyosova N. O.
Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Giyosova N. O., Bukhara State Medical Institute, Bukhara, Uzbekistan.
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Obviously, the kidneys are not only one of the main links in the pathological chain in the development of chronic heart failure (CHF), but also a target organ. Due to prolonged and high hyperactivation, primarily of the tissue renin-angiotensin-aldosterone system (RAAS), there is a change in the neurohumoral activity of the kidneys, leading to a violation of the functional state, which, in turn, not only supports, but also contributes to further hyperactivation of all components of the RAAS and progression of heart failure. That is, the functional state of the kidneys largely determines the severity and progression of CHF. Evaluation of the dynamics of the functional state of the kidneys can determine the effectiveness of the treatment and the prognosis of a patient with CHF.
Keywords: Chronic heart failure, Renin-angiotensin-aldosterone system, Aldosterone, COVID-19, Microalbuminuria, GFR
Cite this paper: Giyosova N. O., Functional State of the Kidneys in Patients with Arterial Hypertension with Chronic Heart Failure Functional Class II–III in the Post-Covid Period, American Journal of Medicine and Medical Sciences, Vol. 13 No. 8, 2023, pp. 1166-1167. doi: 10.5923/j.ajmms.20231308.28.
1. Introduction
- Aldosterone (AS) is an important regulator of sodium, potassium and water balance in the body [1,5]. Note that in healthy people, it determines the reabsorption of about 10% of the total reabsorbed sodium. However, under conditions of prolonged hyperactivation of the renin-angiotensin-aldosterone system (RAAS), observed in arterial hypertension (AH), chronic heart failure (CHF), chronic kidney disease at the stage of a persistent decrease in glomerular filtration rate (GFR), nephrotic syndrome, the value of aldosterone in retention of sodium and water increases many times [2,4].As a result, aldosterone causes sodium accumulation in the body and contributes to an increase in circulating blood volume (CBV), which leads to an increase in blood pressure (BP) and an increase in potassium excretion from the body. All of the above is of great importance in the pathogenesis of the development and progression of hypertension and CHF.Over the past decades, enough evidence has been accumulated about the wider role of aldosterone in the human body than just the regulation of ion homeostasis [3]. It is known that a long-term increase in the concentration of aldosterone in the blood itself, regardless of the effect on the level of blood pressure, leads to the development of complications of vascular diseases, heart and kidney diseases, as well as metabolic disorders. The results of several experimental studies performed in cell culture and animals, as well as studies in humans, have clarified the mechanisms by which aldosterone and mineralocorticoid receptors (MCR) are involved in the development of inflammation, remodeling and fibrosis in target organs.Purpose of the study. Evaluation of changes in the functional state of the kidneys by determining the level of aldosterone in the blood in patients with arterial hypertension and chronic heart failure of II and III functional class who underwent COVID-19.
2. Materials and Methods
- In order to carry out the research, 120 patients aged 30-60 years were selected. All of the patients had hypertension, comorbidity with chronic heart failure II and III functional class, and it was confirmed that they had COVID-19 (more than12 weeks ago).To assess the functional state of the kidneys, the biochemical parameters of blood were monitored, the level of urea, creatinine, potassium and sodium in the blood serum, the GFR was determined, the level of MAU was determined in urine tests, proteinuria. RAAS activity was assessed by the level of aldosterone in the blood serum.
3. Research results
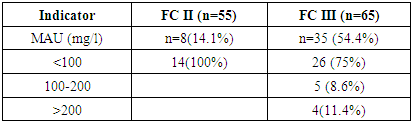
- MAU is a marker of the preclinical stage of morphological and functional kidney lesions [6,7,8]. The MAU study included 120 AH patients with CHF FC II-III (NYHA) who had undergone COVID-19. Among them, 69 men and 51 women, the age of patients ranged from 30 to 60 years, averaging 41.2+4.8 years. The duration of AH ranged from 5 to 10 years, on average 6.3±2.3 years. The duration of CHF ranged from 2.2 to 11.3 years, on average 6.6+1.1 years.MAU in patients with CHF was determined: in the FC II group in 14.1% of patients, in the FC III group in 54.4% of patients. The severity of MAU was assessed by categories: MAU - less than 100 mg/l; 100-200 mg/l; and more than 200 mg/l (Table 1). In patients with CHF FC II, in 100% of cases, MAU was determined less than 100 mg/l. In patients with FC III, MAU values less than 100 mg/l were decisive (75% of patients).
|
4. Conclusions
- 1. Kidney function in hypertensive patients with covid-19 changes already in the early stages of CHF. With an increase in the FC of CHF, the functional ability of the kidneys decreases, which is manifested in an increase in the occurrence and severity of MAU, an increase in the level of creatinine and urea in the blood serum, and a decrease in GFR.2. As CHF progresses, the level of aldosterone in the blood serum increases. Between the level of aldosterone in the blood serum and indicators of the functional state of the kidneys (the level of creatinine in the blood serum, MAU) in patients with hypertension with CHF FC II-III revealed a direct correlation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML