Kh. А. Аkilov1, 2, F. Sh. Primov1, 2, B. N. Tilovov1, 2
1Center for the Development of Professional Qualifications of Medical Workers, Uzbekistan
2Republican Research Centre of Emergency Medicine, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The purpose of the study. Improving the diagnosis and surgical treatment of Meckel's diverticulum (MD) in children with the improvement of therapeutic and diagnostic measures. Material and methods. The present study is based on the results of examination and treatment of 98 children using laparoscopy and 76 patients after laparotomy access surgery admitted to the Department of Pediatric Surgery of the Republican Research Centre of Emergency Medicine, who underwent surgical interventions for Meckel's diverticulum and its complications for the period from 2006 to 2021. Conclusion. The analysis of the summary results showed that the percentage of positive results of surgical treatment of Meckel's diverticulum in children had a higher value after laparoscopic operations, amounting to 94.9% (93 out of 98) versus 85.5% (65 out of 76) with open interventions.
Keywords:
Meckel's diverticulum, Laparoscopy, Endosurgery, Ectopic tissues, Laparoscopic diverticulectomy
Cite this paper: Kh. А. Аkilov, F. Sh. Primov, B. N. Tilovov, Improving the Tactics of Laparoscopic Interventions for Meckel's Diverticulum in Children, American Journal of Medicine and Medical Sciences, Vol. 13 No. 8, 2023, pp. 1161-1165. doi: 10.5923/j.ajmms.20231308.27.
1. Introduction
The urgent task of emergency pediatric abdominal surgery remains to improve the algorithms of diagnostic and therapeutic measures for Meckel's diverticulum, which is a difficult-to-diagnose and frequent congenital anomaly of the gastrointestinal tract [1,2].Along with the widespread opinion that MD is characterized by an asymptomatic course throughout life and it is usually accidentally detected during autopsy, a number of generalizing works present data on a fairly high frequency – 19-25% of clinical manifestations and complications of MD in children [2,3].In the clinical picture of MD, a triad of symptoms are distinguished: abdominal pain, gastrointestinal bleeding and intestinal obstruction. The prevalence and severity of each of them depend on anatomical features, the presence of ectopic tissues in the diverticulum wall with different morphofunctional characteristics, and the age of the patient [4,5].MD is the cause of more than 50% of cases of small intestinal bleeding in children under the age of 2 years. The possibilities of preoperative diagnosis of MD are minimal and do not exceed 12-25% [2,6]. At the same time, a set of special research methods (ultrasonography of abdominal organs, radionuclide method, etc.) acquires a certain importance, the diagnostic capabilities of which are different.The purpose of the study. Improving the diagnosis and surgical treatment of Meckel's diverticulum in children with the improvement of therapeutic and diagnostic measures.
2. Material and Methods
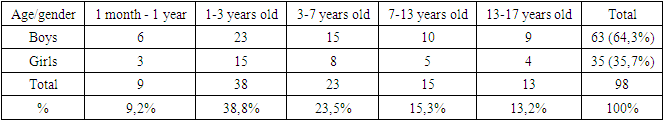
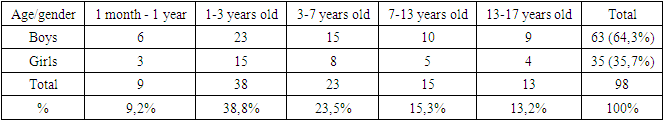
The present study is based on the results of examination and treatment of 98 children using laparoscopy and 76 patients after laparotomy access surgery who were admitted to the Department of Pediatric Surgery of the Clinic of the Republican Research Centre of Emergency Medicine, who underwent surgical interventions for Meckel's diverticulum and its complications for the period from 2006 to 2021.Archival materials and medical histories of children were studied by retrospective and prospective analysis. The age of the children ranged from 1 month to 17 years (Table 1). At the same time, boys made up the vast majority of 63 (64.3%).Table 1. Distribution of patients by gender and age
 |
| |
|
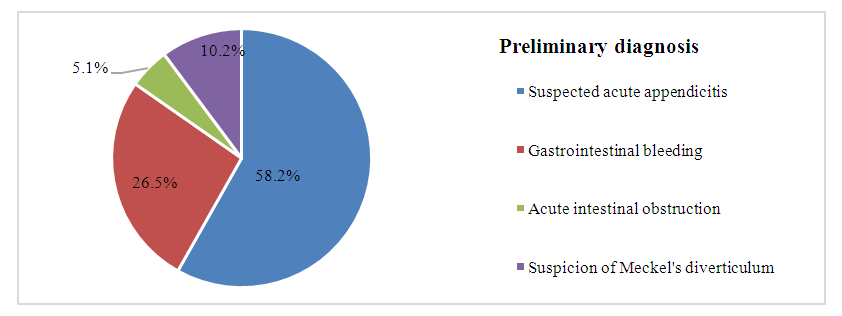
Also, in the age aspect, a relatively large part were children of early childhood (1-3 years) – 38 (38.8%), the next in purity were preschool children (3-7 years) -23 (23.5%), school-age children (7-13 years) they made up 15.3% (15 out of 98), and infants (1 month – 1 year) were the least represented in our study – 9 (9.2%).Patients were referred to us with the following preliminary diagnoses (Fig. 1): in the majority of 57 (58.2%) cases, acute appendicitis was suspected; gastrointestinal bleeding was suspected in 26 (26.5% of 98) cases; Meckel's diverticulum was differentiated in only 10 (10.2%) and less than 5 (5.1%) had a preliminary diagnosis of acute intestinal obstruction.It can be noted that in the vast majority of cases, the diagnosis of MD was not confirmed or even there was no suspicion of its possible presence during the initial examination of the patient.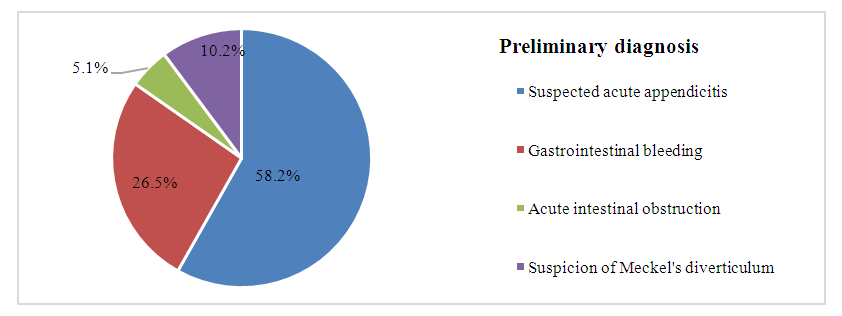 | Figure 1. Distribution of patients according to the directional diagnosis |
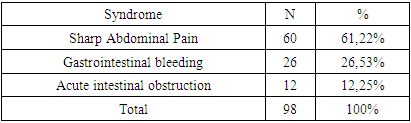
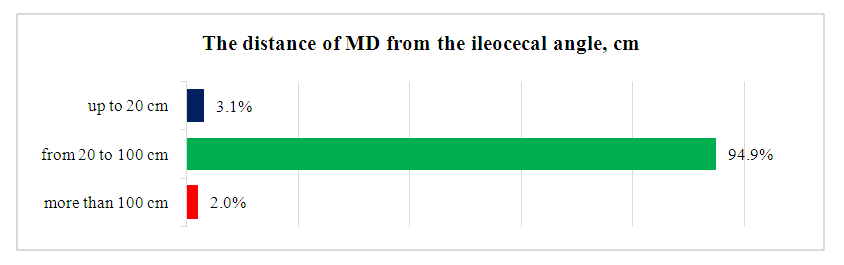
The following clinical situations (Table 2) there were indications for laparoscopic surgery for MD: the presence of symptoms of acute abdomen (n=60), gastrointestinal bleeding (n=26) and acute intestinal obstruction (n=12).Table 2. Symptoms of Meckel's diverticulum
 |
| |
|
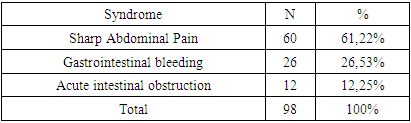
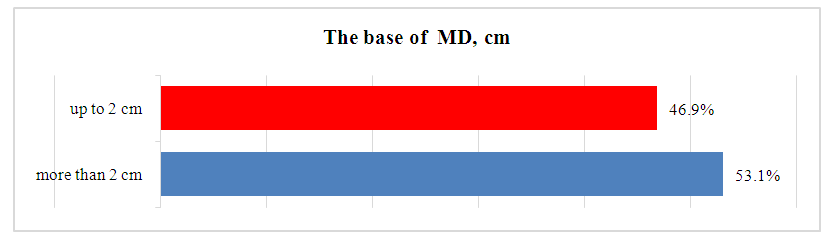
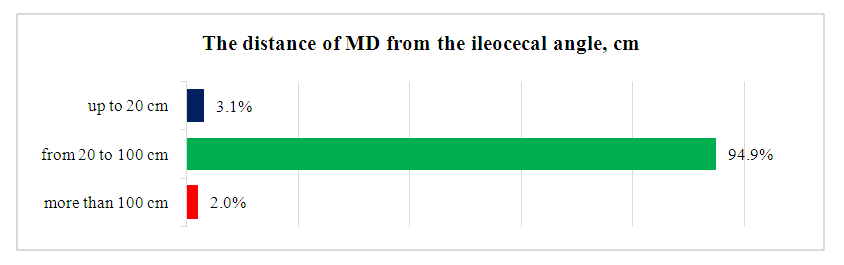
With the introduction of minimally invasive abdominal surgery in children and the accumulation of experience, indications and contraindications to endoscopic methods of diagnosis and treatment changed towards the expansion of indications. To date, the absolute contraindications to laparoscopy in children are: the extremely serious condition of the child, cardiovascular and respiratory insufficiency, pronounced coagulopathy, conditions opposing the safe aseptic administration of trocars.As relative contraindications, the following can be distinguished:- prediction of the total adhesive process in the abdominal cavity of a child according to anamnesis, intraoperative situation during previous interventions, and the results of instrumental diagnostics;- pronounced swelling of the intestinal loops, which counteracts laparoscopic manipulation due to the inability to achieve the required volume of the abdominal cavity.It is necessary to pay attention to some technical features of performing laparoscopic operations with Meckel's diverticulum. When performing laparoscopic revision in search of MD, it is necessary to examine the entire small intestine (diverticula are found at a distance of about 2 m from the ileocecal angle), mobilization of the entire diverticulum, in particular, its base, is mandatory, especially in the presence of intestinal bleeding.Preoperative preparation depended on the patient's condition, which determined the tactics of the examination. Also, depending on the nature of the pathology, the choice was between emergency and planned surgery.During laparoscopy, the anatomical features were clarified intraoperatively and the localization options of the Meckel diverticulum were determined.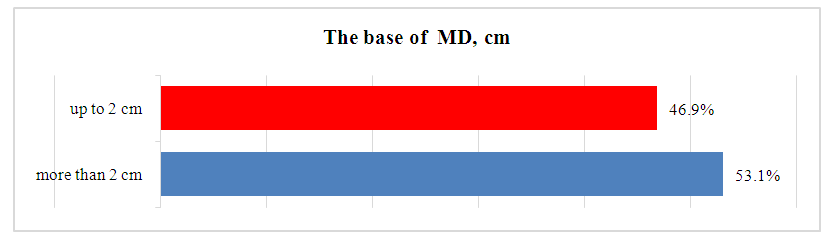 | Figure 2. Variants of the sizes of the base of Meckel diverticulum |
 | Figure 3. Variants of the location of Meckel diverticulum from the ileocecal angle |
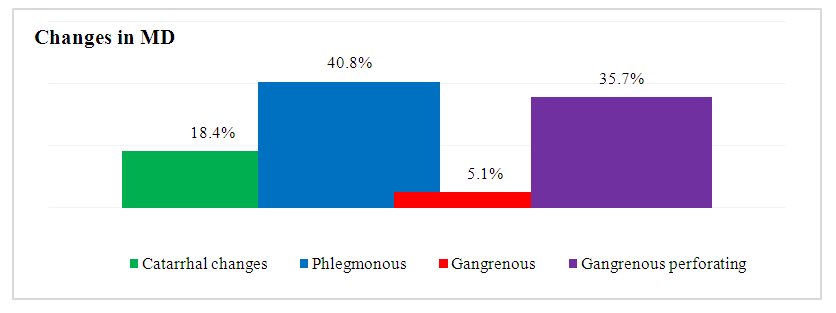
The peculiarity of the anatomical location of the diverticulum is the ratio from the ileocecal angle, which was at a distance of 20 to 100 cm from the diverticulum itself in the vast majority of patients – 93 (94.9%). In addition, according to the localization of the MD, it can be located along the mesenteric edge 51 (52.1%), on the lateral surface 41 (41.8%) and mesenteric edge 6 (6.1%).During the laparoscopic procedure, visual assessment revealed catarrhal 40 (40.8%), phlegmonous 18 (18.4%), gangrenous 35 (35.7%), gangrenous-perforative 5 (5.1%) changes in the diverticulum (Fig. 4).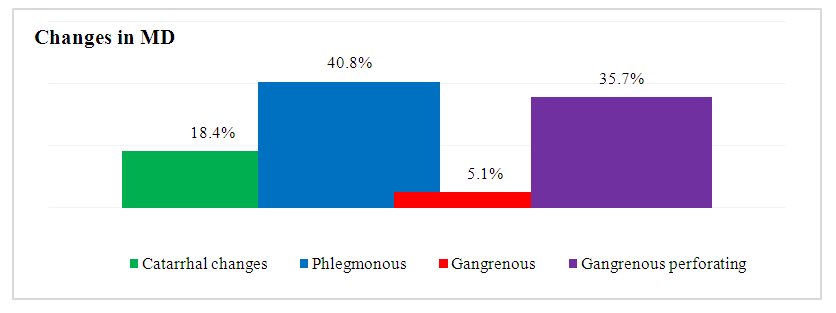 | Figure 4. Variants of pathological changes in Meckel diverticulum |
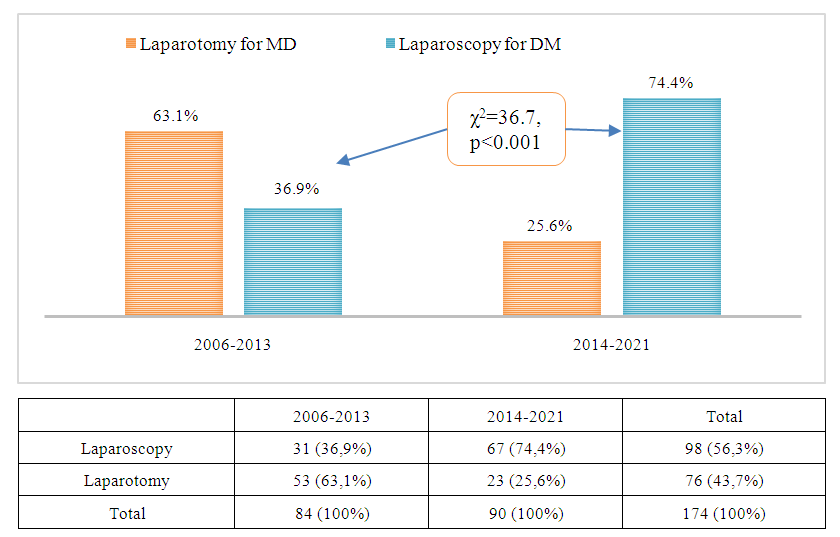
The frequency of laparoscopies and the reduction in the proportion of unjustified open operations with MD in children varied with a statistically significant difference in different periods of research and the introduction of minimally invasive surgery in pediatric practice (Fig. 5). So, if in the period from 2006 to 2013 the proportion of laparoscopies was only 36.9% (31 out of 84), then by 2014-2021, this indicator was increased to 67 (74.4%).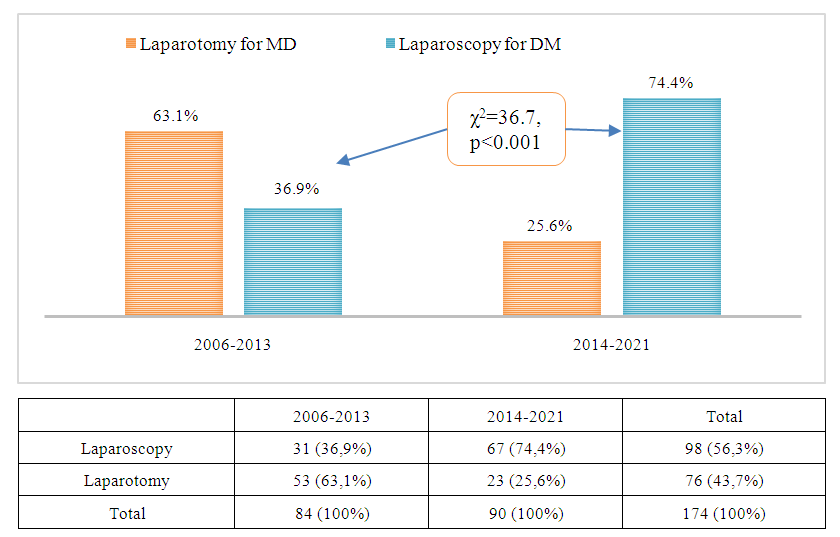 | Figure 5. The proportion of laparoscopies with MD in different periods of the study |
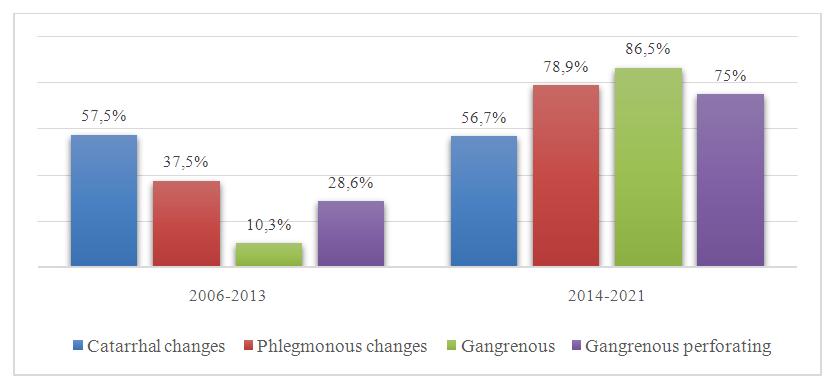
Laparoscopic diverticulectomy with Reader nodular sutures was performed in 32 (32.7%), i.e. in one third of patients. This intervention was supplemented by appendectomy with concomitant inflammation of the appendix in 11.2% of cases.The level of development of minimally invasive surgery for MD in children is determined by the indicator of the use of laparoscopic technique in complex cases (Fig. 6).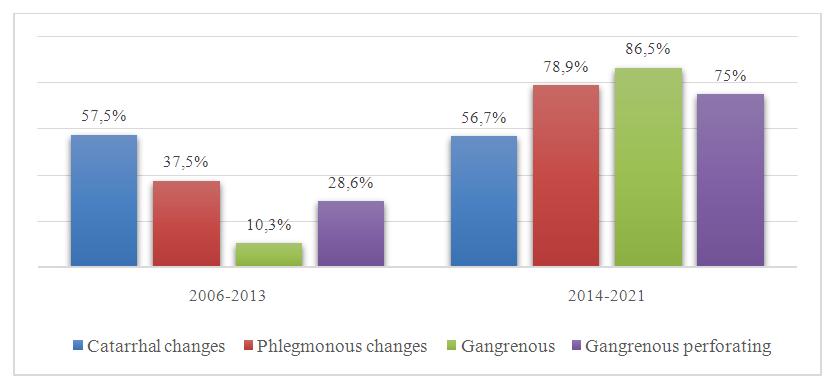 | Figure 6. Indicator of the use of laparoscopic technique in various forms of MD |
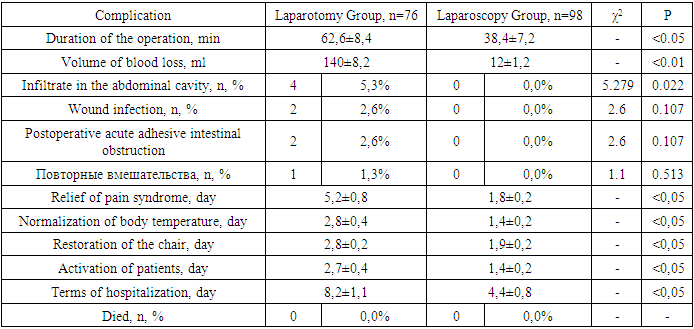
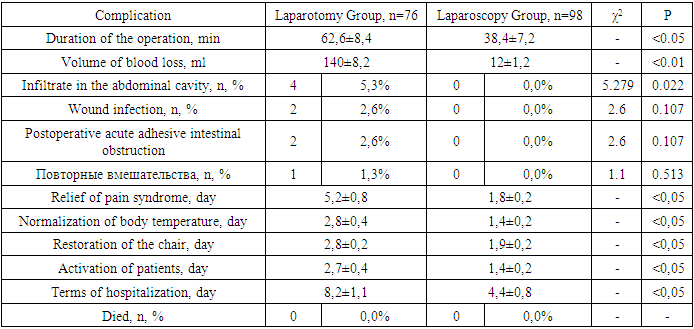
So, if in the first period of the introduction of laparoscopy in pediatric surgery of the Republican Research Centre of Emergency Medicine, operations, in most cases – 57.5%, were performed with the catarrhal form of MD, then as can be seen from Fig. 6, the frequency of laparoscopy in Meckel's gangrenous diverticulum increased from 10.3% to 86.5% (χ2=34.8, p<0.001), with phlegmonous form – from 37.5% to 78.9% (χ2=4.23, p=0.037), gangrenous-perforated form – from 28.6% to 75% (χ2=2.3, p=0.13).There were no intraoperative complications in patients of both the laparoscopy group and the laparotomy group with MD. Laparoscopy duration was significantly shorter compared to open surgery via laparotomy – 38.4±7.2 (from 45 to 60 minutes) versus 62.6±8.4 minutes (from 57 to 74 minutes). The average volumes of intraoperative blood loss were 140±8.2 and 12±1.2 ml in the laparotomy and laparoscopy groups, respectively.The children, for the most part, tolerated surgical interventions for MD well. At the same time, the early postoperative period in traditional open operations was characterized by the development of complications in 8 (10.6%) cases. The formation of an infiltrate in the abdominal cavity was detected in 4 (5.3%) patients, which required additional conservative treatment measures and longer hospitalization. Wound infection and suppuration of the postoperative wound were noted in 2 (2.6%) patients, which required a repeated course of antibiotic therapy, supplemented with physiotherapy and local therapy for a week. In the postoperative period, 2 (2.6%) patients had acute adhesive intestinal obstruction after laparotomy, of which in 1 case this complication was stopped by conservative measures, and in another case it was necessary to perform repeated surgical intervention – to separate the adhesions laparoscopically. Thus, repeated interventions in the laparotomy group were needed in 1 case, which was not noted in the laparoscopy group.Table 3. Comparative characteristics of intra- and postoperative period
 |
| |
|
However, it is also necessary to note the fact of a more pronounced pain syndrome after laparotomy, while after laparoscopy, the pain was easily relieved by non-narcotic drugs. The average duration of persistent pain was 1.8±0.2 days during laparoscopy and 5.2±0.8 days after laparotomy (p<0.05).In the laparoscopy group, children had earlier normalization of body temperature, both with complicated and uncomplicated course of MD.After traditional operations with MD, a longer recovery of the stool was recorded (2,4 days) than after laparoscopic interventions (1,2 days) due to a significant decrease in the severity of intestinal paresis.Patients were active 1.4±0.2 days after laparoscopy and 2.7±0.4 days after laparotomy.No deaths were observed in any group.
3. Conclusions
1. Optimization of the tactical aspects of minimally invasive surgery for MD in children allowed to reduce the frequency of postoperative complications from 8 (10.6%) to 0.0% with a statistically significant difference (χ2=8.546, p=0.004), including the proportion of specific complications was reduced from 7.9% to 0.0%, general complications – from 2.6% up to 0.0%.2. The analysis of the summary results showed that the proportion of positive results of surgical treatment of MD in children had a higher value after laparoscopic operations, amounting to 93 (94.9%) versus 65 (85.5%) with open interventions.
References
| [1] | Вечеркин В.А., Высоцкая В.П., Гисак С.Н., Кораблёв В.А., Коряшкин П.В., Кузнецова В.О., Баранов Д.А. Дифференцированный подход к лапароскопическому лечению перитонитов у детей. Молодежный инновационный вестник. 2016; 5(1): 5-17. |
| [2] | Дронов А. Ф., Поддубный И. В., Котлобовский В. И. Эндоскопическая хирургия у детей. М.: ГЭОТАР-МЕД. 2002: 440. |
| [3] | Di Saverio S, Vennix S, Birindelli A, Weber D, Lombardi R, Mandrioli M, Tarasconi A, Bemelman WA. Pushing the envelope: laparoscopy and primary anastomosis are technically feasible in stable patients with Hinchey IV perforated acute diverticulitis and gross faeculent peritonitis. Surg Endosc. 2016 Dec; 30(12): 5656-64. doi: 10.1007/s00464-016-4869-y. |
| [4] | Кущ Н.Л., Тимченко А.Д. Лапароскопия у детей // Вестник хирургии им. И.И. Грекова. 1969; 102(5): 92–94. |
| [5] | Courtney M. Townsend, Jr., R. Daniel Beauchamp, Mark Evers, Kenneth L. Mattox. Sabiston Textbook of Surgery, 19th Edition. 2012. |
| [6] | Zitsman JL. Pediatric minimal-access surgery: update 2006. Pediatrics. 2006; 118(1): 304–308. doi: 10.1542/peds.2005-2736. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML