-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(8): 1156-1160
doi:10.5923/j.ajmms.20231308.26
Received: Aug. 6, 2023; Accepted: Aug. 22, 2023; Published: Aug. 28, 2023

Comparative Evaluation of the Effectiveness of Endoscopic Interventions in Mallory-Weiss Syndrome
Yakubov F. R.1, Erniyazov E. A.1, Sapaev D. S.1, Mardonov J. N.2
1Urgench Branch of Tashkent Medical Academy, Uzbekistan
2State Unitary Enterprise Republican Specialized Scientific – Practical Medical Center of Surgery Named after Academician V. Vakhidov, Uzbekistan
Correspondence to: Sapaev D. S., Urgench Branch of Tashkent Medical Academy, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

For clinical surgery, the method of endoscopic stopping of bleeding and treatment of ruptures of the mucous membrane of the cardioesophageal zone of the stomach, characterized by a prolonged hemostatic effect, increased local anti-inflammatory and regenerative processes, has been improved. It was found that the proposed method of endoscopic subserous injection of the gel composite substance Хemoben into the area of rupture of the mucous membrane in the cardioesophageal transition in Mallory-Weiss syndrome provided an increase in the primary hemostatic effect from 83.6% to 98.2% (p=0.006), in turn, the overall effectiveness, taking into account the achieved primary and secondary (with early relapse) hemostasis the increase was 100%, which made it possible to eliminate the need for forced surgical treatment.
Keywords: Mallory-Weiss syndrome, Forrest classifications, Active bleeding, Endoscopic hemostasis
Cite this paper: Yakubov F. R., Erniyazov E. A., Sapaev D. S., Mardonov J. N., Comparative Evaluation of the Effectiveness of Endoscopic Interventions in Mallory-Weiss Syndrome, American Journal of Medicine and Medical Sciences, Vol. 13 No. 8, 2023, pp. 1156-1160. doi: 10.5923/j.ajmms.20231308.26.
Article Outline
1. Introduction
- Mallory-Weiss syndrome is defined as a linear rupture of the mucous membrane in the area of the esophageal-gastric junction, which is usually preceded by vomiting or another reason for a rapid increase in intra-abdominal pressure. This is a relatively rare cause of acute bleeding from the upper gastrointestinal tract, which accounts for about 10% of bleeding during endoscopic examination [1,2]. Most often, this pathology passes in a mild form, but there are also contradictory data on mortality. A European observational study showed that the 30-day mortality rates for Mallory-Weiss syndrome are 5.3%, in the UK – 3.8%, in the USA the mortality rate is 1.3%, and in Japan – 9.7%. Mortality in Mallory-Weiss syndrome in patients with bleeding from a high-risk group is similar to mortality from bleeding from a peptic ulcer. There is uncertainty as to which patients with this pathology need endoscopic treatment. In turn, the optimal method of endoscopic treatment, which is divided into adrenaline injections, mechanical clipping, thermocoagulation options and ligation, remains a controversial issue [3,4]. All techniques can be effective, but there is insufficient evidence to indicate a preferred method. All this, combined with the continuing relevance in terms of possible recurrence of bleeding in Mallory-Weiss syndrome, indicates the ambiguity and lack of standardized scientific approaches to therapeutic and diagnostic tactics in various clinical situations.Questions concerning the optimal endoscopic treatment of Mallory-Weiss syndrome still remain unresolved. There is uncertainty about which patients with this pathology need endoscopic therapy: the European Society of Gastrointestinal Endoscopy (ESGE) recommends endoscopic therapy only for "active bleeding", and the American Society of Gastrointestinal Endoscopy (ASGE) - for "ongoing or severe bleeding" [5]. Recently published data showed that according to the Forrest classification, the need for endoscopic treatment occurs with type Ia, Ib and IIa bleeding, whereas patients with IIb, IIc and III were successfully treated without endoscopic therapy [6]. In turn, another controversial issue remains the choice of the optimal method of endoscopic treatment, which is divided into injections of adrenaline, mechanical clipping, options for thermocoagulation and ligation. All techniques can be effective, but there is insufficient evidence to indicate a preferred method [7,8,9]. The European Society for Gastrointestinal Endoscopy (ESGE) indicates that there is currently insufficient evidence to recommend a specific hemostatic method.The analysis of the literature shows that, despite significant progress in the treatment of Mallory-Weiss syndrome, there are still controversial issues of choosing the method of endoscopic intervention, therefore, the search for new and modernization of already known methods of stopping bleeding by combined exposure to the defect area of various methods of endoscopic hemostasis with the parallel use of general hemostatic measures continues, antisecretory, blood-substituting action. Also important are the issues of combining endoscopic hemostasis with increased reparative activity on the part of mucosal tear in the cardio-esophageal transition zone.
2. Material and Methods of Research
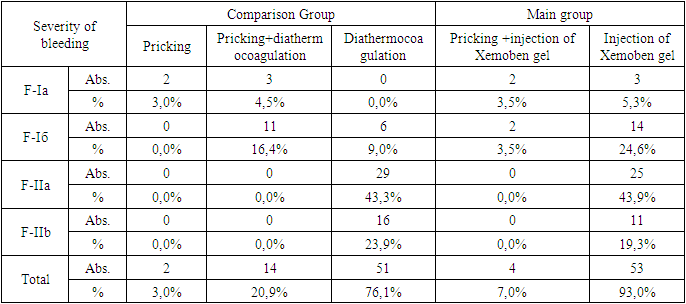
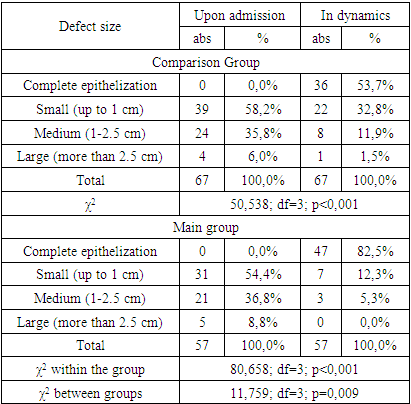
- The clinical study included 124 patients with Mallory-Weiss syndrome complicated by bleeding, and the bleeding activity corresponded to ongoing bleeding – according to the classification of Forrest (1974) I a and b degrees, or stopped - Forrest II a and b degrees. All patients underwent endoscopic manipulations to stop bleeding on the basis of the Khorezm and Nukus branches of the Republican Scientific Center for Emergency Medical Care for the period from 2016 to April 2023. The patients were divided into two groups. The main group included 57 patients who underwent a new method of endoscopic hemostasis in 2022-2023. The comparison group consisted of 67 patients who underwent traditional endoscopic interventions (2016-2021).Male patients significantly prevailed in both groups – 54 (80.6%) and 46 (80.7%), respectively, with 34 (50.7% and 29 (5.9%) patients aged 20-44 years. There were 13 (19.4%) women in the comparison group, 11 (19.3%) in the main group. The average age was 43.5±14.3 years in the comparison group, 46.4±14.7 years in the main group.Upon admission, all patients underwent endoscopic examination. Active bleeding corresponding to grade Ia according to the Forrest classification (1974) was detected in 5 patients in the comparison group (7.5%) and 5 (8.8%) in the main group, F-Ib was diagnosed in 17 (25.4%) and 16 (28.1%) cases, respectively, suspended bleeding of grade F-IIa It was in 29 (43.3%) and 25 (43.9%), F-IIb degree in 16 (23.9%) and 11 (19.3%) patients. In general, there was active bleeding in 22 (32.8%) patients in the comparison group and 21 (36.8%) in the main group, and suspended bleeding in 45 (67.2%) and 36 (63.2%) patients.Anamnesis collection showed that alcohol abuse was the cause of the development of Mallory-Weiss syndrome in 54 (80.6%) patients in the comparison group and 44 (77.2%) in the main group, the alimentary factor with the development of vomiting was noted in 6 (9%) and 8 (14%) patients, respectively, a strong cough caused a rupture the mucosa of the gastroesophageal junction in 4 (6%) and 3 (5.3%) patients, the provoking factor was not detected in 3 (4.5%) and 2 (3.5%) patients.During endoscopic diagnosis, mucosal rupture in 11 (16.4%) cases in the comparison group and 8 (14%) in the main group was in n/3 of the esophagus, in the transition zone to the stomach, a rupture with bleeding was detected in 44 (65.7%) and 36 (63.2%) patients, respectively, in the cardiac part of the stomach in 12 (17.9%) and 13 (22.8%) patients. The extent of the gap up to 1 cm (small gap) was verified in 39 (58.2%) cases in the comparison group and 31 (54.4%) in the main group, the average gap (from 1 to 2.5 cm) was in 24 (35.8%) and 21 (36.8%) patients, large gaps (more than 2.5 cm) were determined in 4 (6%) and 5 (8.8%) cases.The depth of the linear rupture did not go beyond the mucosa in 23 (34.3%) cases in the comparison group and 18 (31.6%) in the main group, it continued into the submucosal layer in 39 (58.2%) and 34 (59.6%) patients, and a deeper tear spreading to the muscle layer was noted in 5 (7.5%) and 5 (8.8%) patients. A single rupture of the mucosa was in 50 (74.6%) cases in the comparison group and 41 (71.9%) in the main group, multiple defects were in 17 (25.4%) and 16 (28.1%) patients. According to the Algover classification (1967), the severity of blood loss corresponded to a mild degree in 34 (50.7%) cases in the comparison group and 27 (47.4%) in the main group, the average degree was noted in 24 (35.8%) and 22 (38.6%) patients, the severe degree was in 9 (13.4%) and 8 (14%) of patients.All patients had active or suspended bleeding. Only pricking in the comparison group was performed in 2 (3%) patients, pricking and diathermocoagulation in 14 (20.9%) and only diathermocoagulation in 51 (76.1%) patients. In the main group, Xemoben gel injection was performed in all 57 patients, of which 4 (7%) were pre-injected with adrenaline (Table 1).
|
3. Results and Discussion
- Taking into account the severity of bleeding, the results were analyzed in subgroups with ongoing (Forrest-I a-b) and stopped bleeding (Forrest-II a-b).The proposed method of endoscopic subserose injection of the Xemoben gel composite substrate into the mucosal rupture zone in the area of cardioesophageal transition in Mallory-Weiss syndrome provided an increase in the primary hemostatic effect with continued bleeding (F-I a-b) from 72.7% (in 16 of 22 patients in the comparison group) to 95.2% (in 20 of 21 patients in the main group; χ2=3,995; df=1; p=0.046), in the subgroup of stopped bleeding (F-II a-b) from 88.9% (in 40 of 45 patients in the comparison group) to 100% (in all 36 patients in the main group; χ2=4,263; df=1; p=0.039) and in general in groups from 83.6% (in 56 of 67 patients in the comparison group) to 98.2% (in 56 of 57 patients in the main group; χ2=7,576; df=1; p=0.006) (Figure 1).
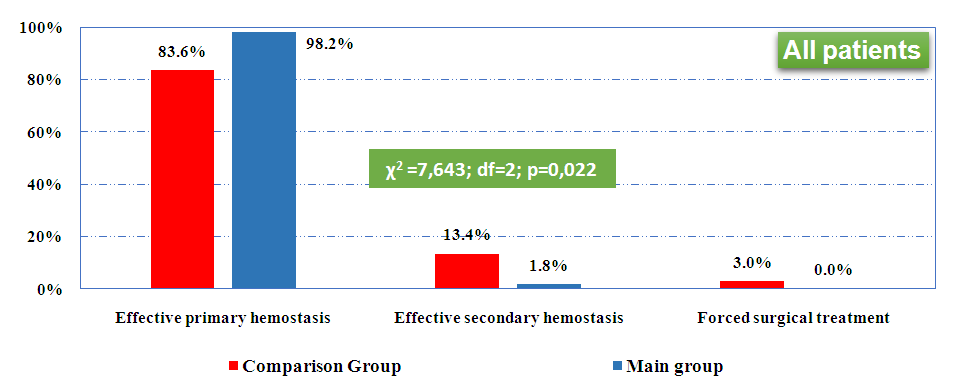 | Figure 1. The overall effectiveness of endoscopic interventions in Mallory-Weiss syndrome |
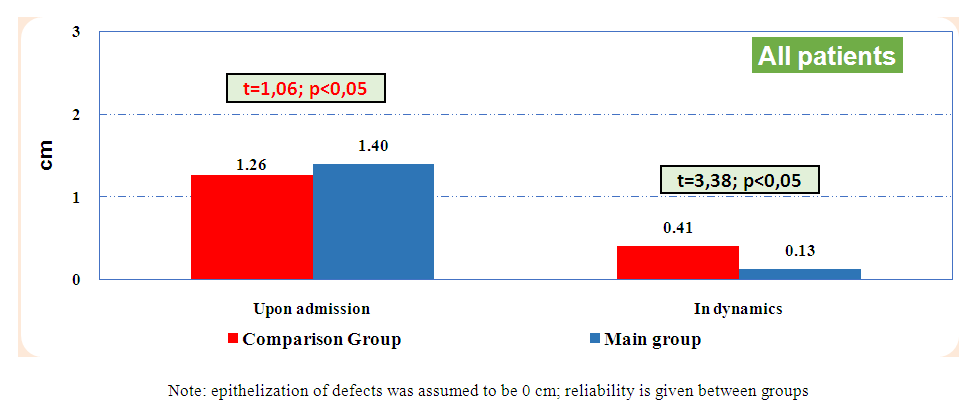 | Figure 2. Summary dynamics of rupture repair (cm; M±σ) |
|
4. Conclusions
- 1. The proposed method of endoscopic subserose injection of the Xemoben gel composite substance into the mucosal rupture zone in the area of cardioesophageal transition in Mallory-Weiss syndrome provided an increase in the primary hemostatic effect from 83.6% to 98.2% (p=0.006), in turn, the overall effectiveness taking into account the achieved primary (83.6% and 98.2%, respectively) and secondary (with early relapse; 13.4% and 1.8%), hemostasis increased from 97.0% to 100%, which made it possible to eliminate the need for forced surgical treatment from 3.0% to 0 (p=0.022).2. Complex conservative therapy after endoscopic interventions in patients with Mallory-Weiss syndrome made it possible in both groups to significantly reduce the size of linear tears of the mucous membrane of the cardioesophageal junction, while the use of Xemoben gel injection provided an increase in the reparative effect, which proves the dynamics of defect size indicators on 4-6 days after manipulation, which changed in the comparison group from 1.26±0.67 to 0.41±0.58 cm and in the main group from 1.40±0.78 to 0.13±0.33 cm (t=3.38; p<0.05), while complete epithelialization in these terms was achieved in 53.7% and 82.5% of patients, respectively (p=0.009).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML