S. N. Isirgapova1, M. A. Sabirov1, N. N. Sultonov1, O. V. Skosireva1, Sh. N. Eshonov2
1Tashkent State Dental Institute, st. Makhtumkuli 103, Tashkent, Uzbekistan
2Republican Specialized Scientific Practical Medical Center of Nephrology and Kidney Transplantation, st. Yangi Shahar 9, Tashkent, Uzbekistan
Correspondence to: N. N. Sultonov, Tashkent State Dental Institute, st. Makhtumkuli 103, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Today, according to statistics, there is a clear trend towards an increase in the average life expectancy of women. According to G.M. Dyukova (2013), the average life expectancy in developed countries for women was about 10 years ago 75–80 years, and in developing countries, it was ten years less. But, in this situation, the age of menopause is still stable and averages 49-50 years. Based on this, almost one third of a woman's life is spent during the menopause, and therefore the issues of the quality of life (QOL) of a woman during this period are very relevant, especially in the category of people who continue active work.
Keywords:
Quality of life, Chronic kidney disease, Menopause, Hormone terapy
Cite this paper: S. N. Isirgapova, M. A. Sabirov, N. N. Sultonov, O. V. Skosireva, Sh. N. Eshonov, Assessment of the Quality of Life of Women with Hormonal Status Disorders under Program Hemodialysis, American Journal of Medicine and Medical Sciences, Vol. 13 No. 8, 2023, pp. 1123-1128. doi: 10.5923/j.ajmms.20231308.19.
1. Introduction
Today, according to statistics, there is a clear trend towards an increase in the average life expectancy of women. According to G.M. Dyukova (2013), the average life expectancy in developed countries for women was about 10 years ago 75–80 years, and in developing countries, it was ten years less. But, in this situation, the age of menopause is still stable and averages 49-50 years. Based on this, almost one third of a woman's life is spent during the menopause, and therefore the issues of the quality of life (QOL) of a woman during this period are very relevant, especially in the category of people who continue active work.
2. Relevance of the Problem
As you know, in the climacteric period (CP) there is a morphofunctional restructuring of many organs and systems of the female body, which is manifested by a wide range of disorders that conditionally subdivided into neurovegetative, metabolic-endocrine and psycho-emotional [2,6,8]. Where in, a decrease in quality of life (QOL) during this period is primarily associated with estrogen deficiency, against which develop about metabolic-endocrine disorders, manifested osteoporosis, hypothyroidism, decreased levels of vitamin D, calcium and magnesium. To neutralize the negative manifestations and improve the prognosis, according to modern recommendations, gynecologists prescribe hormone replacement therapy [7,9,10]. However, taking into account the hormonophobia of society, according to the literature data, 63% of women believe in herbal medicine and widely use it for various diseases and conditions [14]. But, to date, a detailed study from the standpoint of evidence-based medicine, various herbal remedies with estrogenic activity are just beginning. At the same time, despite the use in women with climacteric syndrome (CS) sex and thyroid hormones, vitamin D and calcium, in some cases does not allow to achieve the desired results in improving QOL in this category of patients [1,3,5]. Due to this in recent years, with a detailed study of the diversity of manifestations of menopause, scientists have come to the conclusion that some of them are associated with magnesium deficiency, the decrease in the level of which goes hand in hand with a decrease in hormones produced by the ovaries. At the same time, the study of the role of hypomagnesemia and the effectiveness of its correction in women in menopause devoted to only a few works [4,11,13].The physiological role of magnesium is very diverse, it is involved in many biochemical processes, is an activator of several hundred enzymes and a DNA stabilizer in the processes of mitosis and meyosis, participates in transmembrane transport of ions, in the process of thermoregulation of the body. The important role of this microelement in the functioning of the cardiovascular system (CVS) and the nervous system has been proven [15]. Research by H.E. Meema et al. At the end of the last century, it was shown that magnesium deficiency in the blood in the terminal stage of chronic kidney disease (CKD), in the absence of replenishment of its level, contributes to the development of arterial calcification of the arteries and an increase in cardiovascular mortality in patients with stage V CKD, and the normalization of magnesium can slow down this process. The development of hypomagnesemia, in addition to other dyselectrolyte disorders in women in the age group of 45-55 years, can partly explain the development of symptoms characteristic of CS. Standardized basic therapy in the interdialysis period of such patients, unfortunately, does not lead to a significant relief of the manifestations of CS with an increase in their QOL, which dictates the need to search for new approaches to correct macroelectrolytes and hormonal imbalance [12]. Taking into account the main physiological effects of magnesium and the leading clinical manifestations of its deficiency, the correction of magnesium levels should be one of the first tasks in menopausal women. This task is of particular relevance in situations in women receiving program hemodialysis (PGD), since such procedures in themselves lead to hypomagnesemia with aggravation of metabolic imbalance against the background of constant not only somatic, but also mental stress, which exacerbates the decline in their QOL.In this regard, the aim of our study was to study the effect of phytoestrogen treatment in combination with a magnesium preparation on the level of trace elements (magnesium, calcium, potassium and phosphorus), sex hormones and QOL in women with CS receiving PGD.
3. Patients and Methods
The study included 58 women aged 45-55 years, on average - 48.3±4.8 years (main group - MG) with clinically diagnosed CKD stage V, with impaired water-excretory function of the kidneys, who are on PGD at the Republican Specialized Scientific Research Institute - practical center of nephrology and kidney transplantation. Determination of the stage of CKD was carried out according to international recommendations. The leading nosology in the development of CKD was chronic glomerulonephritis (in 42 patients), chronic pyelonephritis (in 16 patients). The control group (CG) included 20 women of comparable age without any diseases of the cardiovascular system, respiratory system (RS), endocrine or renal diseases, who are in the climacteric period (CP). Patients with stage V CKD received program hemodialysis 3 times a week for an average of 4 hours. Hemodialysis sessions were carried out on Dialog devices manufactured by B Braun (Germany) using Low Flux Series Hallon Fiber Dialyzers from Shadono Weigao Blood Purification Products Co.Ltd. (PRC). During the procedure, a certified standard dialysis solution was used, vascular access was in the form of a native arteriovenous fistula. The duration of the hemodialysis session averaged 4 hours, the duration of stay on PGD ranged from 3 to 8 years and was in the vast majority of cases 5-6 years. Taking into account that the women of the MG were in the SF, for an objective assessment of their QOL, the level of which can be associated not only with the underlying disease and hemodialysis, but also with severe manifestations in the SF, they were examined by a gynecologist, who established the presence of a CS in them. To assess the severity of QOL. According to the questionnaire, according to the sum of the points scored, 4 degrees of QOL impairment are divided, in conjunction with the CS: 1 - no menopausal syndrome (0-11 points), 2 - mild menopausal syndrome (12-34 points), 3 - moderate menopausal syndrome (35 -58 points), 4-severe climacteric syndrome (59 points and above). The study of the composition of macroelements (magnesium, calcium, potassium) in the blood serum was carried out by atomic absorption spectrophotometry using the Analyst-400 apparatus (Perk in Elmer Inc.). The level of hormones in the blood serum was determined using the Mindray MR-96A apparatus (OSIYO MEDIKA) by enzyme immunoassay (ELISA). The control points of the study were the first point - before the start of the next hemodialysis procedure, the second - on the 30th day of observation, the third point - on the 90th day of observation. Medical preparation for the hemodialysis procedure and treatment in the interdialysis period were carried out in accordance with the National Standard. According to this standard, the traditional therapy of OH patients in the interdialysis period consisted of iron preparations and erythropoietin, calcium, B vitamins, antihypertensives and diuretics. At the same time, patients in both groups had not previously received magnesium-containing drugs and hormone replacement therapy (HRT). To justify the inclusion in the complex therapy of patients with CS undergoing PGD, preparation of magnesium and phytoestrogen in women, the OG were divided into 2 subgroups. Patients OG I (38 women) received in addition to standard therapy magnesium preparation "Biolectra Magnesium Fortissimum" (as part of magnesium oxide lung 342 mg and magnesium carbonate lung 670 mg, which corresponds to magnesium ions 365 mg (15 mmol)in the form of effervescent tablets) 1 time in the morning after meals. OGII patients (20 women) received in addition to this preparation magnesium, HRT in the form of a phytoestrogen called "Monopous essel" 1 capsule 2 times a day with meals, which contains essential phospholipids and soy isoflavone 40% with an estrogen-like effect. The course of treatment was 90 days. Side effects from additionally prescribed drugs were not observed.
4. Results and Discussion
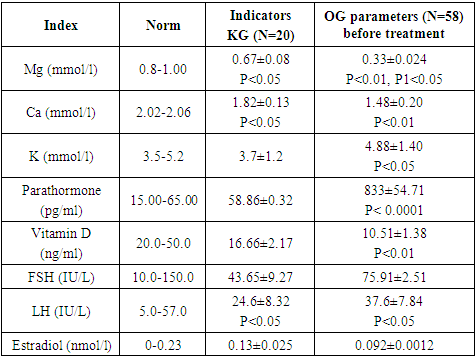
According to the results of the study of the applied modified Kuppermans questionnaire, in all women, the MG level of QOL ranged from 38 to 51 points and averaged 41.73±5.3 points, which corresponds to moderate CS. At the same time, according to the National recommendations, the appointment of HRT is required, however, patients before our study were not prescribed any therapy for CS. The study of the macroelement composition of the blood, the level of vitamin D, parathyroid and sex hormones in the examined OH patients demonstrated the following (Table 1). The level of magnesium in the blood in the exhaust gas was sharply reduced and averaged 0.33±0.024 mmol/l (p<0.001), calcium and vitamin D3 were also significantly reduced to 1.5±0.04 mmol/l ( p<0.003) and up to 9.1±0.33 mIU/l (p<0.001), respectively. In contrast, the concentrations of potassium and parathyroid hormone in the serum of these patients were high, especially the concentration of the latter: the potassium index was 4.5 ± 0.14 mmol/l (p<0.01) and parathyroid hormone - 833, 46±54.71pg/ml (p<0.0004), respectively. Hormonal imbalance in relation to sex hormones was manifested by a significantly reduced level of estradiol to 0.092±0.13 IU/l, (p<0.0001) while maintaining the concentration of FSH and LH within their reference values.Table 1. The content of macronutrients, vitamin D, parathyroid and sex hormones in women with CS who are on PGD before treatment
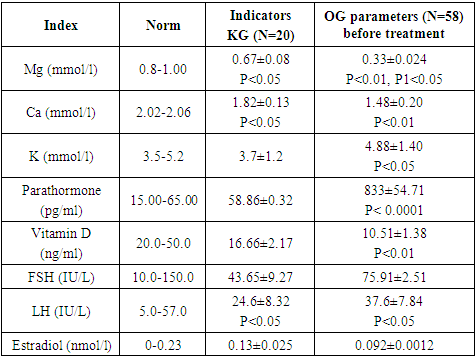 |
| |
|
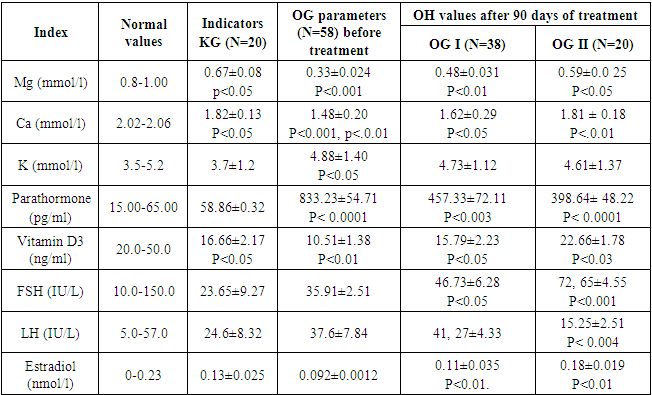
To assess the effect of renal replacement therapy sessions on the level of macroelements in the blood serum, we additionally once conducted a study of some laboratory parameters of patients with OH after the next session of PGD. We found that after the next hemodialysis, the concentration of calcium, and especially magnesium, in the blood had a clear tendency to decrease, but without a significant difference between the content of these macronutrients before and after HD. Thus, dialysis patients revealed a pronounced deficiency of magnesium, calcium and a significant deficiency of vitamin D3, as well as a sharp decrease in the level of estradiol. At the same time, the concentration of parathyroid hormone was very high with moderate hyperkalemia. Similar parameters studied in the group of women from the CG who are in the CP, 0.67±0.08 mmol/l (P<0.05). On day 30observations, the study of the severity of the manifestations of the CS according to the questionnaire showed a slight decrease in its subjective manifestations with an increase in the quality of the quality of life of patients in both groups, but without significant differences in comparison with the baseline scores and among themselves in the groups. The dynamics of laboratory parameters at the same time in both groups was characterized by the absence of a tendency to a decrease in the level of magnesium and an increase in the level of parathyroid hormone. At the same time, other laboratory tests did not reveal any differences in comparison with their baseline values before the start of treatment. When studying the dynamics of the studied indicators at the end point (day 90), the following was found (see table). Examination of the questionnaire data and laboratory tests at the end point of the study (day 90 of observation) revealed other patterns. Thus, the assessment of the severity of clinical manifestations of CS indicated a significant improvement in QOL in both groups with a clear advantage in patients with OH II (p<0.06).Table 2. The content of macroelements, vitamin D, parathyroid and sex hormones in women with CS undergoing PGD in the dynamics of differentiated treatment with magnesium and phytoestrogen
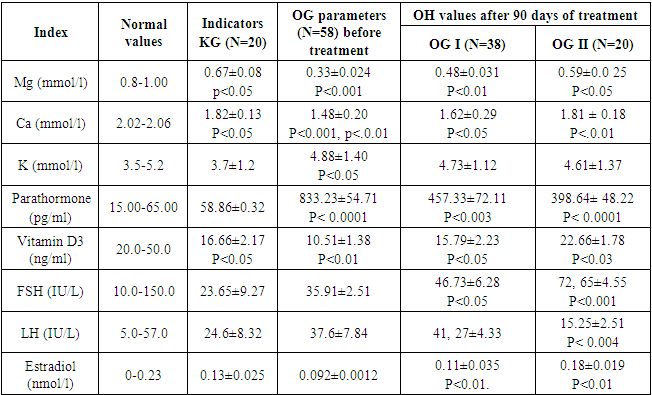 |
| |
|
The average QOL scores of women in OG I were 33.85±4.11 pointsand for women OG II 28.72±6.33 points. When comparing the dynamics of laboratory parameters at the same time in both groups revealed the following. The state of macronutrient metabolism was characterized by a significant increase in the concentration of magnesium in both groups with higher values in OG II (up to 0.48±0.031 mmol/l and up to 0.59±0.0 25 mmol/l, respectively, with significant intergroup differences – p < 0.05), which, however, did not reach the normal values of this macronutrient. The calcium concentration significantly increased in both groups compared with the initial values and amounted to 1.62 ± 0.29 mmol/l in MG I, and up to 1,81 ± 0,18 mmol/l in OG II, with a difference in the groups p < 0, 05. The level of vitamin D, also increased in all patients, while in patients of MG I it was 15.79±2.23 ng/ml on the 90th day of observation, in MG II it was 22.66±1.78 ng/ml with a significant intergroup difference (p<0.05). The values of parathyroid hormone indicated its sharp decrease in both groups: to 457.33±72.11 (in OG I) and to 398.64±48.22 (OG II) with a significant difference in the groups p < 0.01. At the same time, there was a slight decrease in the concentration of potassium without a significant intergroup difference, but with a clear tendency towards his depression in OG II. With regard to the dynamics of sex hormones, a significant significant increase in the level of FSH compared with the initial data was found in patients of MG II, which amounted to 72.65±4.55 IU/l (p<0.001), in contrast to patients of MG I, who had the same the indicator was 46.73±6.28 IU/l (p<0.05), with an intergroup difference p<0.01. The concentration of other sex hormones in the course of treatment fluctuated within normal values, but with a significant decrease in LH values to 15.25±2.51 IU/l compared with baseline data (p<0.003) and compared with those values of OG I (41,27±4.33 IU/l, p<0.001). The level of estradiol significantly increased to the same extent in both groups to 0.11±0.035 nmol/l to 0.18±0.019 nmol/l. Besides, we have established a clear relationship between the content of magnesium and calcium in the blood in patients with CKD stage V. We have found that the replenishment of magnesium in patients receiving PGD leads to a more significant increase in calcium concentration in them. At the same time, before the administration of the magnesium preparation to our patients, while they received significant doses of vitamin D - 50,000 IU (1.250 mg) per week, however, the state of hypocalcemia persisted. In addition, a clear inverse relationship was found between the content of parathyroid hormone and magnesium in the blood serum of the studied patients. Thus, a 3-month course of the use of the drug magic and phytoestrogen largely led to the elimination of imbalances in macronutrients and hormonal status with the relief of most manifestations of CS and an increase in the quality of life of patients receiving PGD. That the replenishment of magnesium in patients receiving PGD, leads them to a more significant increase in the concentration of calcium. At the same time, before the administration of the magnesium preparation to our patients, while they received significant doses of vitamin D3 - 50,000 IU (1.250 mg) per week, however, the state of hypocalcemia persisted. In addition, a clear inverse relationship was found between the content of parathyroid hormone and magnesium in the blood serum of the studied patients. Thus, a 3-month course of the use of the drug magic and phytoestrogen largely led to the elimination of imbalances in macronutrients and hormonal status with the relief of most manifestations of CS and an increase in the quality of life of patients receiving PGD. That the replenishment of magnesium in patients receiving PGD, leads them to a more significant increase in the concentration of calcium. At the same time, before the administration of the magnesium preparation to our patients, while they received significant doses of vitamin D3 - 50,000 IU (1.250 mg) per week, however, the state of hypocalcemia persisted. In addition, a clear inverse relationship was found between the content of parathyroid hormone and magnesium in the blood serum of the studied patients. Thus, a 3-month course of the use of the drug magic and phytoestrogen largely led to the elimination of imbalances in macronutrients and hormonal status with the relief of most manifestations of CS and an increase in the quality of life of patients receiving PGD. Before the appointment of the magnesium preparation to our patients, while they received significant doses of vitamin D3 - 50,000 IU (1.250 mg) per week, however, the state of hypocalcemia persisted. In addition, a clear inverse relationship was found between the content of parathyroid hormone and magnesium in the blood serum of the studied patients. Thus, a 3-month course of the use of the drug magic and phytoestrogen largely led to the elimination of imbalances in macronutrients and hormonal status with the relief of most manifestations of CS and an increase in the quality of life of patients receiving PGD. Before the appointment of the magnesium preparation to our patients, while they received significant doses of vitamin D3 - 50,000 IU (1.250 mg) per week, however, the state of hypocalcemia persisted. In addition, a clear inverse relationship was found between the content of parathyroid hormone and magnesium in the blood serum of the studied patients. Thus, a 3-month course of the use of the drug magic and phytoestrogen largely led to the elimination of imbalances in macronutrients and hormonal status with the relief of most manifestations of CS and an increase in the quality of life of patients receiving PGD.For patients with CS receiving PGD, maintaining and improving QOL is the most important task. From these positions, it seems relevant to maintain a stable level in the blood serum of such a macronutrient as magnesium. Analysis of the results of our studies on the assessment of the content of the main macronutrients in the blood serum. This category of women showed that in all patients on the background of hemodialysis there is a pronounced deficiency of magnesium, calcium, vitamin D and estradiol with a simultaneous increase in potassium and, especially, parathyroid hormone. In this case, repeated sessions of hemodialysis lead to aggravation of hypomagnesemia. Besides, us V regularities were revealed in the form of a multidirectional relationship between the content of magnesium, parathyroid hormone and calcium in the blood serum. This leads to an important conclusion about the need for replacement therapy with magnesium preparations in patients undergoing PGD treatment. The dynamics of the state of QOL and laboratory parameters at the intermediate control point on the 30th day of observation in both groups did not show significant changes in the studied parameters. At the end point of observation, the change in QOL was analyzed in comparison with laboratory parameters. expressiveness clinical manifestations of CS decreased significantly and corresponded, according to the questionnaire, to its mild degree in both groups with a clear advantage in patients of MG II. When comparing the dynamics of laboratory parameters at the same time, it was demonstrated by an increase in the concentration of magnesium in both groups with higher values in MG II, however, without achieving normal values of this macronutrient, similar patterns were found in the dynamics of the level of calcium and vitamin D3. A pronounced depression in the concentration of parathormone, especially in OG II with a parallel mild decrease in the concentration of potassium without a significant difference in the groups. As a result of treatment at the final control point, a pronounced increase in FSH levels was recorded in patients in MG II compared with baseline data, in contrast to patients in MG I. At the same time, the LH level was characterized by its significant depression, especially in comparison with patients in OG I. Estradiol levels significantly increased equally in both groups with no significant difference between groups. In addition, we have established a clear direct relationship between the content of magnesium and calcium in the blood of patients with stage V CKD receiving PGD, which was confirmed by a number of DM researchers. Spiegel, 2011, N.A. Mikhailova, 2013). Prior to prescribing a magnesium preparation to our patients, while they received significant doses of vitamin D3 - 50,000 IU (1, 250 mg) per week, however, did not eliminate the state of hypocalcemia. However, the use of a magnesium-containing drug in the complex therapy of such patients led to a significant increase in the level of calcium. In addition, a clear inverse relationship was found between the content of parathyroid hormone and magnesium in the blood serum of the studied patients. A more significant positive dynamics of CS manifestations in women receiving PGD, in comparison with the results of laboratory tests, allows us to conclude that in order to improve the quality of life and correct the macroelement composition of the blood and hormonal imbalance in this category of patients, it is necessary to include magnesium preparations in combination with HRT in complex therapy. as a phytoestrogen. The use of a magnesium-containing drug in the complex therapy of such patients led to a significant increase in the level of calcium. In addition, a clear inverse relationship was found between the content of parathyroid hormone and magnesium in the blood serum of the studied patients. A more significant positive dynamics of CS manifestations in women receiving PGD, in comparison with the results of laboratory tests, allows us to conclude that in order to improve the quality of life and correct the macroelement composition of the blood and hormonal imbalance in this category of patients, it is necessary to include magnesium preparations in combination with HRT in complex therapy as a phytoestrogen. The use of a magnesium-containing drug in the complex therapy of such patients led to a significant increase in the level of calcium. In addition, a clear inverse relationship was found between the content of parathyroid hormone and magnesium in the blood serum of the studied patients. A more significant positive dynamics of CS manifestations in women receiving PGD, in comparison with the results of laboratory tests, allows us to conclude that in order to improve the quality of life and correct the macroelement composition of the blood and hormonal imbalance in this category of patients, it is necessary to include magnesium preparations in combination with HRT in complex therapy as a phytoestrogen.
5. Conclusions
1. In patients with CS receiving PGD. Revealed a deficiency in the blood serum of the main essential macroelements (magnesium and calcium), as well as vitamin D3, with a simultaneous increase in the content of potassium and, especially, parathyroid hormone.2. The next session of hemodialysis leads to a further decrease in the concentration of magnesium and calcium in this category of patients.3. Inflammation of magnesium concentration more effectively leads to the elimination of hypocalcaemia, vitamin D3 deficiency and hyperparathyroidemia.4. The inclusion of magnesium and phytoestrogen in interdialysis therapy in patients with CS who are on PGD, largely eliminates the manifestations of CS and increases QOL.
References
| [1] | Амбрамова Е.Э., Королева И.Е., Тов Н.Л. и др. Факторы риска летальных исходов у больных на гемодиализе // Journal of Siberian Medical Sciences 2015, №6, С. 15-26. https://cyberleninka.ru/article/n/faktory-riska-letalnyh-ishodov-u-bolnyh-na-gemodialize?ysclid =ljptuekiqo489814987. |
| [2] | Мирзаева Барно Миркамол кизи. Ренальная остеодистрофия у больныхтерминальной стадии почечной недостаточности, получающих гемодиализ, и пути её коррекции. Диссертация. 2020г. http://repository.tma.uz/xmlui/handle/1/2214. |
| [3] | Мунавваров Б.А., Сурункали буйрак касаллиги билан огриган беморларда гипоазотемик дори-воситаларини куллаш билан даволашни мукобиллаштириш. Автореферат. 2020й. http://repository.tma.uz/xmlui/handle/1/821. |
| [4] | Профессор Зайдиева Я. З. Альтернативная терапия менопаузальных расстройств у женщин в климактерии. Акушерство/Гинекология. РМЖ, 2017 № 12. С. 873-878. https://www.rmj.ru/articles/ginekologiya/Alyternativnaya_terapiya_menopauzalynyh_rasstroystv_u _ghenschin_v_klimakterii/?ysclid=ljptxaoimm6490185. |
| [5] | Сметник В.П. Менопаузальная гормонотерапия и сохранение здоровьяженщин зрелого возраста. Клинические рекомендации: протоколы // Климактерий. 2015. 49 cтр. http://zdrav.spb.ru/media/filebrowser.pdf. |
| [6] | Султонов Н.Н. Сурункали буйрак касаллиги билан огриган беморларда гемодинамик бузилишларни бахолашда антиагрегант терапияни мукобиллаштириш. 2020й. http://repository.tma.uz/xmlui/handle/1/870. |
| [7] | Шарапов О.Н., Сердечно-сосудистые заболевания у больных получающих гемодиализ. 2021г. https://doi.org/10.26739.2181-0974-2021-3-10. |
| [8] | Хроническая болезнь почек (ХБП) клинические рекомендации. 2021г. 3-й пересмотр. https://diseases.medelement.com/disease/2021/16916?ysclid=ljptaejvhe988756101. |
| [9] | Baber R.J., Panay N., Fenton A. et al. IMS Recommendations on women’s midlife health and menopause hormone therapy (MHT) // Climacteric. 2016. Vol. 19(2). P. 109–150. https://pubmed.ncbi.nlm.nih.gov/26872610/. |
| [10] | Bobokulov M. B., Sabirov M. A., Munavvarov B.A. Evaluation of the Morphofunctional State of the Transplant in the Period after Kidney Transplantation NeuroQuantology - All Rights Reserved. Volume 20, No 8 (2022) P.9877-9884. DOI: 10.48047/nq.2022.20.8.NQ221009. https://univerpubl.com/index.php/synergy. |
| [11] | Daminova K.M., Sabirov M.A., Babajanova N.R., Daminova H.M., Munavvarov B.A. Some Risk Factors For The Development And Progression Of Chronic Kidney Disease In A Primary Line Of Health Care. Chin J Ind Hyg Occup Dis, 2021, Vol. 39, No.7. https://zhldwszyb.cn/2021/08/19/2021-vol-39-no-7/. |
| [12] | Guidelines for hormone treatment of women in the menopausal transition and beyond / F. Naftolin, H.P. Schneider, I.D. Sturdee et al. // Position state-ment by the Executive Committee of the International Menopause Society. – 2015. – 127 (3–4). – P. 94–96. https://doi.org/10.1016/j.maturitas.2004.03.001. |
| [13] | Hruska K.A., Mathew S., Lund R. et al. Hyperphosphatemia of chronic kidney disease // Kidney International. 2018. №74. Р. 148–157. https://www.kidney-international.org/article/S0085-2538(15)53280-8/fulltext. |
| [14] | Sultonov, N. N., Sabirov, M. O., Tashpulatova, M. H., & Maksudova, L. I. (2020). Evaluating the effectiveness of antiplatelet therapy of the patients with kidney disease. European Journal of Molecular and Clinical Medicine, 7(8), 1500-1505. https://scholar.google.com/citations?view_op=view_citation&hl=ru&user=7UUm1gkAAAAJ&citation _for_view=7UUm1gkAAAAJ:5nxA0vEk-isC. |
| [15] | Моисеев В.С., Мухин Н.А., Смирнов А.В. и соавт. Сердечно - сосудистый риск и хроническая болезнь почек: стратегии кардио-нефропротекции // Российский кардиологический журнал. – 2014. - № 8 (112). – С. 7-37. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML