-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(8): 1114-1117
doi:10.5923/j.ajmms.20231308.17
Received: Aug. 3, 2023; Accepted: Aug. 20, 2023; Published: Aug. 23, 2023

An Improved Method of Non-Tension Hernioplasty for Inguinal Hernias
Khujamov Olim Bakhritdinovich, Davlatov Salim Sulaymonovich
Bukhara State Medical Institute, Republic of Uzbekistan, Bukhara
Correspondence to: Khujamov Olim Bakhritdinovich, Bukhara State Medical Institute, Republic of Uzbekistan, Bukhara.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The study included the results of surgical treatment of 85 patients who underwent hernioplasty for inguinal hernia. To study the effectiveness of the proposed method of inguinal hernia hernioplasty, the results of treatment in two groups were compared. For the first group, for control comparison, in 24 patients, hernioplasty was performed using the Lichtenstein method, in 61 patients, the developed method of inguinal hernia alloplasty was used. The presented technique for reconstructing the inguinal canal, aimed at reducing trauma and reducing the time of intervention, can be used in wide practice.
Keywords: Inguinal hernia, Non-tension, Hernioalloplasty
Cite this paper: Khujamov Olim Bakhritdinovich, Davlatov Salim Sulaymonovich, An Improved Method of Non-Tension Hernioplasty for Inguinal Hernias, American Journal of Medicine and Medical Sciences, Vol. 13 No. 8, 2023, pp. 1114-1117. doi: 10.5923/j.ajmms.20231308.17.
Article Outline
1. Introduction
- The “non-tensioning” technique of inguinal hernioalloplasty according to Lichtenstein has shown a number of obvious advantages over traditional types of inguinal hernioplasty. The operation takes a little time, is easy to perform and is quite acceptable at cost [3,8,11].However, often the inguinal ligament is so loose that it can hardly be a reliable place to fix the prosthesis. There is a need for its additional fixation. Using the Cooper ligament for this, as many authors recommend, only partially solves the problem, and Kozlov's methods with the formation of an artificial inguinal ligament and Fletching using a "three-layer mesh" are technically difficult [3,5,9].In addition, it is not always possible to observe the principle of "no tension" with the Lichtenstein method. The weakness of the inguinal ligament encountered makes it necessary to resort to grabbing into a continuous seam and part of the aponeurosis of the external oblique abdominal muscle for a more durable fixation of the prosthesis. In addition, the capture of the Cooper ligament into the seam shifts the inguinal ligament downwards. As a result, stitching the flaps of the aponeurosis of the external oblique abdominal muscle is impossible without tension. Even a slight swelling of the tissues that occurs in the postoperative period leads to even greater tension of the anterior wall of the inguinal canal. Incomplete restoration of the integrity of the anterior wall of the inguinal canal with the abandonment of a large external inguinal ring leads to straightening of the inguinal canal and violation of its valve function [2,7,10].It should also be noted that exudation resulting from surgical trauma and in response to the prosthesis, as a foreign body, can lead to fluid accumulation in the inguinal canal cavity, edema of the spermatic cord and testicle. The use of various types of drains frees from hematomas and effusion fluid often only subcutaneous tissue, while the effusion remains in the inguinal canal [1,4,6,14].Another important thing is that the posterior wall of the inguinal canal is strengthened only by a weakened transverse fascia and a mesh implant. The mechanical load immediately falls on the graft. There is a need to use dense "heavy" nets, because the use of lightweight and semi-absorbable nets with an increase in intra-abdominal pressure leads to the separation or rupture of the mesh and, as a consequence, the recurrence of hernia. But also transplants made of "heavy" polypropylene are reduced in size by 30% during the year, which also contributes to relapse [5,9,13]. Also, a pre-cut graft with a hole for the spermatic cord is fixed to the tissues with the formation of folds, because it does not take into account the individual characteristics of the inguinal space. In addition, fixation of the upper edge of the graft to the surface of the internal oblique abdominal muscle leads to a number of negative consequences: to the eruption of sutures and migration of the mesh implant due to the low mechanical strength of muscle tissue; to the danger of injury to muscle vessels, and in conditions of early loading - to the formation of intermuscular hematomas, suppuration of the postoperative wound; to the formation of a rough rigid scar on the site of the formed folds [6,10,12].In general, the described changes show that after implantation of a synthetic prosthesis by the Lichtenstein method in the tissues of the inguinal region, processes occur that predispose to the development of a possible recurrence of hernia.The aim of the study is to optimize non-tensioning herniplasty in inguinal hernias by introducing a new method of alloplasty.
2. Materials and Methods of Research
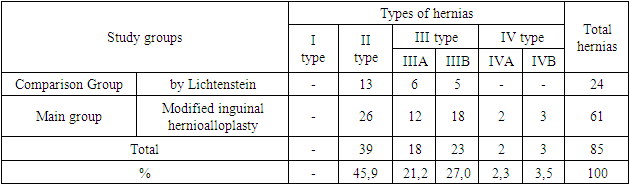
- The study is based on the results of examination and treatment of patients with inguinal hernias who were operated in the surgical department of the multidisciplinary regional hospital of Bukhara in the period from 2018 to 2023. 85 patients with inguinal hernias were selected for a prospective dynamic active study. These were male patients with inguinal hernias of various types. The patients were operated on both as planned and as an emergency, and depending on the choice of treatment tactics, the patients were divided into two groups. The first group, the comparison group, consisted of 24 (28.2%) patients with inguinal hernias who underwent hernioalloplasty using the Lichtenstein method. The second, main group consisted of 61 (71.8%) patients who underwent inguinal hernioalloplasty according to our modified method.According to the types of hernias (classification of L.M. Nyhus), the distribution in the groups is shown in Table 1. The total number of oblique hernias in patients was 62 (72.9%). The number of type III hernias (direct hernias) was 18 (21.2%), recurrent inguinal hernias were found in 5 (5.9%) cases. Based on the statistical analysis carried out by the type of hernias in the studied groups, they can be considered homogeneous (pχ2 > 0,05).
|
3. The Results of the Study
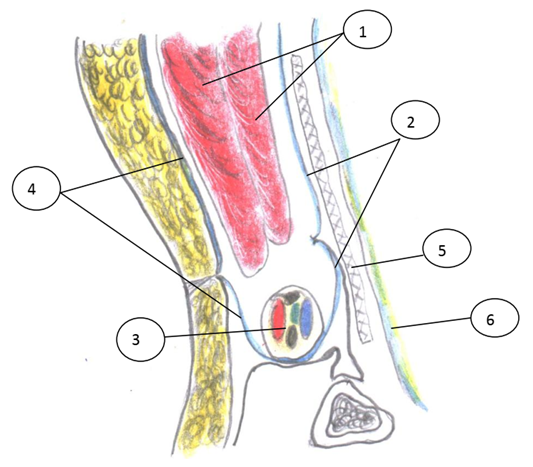
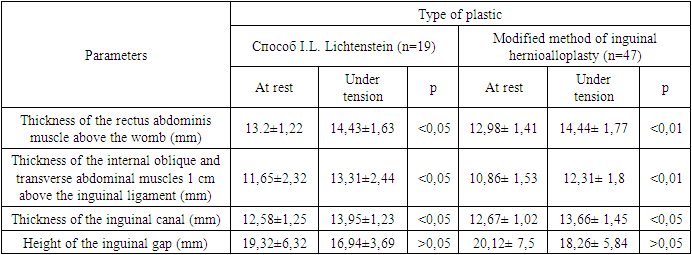
- A reduction in the traumatic nature of surgical access with early activation of operated patients, the possibility of strengthening the posterior wall of the inguinal canal with polypropylene mesh with preperitoneal fixation contributed to a twofold reduction in the duration of postoperative fever, i.e., seroma secretion decreased from 16.7% to 1.6%.After alloplastic, changes in the inguinal canal were studied by ultrasound. In the course of the study, in order to study the constituent tissues of the inguinal canal, the thickness of the rectus abdominis muscle, the internal oblique and transverse abdominal muscles, the height of the inguinal gap at rest and under tension (leg lift by 15°) was measured in patients who underwent alloplasty of a hernial defect 1 month after surgery in 47 (77.0%) and 19 (79.2%) patients of the main group and in the comparison group, respectively (Table 2).After alloplasty (after 1 month), during ultrasonography of the inguinal area, the mesh implant behind the spermatic cord is well traced, regardless of whether the plastic was performed according to the I.L.Lichtenstein technique or preperitoneal alloplasty in the modification we proposed. The transverse fascia is not always possible to visualize.Under stress, regardless of the type of alloplasty, there was a significant (p>0.05) increase in the thickness of the rectus abdominis muscle, the internal oblique and transverse abdominal muscles, and the thickness of the inguinal canal. The height of the inguinal space decreased slightly (p>0.05). This indicates that changes in the inguinal region in patients after alloplasty (according to the I.L. Lichtenstein technique or preperitoneal aloplasty of a hernial defect in the proposed modification) at rest and under load are identical (Table 2).
|
4. Conclusions
- Surgery using the I.L. Lichtenstein method is technically simple and available in execution, however, it gives a recurrence of hernia in 5.3% of patients. Preperitoneal alloplasty of a hernial defect in the modification we propose is a reliable alternative to surgery according to the I.L. Lichtenstein technique in the treatment of patients with inguinal hernia of medium and large sizes, recurrent inguinal hernia, which, if performed correctly, does not give relapses and has a low number of complications characteristic of alloplasty, which do not depend on the type of mesh implant used.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML