-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(8): 1058-1060
doi:10.5923/j.ajmms.20231308.05
Received: Jun. 12, 2023; Accepted: Jul. 23, 2023; Published: Aug. 12, 2023

Polymorphism of IL-17A G-197A Locus and Predisposition to Bronchial Asthma
Akhmedov F. S.1, Ziyadullaev Sh. K.1, Khudaiberdiev Sh. Sh.2, Rizaev J. A.1, Kamalov Z. S.3, Ruzybakieva M. R.3
1Samarkand State Medical University, Samarkand, Uzbekistan
2AKFA University, Tashkent, Uzbekistan
3Institute of Immunology and Human Genomics of Academy of Sciences of the Republic of Uzbekistan, Tashkent, Uzbekistan
Correspondence to: Akhmedov F. S., Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction: Bronchial asthma is a chronic inflammatory respiratory disease with a multifactorial nature. Genetic factors play a crucial role in the predisposition to bronchial asthma, and studying genetic polymorphisms can help identify risk markers and develop personalized treatment approaches. Materials and Methods. In this study, we investigated the association between the IL17A gene polymorphism (rs2275913 G/A) and predisposition to bronchial asthma in the Uzbek population. The study included 97 patients with bronchial asthma and 111 healthy individuals as a control group. Genotyping of the IL17A gene polymorphic loci was performed using the polymerase chain reaction (PCR) method and allele-specific primers. Results: Analysis of the genotype and allele frequencies of the IL17A gene revealed significant differences between the bronchial asthma group and the control group. The A allele of the IL17A gene was associated with an increased risk of developing bronchial asthma, while the G allele was less frequent in patients with bronchial asthma. The AA genotype of the IL17A gene was also associated with an increased risk of bronchial asthma, while the GG genotype showed a protective effect. Conclusion: Our findings support the role of the IL17A gene in the predisposition to bronchial asthma in the Uzbek population. The A allele and AA genotype of the IL17A gene serve as risk markers indicating the possibility of developing bronchial asthma, while the G allele and GG genotype have a protective value. These results may contribute to the development of more accurate diagnostic methods, prognosis, and personalized approaches to the treatment of bronchial asthma.
Keywords: Bronchial asthma, Genetic polymorphism, IL17A gene, Predisposition, Uzbek population
Cite this paper: Akhmedov F. S., Ziyadullaev Sh. K., Khudaiberdiev Sh. Sh., Rizaev J. A., Kamalov Z. S., Ruzybakieva M. R., Polymorphism of IL-17A G-197A Locus and Predisposition to Bronchial Asthma, American Journal of Medicine and Medical Sciences, Vol. 13 No. 8, 2023, pp. 1058-1060. doi: 10.5923/j.ajmms.20231308.05.
1. Introduction
- Bronchial asthma is a respiratory disease characterized by a variety of symptoms and is marked by chronic inflammation and increased airway hyperresponsiveness. The underlying basis of this disease is an inadequate immune response to various environmental stimuli, particularly in individuals with a genetic predisposition. Symptoms of bronchial asthma include shortness of breath, wheezing, coughing, and chest tightness.According to research data, bronchial asthma affects 1% to 18% of the global population [1]. This presents a significant public health problem that requires attention and the development of effective management and prevention strategies. Genetic factors play a crucial role in the development of this disease, and studies have shown that numerous genetic polymorphisms are associated with susceptibility to or protection against bronchial asthma [2-5].In particular, genes encoding polymorphic proteins, especially those involved in immune regulation, have attracted significant attention from researchers [6]. These genes can vary in their structure and functions, affecting the body's ability to respond to the environment and the development of the inflammatory process.One such gene is IL17A, which encodes a protein of the same name and is located on the short arm of chromosome 6 in humans (6p12.2). Studies have shown that single nucleotide polymorphisms in the IL17A gene are associated with predisposition to various immune-mediated and inflammatory diseases [7]. These polymorphisms can influence the expression of the IL17A gene and the functions of Th17 cells, which play a crucial role in immune responses and inflammatory processes [8-9].However, there have not been enough studies conducted to determine the role of IL17A gene polymorphisms in the predisposition to bronchial asthma in the Uzbek population. Therefore, conducting such studies can be valuable for a deeper understanding of the genetic mechanisms underlying this disease and for the development of individualized approaches to the diagnosis and treatment of patients with bronchial asthma.In conclusion, bronchial asthma is a chronic disease characterized by airway inflammation and hyperresponsiveness. Genetic factors, including gene polymorphisms related to immune reactions, play a significant role in the predisposition to this condition. The IL17A gene is one of the key genes associated with immune and inflammatory processes, and its polymorphisms can influence the development of bronchial asthma. Further research, including studies involving the Uzbek population, will contribute to expanding our knowledge of the genetic basis of bronchial asthma and developing more effective strategies for its diagnosis and treatment.The aim of this study is to investigate the single nucleotide polymorphism (SNP) of the IL17A gene (rs2275913 G/A) in patients with bronchial asthma in the Uzbek population and assess its association with predisposition to this disease.
2. Materials and Methods
- The study was conducted on a group of 97 patients with bronchial asthma. The study participants were selected from patients under observation at the Department of Internal Medicine, Samarkand State Medical University. In addition, a control group of 111 healthy individuals, matched to the patients in terms of age and gender, was included in the study. The control group had no signs or symptoms of allergy.A high-pitched whistling sound produced during breathing due to narrowed airways. Difficulty in breathing or a feeling of breathlessness. A sensation of pressure or constriction in the chest. A persistent cough, especially at night or early in the morning. Increased production of sticky mucus, which may be coughed up or cause throat irritation. Feeling tired or exhausted due to the strain on the respiratory system. Frequent respiratory infections such as colds, bronchitis, or pneumonia.It's important to note that these symptoms can vary in intensity and frequency among individuals with bronchial asthma. It is always recommended to consult a medical professional for accurate diagnosis and appropriate management of the condition.In the study, the single nucleotide polymorphism (SNP) of the IL17A gene (rs2275913 G/A) was investigated. Genomic DNA was obtained using a two-step cell lysis method. The purification of leukocyte lysates was based on the salt-precipitation method developed by S. Miller et al. (1988), with some modifications proposed by the Stanford University laboratory. Genotyping of immune response gene polymorphic loci was performed using the polymerase chain reaction (PCR) method with allele-specific primers 5'-ttcccatttttccttcagaag [A/G] agagattcttctatgacctc - 3' (NPP "Litekh", Moscow), and the reaction products were detected by agarose gel electrophoresis. The identification of amplified products and their distribution by length marker was carried out under ultraviolet light (310 nm) after a 15-minute electrophoresis at 300V with subsequent ethidium bromide staining.The distribution of genotypes in the investigated polymorphic loci was analyzed using logistic regression analysis and tested for Hardy-Weinberg equilibrium using the exact Fisher's test. The analysis took into account the matching of patients and control group participants by gender and age. The statistical significance of differences was set at p<0.05. Data processing was performed using Microsoft Excel, SISA9.17®, as well as statistical software packages SISA, Arlequin 3.5.2., and relevant formulas.
3. Results and Discussion
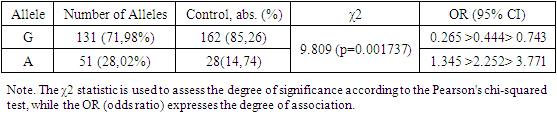
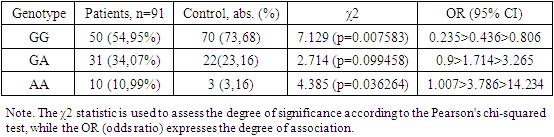
- Analyzing the results (Table 1), it can be concluded that the A allele of the IL17A gene, associated with the development of bronchial asthma (BA), is present in this sample with a frequency of 28.02%, while its frequency in the control group is 14.74%. Statistical analysis showed a significant association between this allele and the development of BA (OR = 2.252; 95% CI: 1.345 >2.252> 3.771; χ2=9.809 (p=0.001737)). Conversely, the G allele of the IL17A gene was observed significantly less frequently in the BA group compared to the control group (71.98% and 85.26%, respectively). Statistical analysis also confirmed the association between the G allele and a protective effect against the development of BA (OR = 0.444; 95% CI: 0.265 >0.444> 0.743; χ2=9.809 (p=0.001737)). Thus, the obtained data indicate that the A allele variant of the IL-17A G-197A gene is a risk marker for the development of bronchial asthma in this sample.
|
|
4. Conclusions
- Our findings underscore the importance of genetic factors in the pathogenesis of bronchial asthma and may contribute to the development of personalized approaches to diagnosis, prevention, and treatment of this disease. However, it should be noted that our study was conducted on the Uzbek population, and further research on larger cohorts and in different ethnic groups is required to confirm and generalize our results.Overall, our study contributes to the understanding of the genetic mechanisms of bronchial asthma and may facilitate the development of more accurate diagnostic methods, prognostication, and individualized approaches to the treatment of this prevalent condition.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML