-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(7): 1016-1019
doi:10.5923/j.ajmms.20231307.36
Received: Jul. 6, 2023; Accepted: Jul. 25, 2023; Published: Jul. 27, 2023

Morphofunctional Characteristics of the Nose Mucosa after Simultaneous Surgery
U. S. Khasanov, A. A. Rakhimov, B. O. Sultanov, J. U. Rustamov, B. D. Jumanyozov
Researcher, Tashkent Medical Academy, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The characteristics of the methods of checking the condition of the nasal mucosa after the combined surgical procedure performed in the nasal cavity are presented. Modern advances in medicine in the last decade allow expanding the scope of simultaneous operative procedures. Simultaneous (joint, at the same time) operations allow to eliminate several pathological conditions in the nose and paranasal sinuses at the same time. A strong curvature of the nasal septum is one of the most common local factors associated with the pathology of nasal cavities. Disruption of nasal breathing leads to changes in mucociliary clearance and creates conditions for inflammation in nasal cavities.
Keywords: Nasal cavity, Functional endoscopic sinus surgery (FESS), Paranasal sinuses
Cite this paper: U. S. Khasanov, A. A. Rakhimov, B. O. Sultanov, J. U. Rustamov, B. D. Jumanyozov, Morphofunctional Characteristics of the Nose Mucosa after Simultaneous Surgery, American Journal of Medicine and Medical Sciences, Vol. 13 No. 7, 2023, pp. 1016-1019. doi: 10.5923/j.ajmms.20231307.36.
1. Introduction
- In modern medicine, diseases of the nose and paranasal sinuses (PS) occupy the main place among the diseases of the upper respiratory organs. Simultaneous operations ("simultaneous" in English - at the same time) are complex operative practices aimed at the simultaneous surgical correction of two or more diseases of different organs in one or more anatomical areas. It is especially important to perform simultaneous operations in cases where there is a pathogenetic connection between two surgical diseases. If the existing joint pathology is not surgically corrected at the same time, the disease may worsen in the postoperative period. It should be noted that simultaneous surgical correction performed by an otorhinolaryngologist is cost-effective compared to separate operations, in which the bed-day is reduced by 2 or more times, the costs of examinations, pre- and post-operative treatment, and anesthetic drugs are reduced. With the implementation of FESS procedures, the number of operative procedures performed in the nasal cavity has increased significantly. Currently, elimination of the pathological process based on the analysis of the data of endoscopic examination of the nasal cavity, CT of the nose and adjacent nasal cavities, performed functional examinations, maximum preservation of the mucous membrane of the nose and cavities, anatomical bone structures , correcting their configuration.Strong curvature of the nasal septum is one of the most common local factors associated with the lateral pathology of the nasal cavity. Disruption of nasal breathing leads to changes in mucociliary clearance and creates conditions for inflammation in paranasal cavities. In this regard, there is a need to sanitize the center of chronic infection and anatomical correction of nasal structures. Modern medical advances allow expanding the scope of joint surgical operations. In the literature, there are pathological processes in the area of the nasal septum, deformations of the structures of the lateral wall of the nasal cavity, and the natural opening of the nasal cavities; perforative odontogenic maxillary sinusitis; issues related to the implementation of typical variants of joint operations in the finger-like protrusions of the paranasal sinuses combined with the damage of the orbit have not yet been clarified [5-8]. Although in joint operative practices, to one degree or another, injuries of the mucous membrane occur in different areas of the nasal cavity, the problem of prevention and treatment of post-operative traumatic bleeding becomes extremely important [4-12]. The hemostatic effect of tamponade is, on the one hand, a strong mechanical pressure on the bleeding vessel, and on the other hand, keeping the blood in the nasal cavity, which ensures faster blood clotting and faster thrombus formation in the vessel. However, this method of stopping bleeding from the nose is quite traumatic for the mucous membrane of the nasal cavity, causing its dysfunction and causing significant pain in patients. Tampon removal is also a painful process. In addition, the presence of a gauze tampon in the nasal cavity is accompanied by strong inflammatory changes of the mucous membrane, accompanied by the appearance of signs of intoxication. The purpose of the research is to conduct clinical-functional and morphological studies of the mucous membrane of the nasal cavity in joint surgical procedures. passes with the appearance of signs of intoxication. The purpose of the research is to conduct clinical-functional and morphological studies of the mucous membrane of the nasal cavity in joint surgical operations. passes with the appearance of signs of intoxication. The purpose of the research is to conduct clinical-functional and morphological studies of the mucous membrane of the nasal cavity in joint surgical operations.Purpose of the work: Assessment of the morpho-functional state of the nasal mucosa after simultaneous surgery.
2. The Obtained Results and Their Discussion
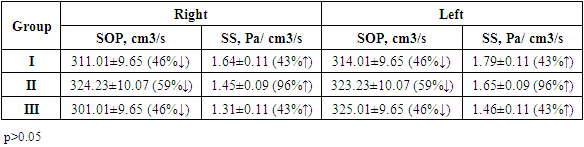
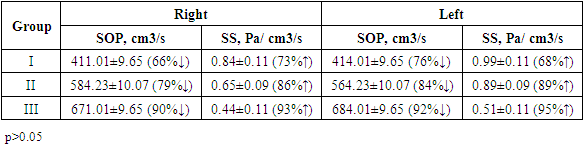
- Research materials and methods in 2021-2022, 60 patients with diseases of the nose and paranasal cavities were comprehensively examined and treated at the otorhinolaryngology department of the multidisciplinary clinic of the Tashkent Medical Academy. Combined surgical procedures were performed in these patients, and clinical-functional, morphological, microbiological studies were conducted on the effectiveness of hemostatic agents.In order to investigate nasal breathing or nasal ventilation, we studied rhinopneumometry indicators (Table 1).
|
|
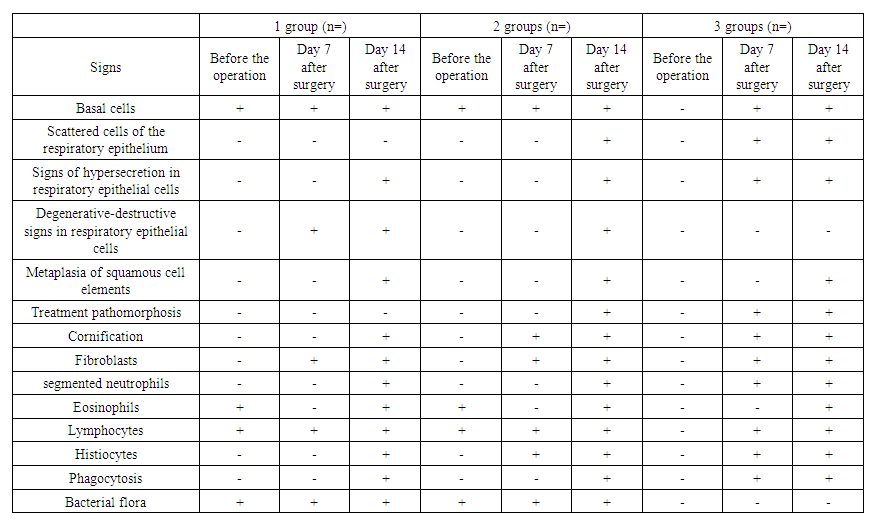 | Table 3. In rhinopathologies, the state of the mucous membrane of the nasal cavity is on a rhinocytogram |
3. Conclusions
- 1. Changes in the surrounding anatomical structures of the nasal septum specific to the type of curvature of the nasal septum develop, changes in the functional state of the nasal cavity with 3-4 and mixed types of the nasal septum. mucociliary transport in joint pathological conditions of tissues - 29.1 min, Ph-7.36, absorption activity - 78.2, secretion activity - 49.3 mgr. Therefore, it is advisable to correct the nasal septum and anatomical structures located close to it in patients; 3. Experimental studies have shown that collagen "Splint" does not have damaging and local effects in the early stages. The effect of the surrounding tissue on the sponge is insignificant and non-inflammatory. Adhesion of collagen fibrils of the sponge to the layers of mucous membrane structures in the periphery is observed in the late periods of the study;2. The use of collagen "Splint" as an alternative to gauze tamponade of the nasal cavity in joint surgical operations in the nasal cavity, due to the reduction of the volume of complications during and after the operation in patients, strong trophic changes of the mucous membrane and pain reduction made it possible to improve the results of treatment.3. Cytological examination of smears taken from the mucous membrane of the nasal cavity taken from patients with various rhinopathologies in the post-operative period showed that the regenerative processes of the mucous membrane of the nasal cavity were strengthened after surgery using slplint in group 3 patients brought The results of cytological studies have once again confirmed the effectiveness of using the splint in the practice of otorhinolaryngologists.4. Experimental studies have shown that collagen "Splint" does not have damaging and local effects in the early stages. The effect of the surrounding tissue on the sponge is insignificant and non-inflammatory. The use of collagen "Splint" as an alternative to gauze tamponade of the nasal cavity in joint surgical operations in the nasal cavity, due to the reduction of the volume of complications during and after the operation in patients, strong trophic changes of the mucous membrane and pain reduction made it possible to improve the results of treatment.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML