-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(7): 946-948
doi:10.5923/j.ajmms.20231307.22
Received: Jun. 19, 2023; Accepted: Jul. 15, 2023; Published: Jul. 24, 2023

Mosaic Variant of Turner Syndrome
Kamola Raxmanberdiyevna Akhmedova, Nasiba Usmanovna Alimova, Malika Muzafarovna Mahmudova, Elena Leonidovna Kim, Akida Sattarovna Sadikova, Feruza Zafarjanovna Yuldasheva
Republican Specialized Scientific and Practical Medical Center named after Academician Y.H. Turakulov, Toshkent, Uzbekistan
Correspondence to: Kamola Raxmanberdiyevna Akhmedova, Republican Specialized Scientific and Practical Medical Center named after Academician Y.H. Turakulov, Toshkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In a number of cases the mosaic variant is diagnosed late due to a less pronounced clinical picture compared to the full form of the disease. Pediatricians should pay attention to the weight and height parameters of patients, compare these results with those of their parents and refer patients to an endocrinologist, gynecologist and geneticist if the growth rate decreases.
Keywords: Mosaic variant
Cite this paper: Kamola Raxmanberdiyevna Akhmedova, Nasiba Usmanovna Alimova, Malika Muzafarovna Mahmudova, Elena Leonidovna Kim, Akida Sattarovna Sadikova, Feruza Zafarjanovna Yuldasheva, Mosaic Variant of Turner Syndrome, American Journal of Medicine and Medical Sciences, Vol. 13 No. 7, 2023, pp. 946-948. doi: 10.5923/j.ajmms.20231307.22.
1. Introduction
- Turner syndrome (TS) is the most common chromosomal abnormality, occurring in one in 2000 live birth girls. ST is associated with complete or partial loss of the X chromosome. The main features of the disease are short stature and delayed puberty.In 40-50% of cases there is a complete form of the syndrome - monosomy 45,X. In the complete form the disease is more severe compared to mosaic karyotype 45,X/46,X, which occurs in 15-25% of cases. In girls with mosaicism, congenital heart abnormalities and lymphoedema are less common and less severe; mosaicism 45,X/47,XXX has a milder phenotype. A Y-chromosome 45,X/46,XXX may be present in 10-12% of cases (the Y chromosome is only found in some cells, because the presence of the Y chromosome in all cells excludes ST); a mosaicism of 45,X/47,XXX or 45,X/46,XX/47,XXX may occur in 3% of cases.In addition, the following defects are sometimes found in the X chromosome: partial or complete deletion of the long or short arm of the X chromosome;two copies of the long arm of the X chromosome with a complete or partial absence of the short arm;ring X chromosome deletion with loss of parts of the short and long arms of the X chromosome.According to foreign statistics, in patients with the mosaic form of ST, menarche may occur in 57-67% of cases, 14% have problems with fertility, and 64.3% have short stature.Clinically, the syndrome is characterised by stunting, hypergonadotropic hypogonadism, and abnormalities such as wing folds in the neck, low hair growth, ptosis, epicanthosis, high gothic palate, micrognathia, and rotated auricles. A number of abnormalities of different organs and systems are seen in this disorder: coarctation of the aorta, aneurysm/expansion of the aorta, horseshoe kidney, abnormal position/duplication of the renal pelvis, ureters or vessels, autoimmune diseases.At present, most girls with ST, with timely hormone therapy (growth hormone and estrogen-gestagen replacement hormone therapy), show near age-matched puberty. Subsequently, these patients can plan a pregnancy with the help of assisted reproductive technologies with donor programmes.The mosaic variant of the ST karyotype deserves special attention and is often diagnosed late due to a poor clinical picture. The prevalence of spontaneous menarche for 45.X is 6-30%, mosaic variants 54-67%. Mosaic patients are characterised by low growth in only 64.3% of cases, whereas in the complete form more than 90% of cases are characterised by stunted growth (1-8). An article by R. Tang et al. presented a clinical case of a patient with ST who had hypothyroidism of autoimmune origin. Only in the absence of menstruation during puberty, a karyotypic study (found to be 47.XXX/45.X) was carried out confirming the presence of ST (9). In contrast to monosomy, a mosaic karyotype is characterised by a higher rate of spontaneous pregnancy. For example, the foreign literature describes a spontaneous pregnancy in a girl with ST who was diagnosed with a mosaic karyotype at the age of five years. The pregnancy proceeded without abnormalities and a healthy baby girl was born at 38 weeks of gestation by caesarean section - 46.XX [10].
2. Clinical Case
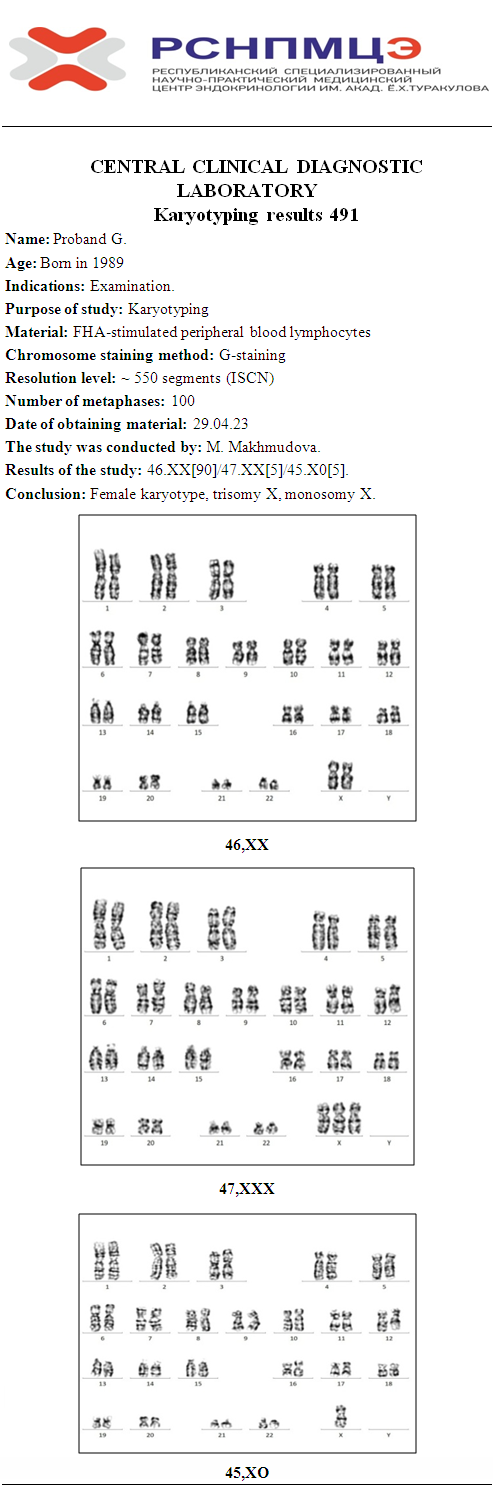
- Patient G., 34 years old, was referred to the Republican Specialized Scientific-Practical Medical Center of Endocrinology named after Academician Y. H. Turakulov of the Ministry of Health of the Republic of Uzbekistan. The patient was referred to the Republican Specialized Scientific-Practical Medical Center of Endocrinology named after Academician Y. H. Turakulov of the Ministry of Health of the Republic of Uzbekistan by an endocrinologist in May 2023 due to complaints of obstructive obstetric history.She had a history of unmarried proband, no occupational hazards in her parents, and an unhealthy heredity. Proband from 1 pregnancy, 1 childbirth. Mother's age at the time of delivery was 36 years. Delivered on time, physiological. Crying and feeding at once. BPD -2200 grams. Menarche at the age of 12-13 years. Allergoanamnesis is not aggravated, genealogical history of no features, vaccinated according to calendar plan. Proband grew and developed in a timely manner, according to sex and age. She had had HAI, mumps, VO.Proband married, unrelated marriage, occupational hazards denied, heredity not aggravated.A history of obstetric complications:1 pregnancy (2017) - failed at 5 weeks' gestation.2 pregnancy (2019) - 7 weeks' gestation without progression.3rd pregnancy (2021) - 7-8 weeks' gestation and not confirming.Currently registered at an endocrinologist with the diagnosis: Diffuse goiter. Euthyroidism, a gynaecologist with a diagnosis of ARPO, bicornic uterus. Habitual pregnancy (3 failed pregnancies).Phenotype: Reaction to examination adequate, asthenic physique. Skin clean, moderately moist. Visible mucous membranes are clean, pink and moist. There was no oedema. Movement in the joints was full and painless. Peripheral lymph nodes were not enlarged. Thyroid gland was enlarged, dense and nodes were not detected on palpation. There were no signs of parathyroid gland dysfunction. Above the lungs there was a clear pulmonary sound, vesicular breathing, no rales. Cardiac tones are clear, rhythmic, no murmurs are heard. Percussive boundaries of the heart are within the age norm. The abdomen is soft, painless, the liver and spleen are not enlarged on palpation. Stool is regular, regular, clear, urination is free, painless, tapping symptom is negative on both sides. Gynecological status: no menstruation, no discharge, feminine hair, pubic and axillary hair, external genitalia correctly developed, clitoris not enlarged, hymenal fimbriae, not hyperemic, oestrogenic. The vulval mucosa is pink on examination.Sexual development formula: Ah3, Ma3, Pb3, Me 12-13. In the mammary glands palpated glandular tissue without focal thickening, nipple pigmented.FD - 171 cm. FS - 55 kg.Results of pelvic ultrasound: bicornic uterus, dimensions - 50 × 42 × 60 mm, M-echo homogeneous, right horn - endometrial thickness 9.8 mm, left horn - 9.2 mm. Ovaries b/o. Small pelvis: no fluid in the douglas-field. Conclusion: Echoes of a bicornic uterus. The ultrasound of the thyroid gland - echosigns of diffuse goiter.According to the cytogenetic study, dated April 29, 2023, the study revealed a mosaic karyotype consisting of a normal set of chromosomes, from a clone of cells with X monosomy and trisomy X: mos46.XX(90%)/47.XXX(5%)/45.X0(5%).
 She has not consulted a geneticist or endocrinologist until now, as she has not had any complaints of delayed physical or sexual development. She has not received any hormone replacement therapy. Patient G. has no stigmata of disembryogenesis, most likely due to the presence of most cells with a normal chromosome set (46.XX).
She has not consulted a geneticist or endocrinologist until now, as she has not had any complaints of delayed physical or sexual development. She has not received any hormone replacement therapy. Patient G. has no stigmata of disembryogenesis, most likely due to the presence of most cells with a normal chromosome set (46.XX).3. Conclusions
- This clinical case confirms the need for a thorough history of pregnancy failure and infertility, together with geneticists, endocrinologists, and, in the presence of phenotypic findings of short and tall stature in the family, the correlation of the child and parental weight and height parameters during routine pediatric examinations and examinations by other specialists. When Turner syndrome is suspected and phenotypic manifestations of this chromosomal abnormality (wing folds in the neck, low hairline at the nape of the neck, low-slung auricles, edema of the feet) are found, patients should be referred to a pediatric gynecologist, endocrinologist and geneticist.Timely diagnosis of the disease and timely initiation of hormone replacement therapy can improve the quality of life of patients, normalise their social adaptation, and prepare them for the realisation of reproductive function through assisted reproductive technology (IVF).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML