Khudaynazarov D. A., Muminov Sh. M., Nizov O. N., Minaev T. R., Khakimov A. B., Tashkhodzhaev A. A.
Republican Scientific Center for Emergency Medical Care of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan
Correspondence to: Khudaynazarov D. A., Republican Scientific Center for Emergency Medical Care of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Aim: to analyze the structure of severe open combined injuries of the upper extremities with circulatory disorders. Material and methods: For the period from 2001 to 2021, 565 patients with severe combined (bone-vascular) injuries of the upper limbs were treated at the RRCEM. There were 471 men (83.4%), women - 94 (16.6%). At the same time, there were 110 (19.5%) children aged 1–17 years, 408 (72.2%) patients of the most able-bodied age (from 18 to 60 years), 47 (8.3%) patients over the age of 61 years. %). All patients had damage to the main vessels with varying degrees of circulatory disorders in the distal extremities. Results: The analysis of the obtained results showed that despite the complexity of the combined osteovascular injuries of the upper extremities, 484 (85.7%) patients underwent restorative interventions. In all cases, in the postoperative period, patients received therapy aimed at preventing and treating secondary infections, improving blood rheology, infusion therapy, blood and plasma transfusions, and anticoagulants. The number of favorable outcomes after reconstructive surgery is quite large - 446 (92.1%) cases, which correlates with published data on other specialized clinics in the world.
Keywords:
Upper limbs, Concomitant injuries, Analysis
Cite this paper: Khudaynazarov D. A., Muminov Sh. M., Nizov O. N., Minaev T. R., Khakimov A. B., Tashkhodzhaev A. A., Treatment of Patients with Severe Open Bone and Vascular Injuries of Large Segments of the Upper Limbs, American Journal of Medicine and Medical Sciences, Vol. 13 No. 7, 2023, pp. 928-936. doi: 10.5923/j.ajmms.20231307.19.
1. Relevance of the Problem
Currently, the treatment of open bone and vascular injuries of the upper extremities is one of the pressing problems of surgery during peacetime. The emergence of a large number of private enterprises, non-compliance with safety rules, and a significant increase in road accidents inevitably lead to an increase in the overall number of open injuries of the upper extremities, as well as to the aggravation of the nature of the injuries. According to several authors [1,2,3], closed limb fractures are accompanied by secondary damage to major arteries and veins in 1.7-2% of cases. At the same time, open bone and joint injuries of the upper extremities are combined with injuries to major vessels in more than 32.6% of cases. Disability after such injuries reaches 32.2% of the total number of lost work capacity. Currently, due to the rapid development of angio- and microsurgery, early timely diagnosis (pulse oximetry, MSCT angiography, CDS, etc.), timely performance of reconstructive surgeries, the frequency of primary amputations of the upper extremities has significantly decreased. However, absolute general contraindications to the performance of reconstructive surgeries are considered to be the general severe condition of patients, caused by concomitant injuries of internal organs, severe head injuries, multiple bone fractures, as well as the presence of severe chronic diseases. Local contraindications include destruction of limb segments, high level of damage, and the patient's arrival time exceeding the permissible time for revascularization [3-11].Trauma of a traction-crushing nature represents a particular severity in terms of treatment, which has recently become more common. The tightening of the limb into a rotating mechanism leads to ruptures of vessels and nerves at different levels, muscle contusions along the length, as well as multiple open fractures and dislocations. Such injuries themselves pose a danger to life; performing reconstructive surgeries in such cases is associated with significant difficulties, which explains the high percentage of primary amputations. Injuries from electric saws and stab-cutting wounds occur much less frequently and are the most favorable in terms of reconstruction, primarily due to the damage to anatomical structures at one level.Upon admission of patients in a state of traumatic and hemorrhagic shock, the surgeon is often faced with a dilemma: to perform a reconstructive operation, often associated with a risk to the patient's life, or to perform primary amputation, which takes much less time but inevitably leads to the patient's disability. According to most authors, an individual approach is necessary in each specific case when choosing a treatment strategy [10,11,12].
2. Materials and Methods
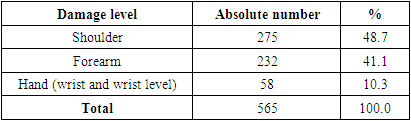
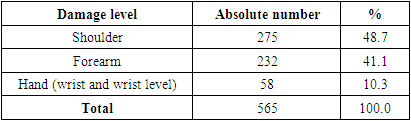
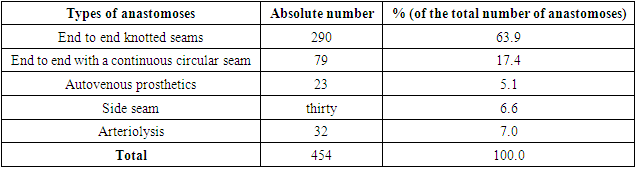
During the period from 2001 to 2021, 565 patients with severe combined (bone-vascular) injuries of the upper extremities were treated at the RRCEM. There were 471 men (83.4%) and 94 women (16.6%). At the same time, there were 110 children aged 1-17 years (19.5%), 408 patients of the most working age (18-60 years) (72.2%), and 47 patients over 61 years old (8.3%). All patients had injuries to major blood vessels with varying degrees of impaired blood circulation in the distal parts of the limbs. The distribution of patients by the level of injury is presented in Table 1.Table 1. Distribution of patients according to the level of damage
 |
| |
|
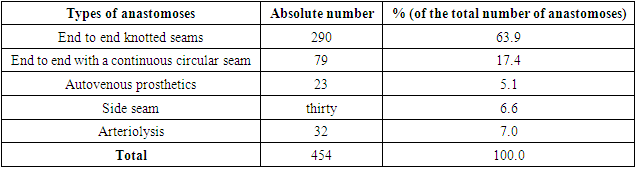
We did not set the task of analyzing the prospects for treating such injuries in women. However, we believe that the prospects for recovery depend primarily on the mechanism of the injury and the quality of the operation performed. Therefore, we did not discuss the differences between men and women. Division by gender in statistics is standard.In this article, the authors do not provide results on lower limb injuries. It can be said unequivocally that the percentage of reconstructive surgeries is significantly lower in cases of lower limb injuries, which is often due to the mechanism of the injury itself: railway accidents, car crashes, crush injuries, compression. Often, such victims arrive with complete crushing of the damaged segments, which makes reconstructive surgery impossible.The majority of patients, 401 (71%), were admitted to the Center within the first three hours after the injury, which is the most favorable time for reconstructive surgery. 254 (45%) patients were delivered by ambulance, 179 (31.7%) were transported without first aid, and 132 (23.4%) were referred from other hospitals. Of these, 144 (25.5%) patients had symptoms of shock of the first degree, 89 (15.8%) had symptoms of shock of the second degree, and 46 (8.1%) had symptoms of shock of the third degree. Shock symptoms were not present in the remaining 286 (50.6%) patients. General examination methods included collecting complaints and history, external examination, hemodynamic data (pulse, blood pressure), general clinical tests, ECG, and chest X-ray. If necessary, patients were examined by related specialists (traumatologist, neurosurgeon, thoracic or abdominal surgeons). In addition, all 565 patients underwent pulse oximetry and X-ray of the affected segments. CDS was performed in 140 (24.8%) patients, and arteriography in 9 (1.6%). Pulse oximetry was performed on a "Nihon Kohden" device, and X-ray was performed on a "Duodiagnost - Phillips" device. In cases of complex multi-level bone injuries, intraoperative X-ray, performed on a "C-Arm" device by Siemens, allowed for the control of repositioning and osteosynthesis of fragments during the operation. CDS was performed on an ND 11XE device by Philips, and angiography was performed on an "Allura 20 FD" device by Philips, Netherlands. Reconstructive interventions were performed on 484 (85.7%) patients, and primary amputation was performed on 81 (14.3%) patients. The reasons for the latter were shock of the third or fourth degree, lack of conditions for reconstructive surgery (severe segmental crushing), and the presence of severe concomitant trauma (thoracic and abdominal organs, severe head injury).During osteosynthesis in 484 patients, spokes were used as fixators in 408 (84.3%) cases, pins in 46 (9.5%) cases, rod devices in 12 (2.5%) cases, and Ilizarov's device in 18 (3.7%) cases. Reconstructive vascular surgery was performed on 454 (93.8%) patients. Types of vascular interventions are presented in Table 2.Table 2. Types of vascular interventions
 |
| |
|
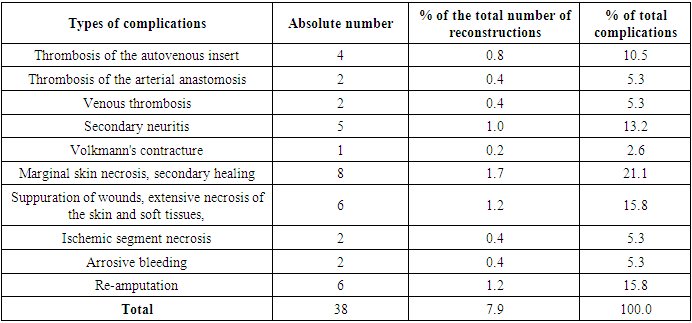
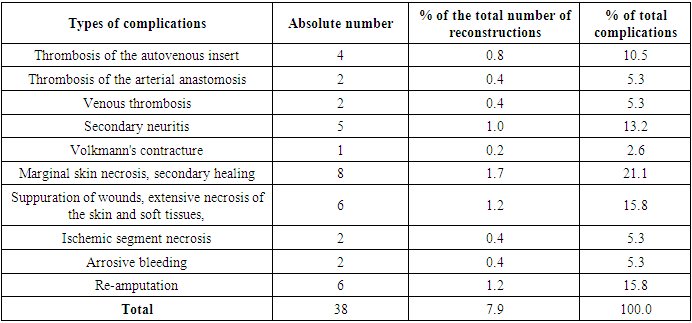
Of the remaining 30 (6.2%) patients, taking into account compensation of blood circulation, vessel ligation was performed. Out of 484 reconstructive surgeries performed, primary wound healing with preservation of the limb segment was achieved in 446 (92.1%) cases. In 38 (7.9%) cases, complications developed, the structure of which is presented in Table 3.Table 3. Structure of postoperative complications
 |
| |
|
Clinical case 1. Patient: K. Age: 25 years old. Date of admission: 04/05/14. Medical history number: 13352.Medical history: One hour before admission, the patient suffered an injury from an electric saw.Diagnosis: Complete traumatic amputation (by electric saw) of the left hand at the level of the radiocarpal joint. First-degree traumatic shock.The type of limb and the X-ray upon admission are presented in Figures 1-2. | Figure 1. View of the limb of the patient K |
 | Figure 2. X-ray |
Operation performed - REPLANTATION of the detached segment. Stages of the operation:1. Primary surgical debridement of the segment wound and cults, revision and marking of structures2. Removal of the first row of wrist bones and osteosynthesis with three Ilizarov spokes3. Anastomosis of the ulnar artery, three dorsal veins.4. Restoration of the tendons of the wrist and finger extensors and flexors5. Restoration of the median, ulnar, and superficial branch of the radial nerve.The stages of the operation are presented in figures 3-10.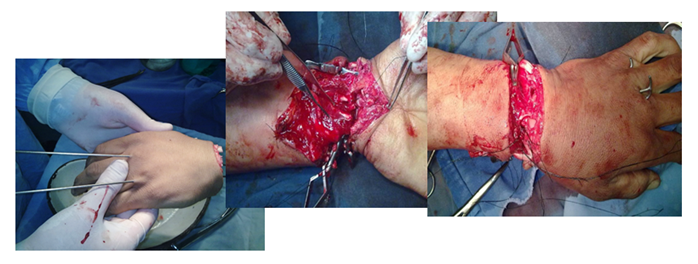 | Figure 3-5. Stage of osteosynthesis with wires |
 | Figure 6. Anastomosis of the ulnar artery |
 | Figure 7. Anastomosis of the dorsal veins |
 | Figure 8-10. View after surgery and pulse oximetry |
The view on the 7th day and the control radiograph are shown in fig. 11 - 14. | Figure 11-14. View of the limb and control radiograph |
 | Figure 15. Full recovery of function after 5 months |
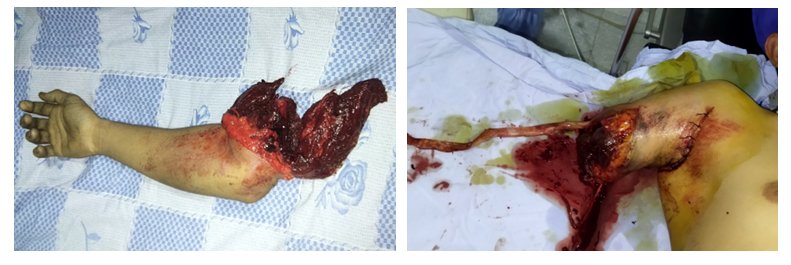
Clinical case 2. Patient: E-v. Age: 26 years. Admission date: 26.10.2021. ID number: 37368.History: Two hours before admission, the patient sustained an injury while working on a combine harvester - his hand got caught in the rotating blades. After the injury, the patient was taken to a district hospital, where the wound in the armpit area was sutured, a bandage was applied to the wound on the forearm, and the segment was wrapped in a package. The patient was then transferred to the Regional Emergency Medical Center along the ambulance line.DIAGNOSIS: Complete traumatic traction amputation of the right upper limb at the level of the shoulder joint. Sutured wound in the right armpit area. Traumatic shock of the second degree. The appearance of the amputated segment, the wound on the forearm, and the X-ray are presented in figures 16-18.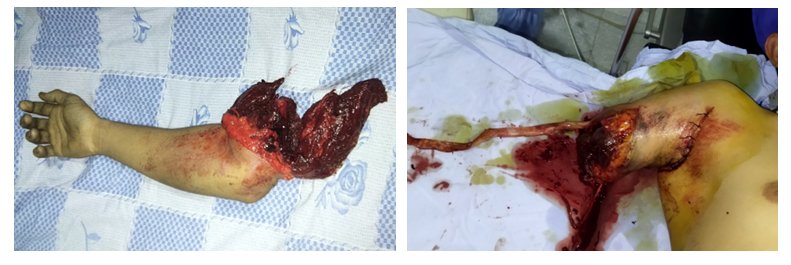 | Figure 16-17. View of the severed segment and the wound of the stump of the patient E |
 | Figure 18. X-ray of the patient E |
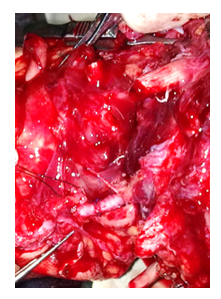
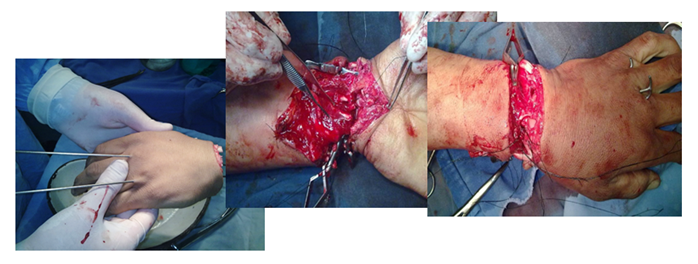
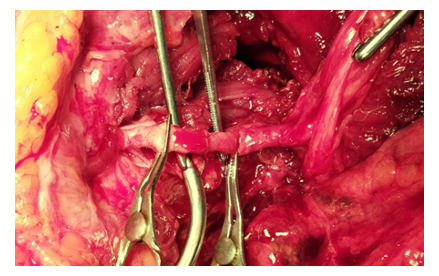
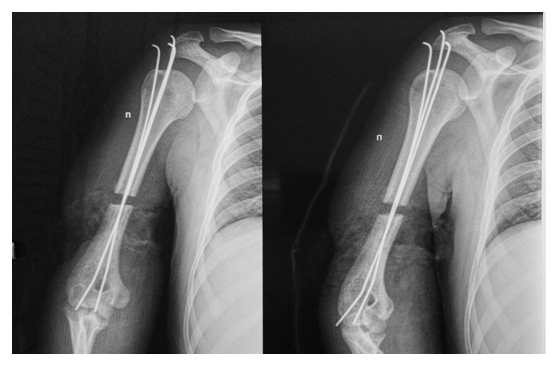
Debridement and revisionResection of bone fragments (total shortening in the humerus and segment - 8 cm) and osteosynthesis of the humerus with Ilizarov wires.Anastomoses of the brachial artery (d=5 mm), vena comitans (d=2.5 mm), and basilic vein (d=7 mm).Restoration of musclesAnastomosis of the cephalic vein (d=5 mm).Restoration of the median nerve with epineural sutures, transposition of the ulnar nerve to the area of the forearm. There were no conditions for the restoration of the radial nerve.We did not always conduct monitoring of the restoration of function. In the cases presented in the article, the first case (replantation of the hand) resulted in complete restoration of function, while in the second case (replantation at the shoulder level), there was a sharp limitation of elbow joint function and flexion of the hand and fingers, as well as complete absence of active extension of the hand and fingers due to the absence of the radial nerve. The latter will require a repeat operation, possibly involving a muscle-tendon transfer. | Figure 19. Osteosynthesis of the humerus with knitting needles |
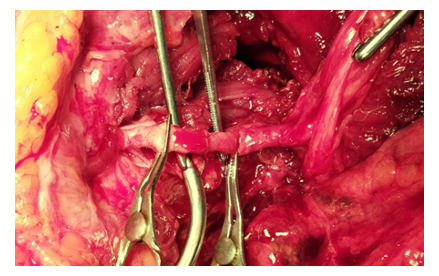 | Figure 20. Anastomosis of the brachial artery |
 | Figure 21. View after restoration of structures: a.brachialis, v.commitans, n.medianus, proximal end of n.ulnaris, v.basilica |
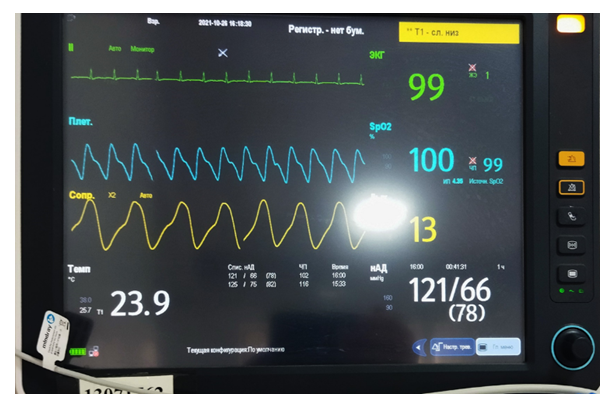
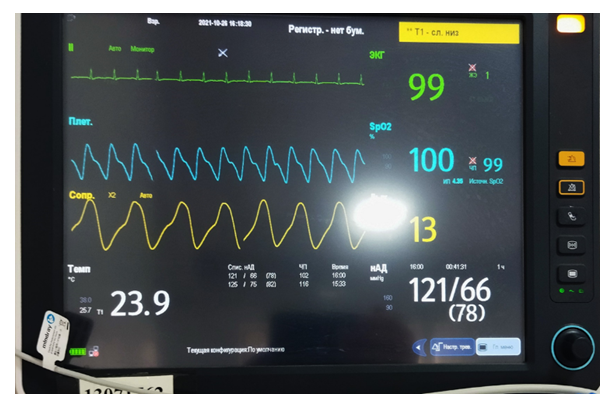 | Figure 22. Pulse oximetry |
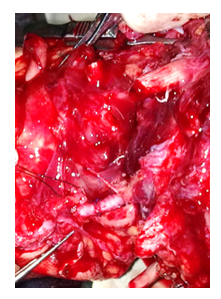
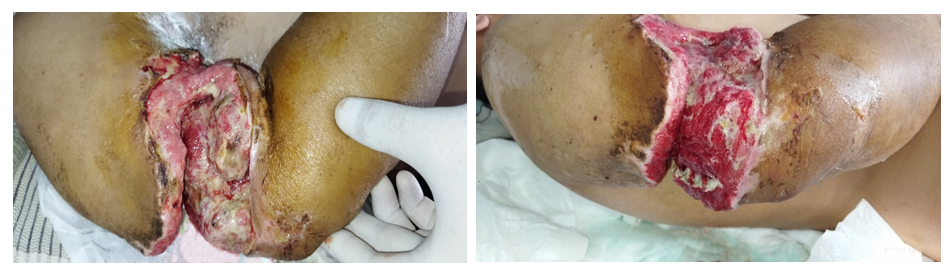
The appearance of the limb after the operation is shown in Figure 23. Subsequently, the patient developed suppuration and muscle necrosis, which required step-by-step necrectomy until the wound was completely cleaned and granulation tissue grew well (Figures 24-28). On the 29th day, a full-thickness autodermoplasty was performed, which completely healed (Figures 29-34). | Figure 23. View after the operation |
 | Figure 24. View on the 3rd day – evident edema |
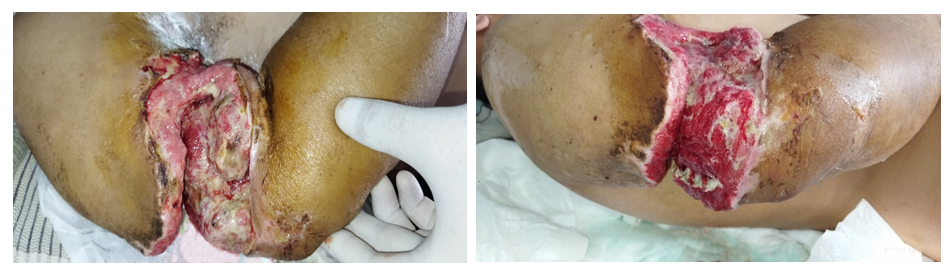 | Figure 25-26. 8th day - suppuration and necrosis of muscles; staged necrectomy |
 | Figure 27-28. Growth of granulation tissue; the imposition of secondary sutures on the granulation |
(19th day after replantation). | Figure 29-31. Free autodermoplasty with a full-thickness graft (29th day after replantation) |
 | Figure 32-34. View of the limb on day 11 after ADP (day 40 after replantation) |
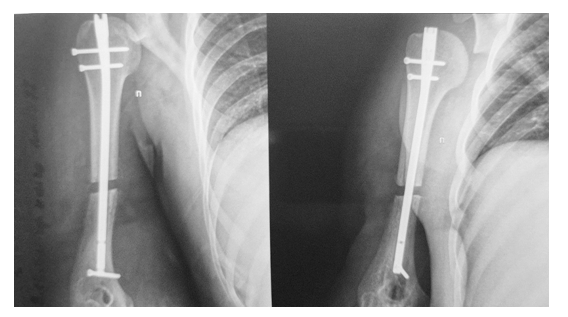
Due to unstable fixation and the presence of diastasis between the bone fragments, osteosynthesis of the humerus was performed with a BIOS pin (Fig. 35, 36).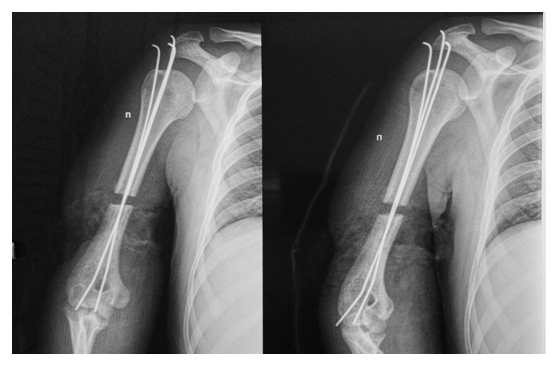 | Figure 35. Unstable fixation and the presence of diastasis between bone fragments |
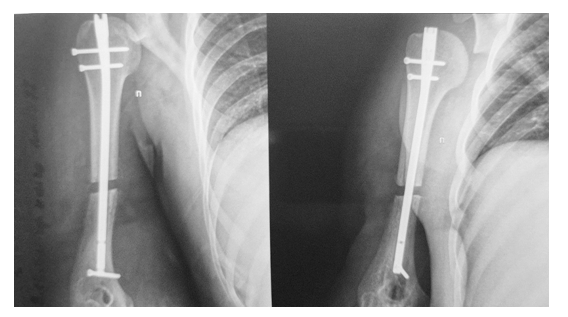 | Figure 36. Osteosynthesis of the humerus with a BIOS pin: 13 days after ADP and 42 days after replantation |
The view of the limb on the 7th day after osteosynthesis on the 48th day after replantation is shown in Figures 37 and 38. | Figure 37-38. View on the 7th day after osteosynthesis. 48th day after replantation |
In this case, despite the postoperative complications that developed in the form of wound suppuration and muscle necrosis, after step-by-step necrectomy, plastic surgery, and repeated osteosynthesis, segment engraftment was achieved.
3. Discussion of Results
The article discusses the challenges of treating open combined bone and vascular injuries of the upper extremities. Despite the severity of such injuries, the development of new technologies, such as precision microsurgical techniques, the use of optical magnification, modern pharmacotherapy, as well as equipping medical centers with necessary equipment for early and rapid diagnosis, and staffing operating teams with specialists of various profiles, allow for reconstructive surgeries to be performed in the shortest possible time. However, the percentage of primary amputations remains significant. The reasons for this are primarily significant destruction of segments, as well as the presence of severe concomitant injuries in cases of polytrauma, when the patient's general condition does not allow for reconstructive surgeries. The analysis of the results showed that despite the complexity of combined bone and vascular injuries of the upper extremities, restorative interventions were performed on 484 (85.7%) patients. In all cases, patients received therapy aimed at preventing and treating secondary infection, improving blood rheology, infusion therapy, blood and plasma transfusions, and anticoagulants. The number of favorable outcomes after reconstructive surgeries is quite high - 446 (92.1%) cases, which correlates with published data on other specialized clinics in the world. Two completely different cases of complete limb segment amputation are presented as clinical examples. In both cases, replantations were performed. However, in the second case, with traction amputation at the shoulder level, such serious complications as muscle suppuration and necrosis developed in the postoperative period, which posed a real threat of erosive bleeding and limb loss. Nevertheless, timely and radical necrectomy with prolonged wound sanitation and subsequent granulation created conditions for skin plasty, which was performed. Repeated osteosynthesis was a forced measure due to the instability of the fracture. Of course, counting on full restoration of limb function in this case is not possible. However, the preservation of the hand as an organ should undoubtedly be regarded as a positive result.
4. Conclusions
1. In cases of open combined trauma of large segments of the upper extremities accompanied by circulatory disorders, traumatic and hemorrhagic shock, the priority remains to save the patient's life.2. Reconstructive operations can only be performed in specialized centers equipped with the necessary equipment and qualified specialists of various profiles.3. Radical surgical treatment of wounds, reliable osteosynthesis, and restoration of adequate blood circulation are the primary conditions for the successful completion of the operation.4. Careful observation of patients in the postoperative period will help to take timely measures in case of a threat of fatal complications and avoid them in time.5. We believe that although anastomosis of vessels with nodal sutures takes more time, it is the preferred method when dealing with vessels with a diameter of less than 5 mm in adults, as well as in all cases of vascular damage in children, as this reduces the likelihood of stenosis of the anastomosis. 6. We believe that reducing the frequency of skin necrosis is achieved by radical excision of tissues within visibly healthy limits during primary surgical treatment. However, it is not always possible to clearly differentiate clearly crushed tissues from tissues with questionable blood supply. In such cases, we leave these areas of skin unexcised.
References
| [1] | Абышов Н.С. Ближайшие и отдалённые результаты при травматических повреждениях артерий конечностей. Ангиол и сосуд хир. 2002; 8 (4): 103-110 [Abyshov N.S. Blizhayshie i otdalennye rezul'taty pri travmaticheskikh povrezhdeniyakh arteriy konechnostey. Angiol i sosud khir. 2002; 8 (4): 103-110. In Russian] |
| [2] | Афанасьев Л.М., Агаджанян В.В., Якушин О.А. К вопросу об организации помощи больным с полными, неполными отрывами и открытыми сочетанными повреждениями сосудов, нервов, сухожилий конечностей. VI съезд травматологов-ортопедов Узбекистана. 2002: 11-13 [Afanas'ev L.M., Agadzhanyan V.V., Yakushin O.A. K voprosu ob organizatsii pomoshchi bol'nym s polnymi, nepolnymi otryvami i otkrytymi sochetannymi povrezhdeniyami sosudov, nervov, sukhozhiliy konechnostey. VI s"ezd travmatologov-ortopedov Uzbekistana. 2002: 11-13. In Russian] |
| [3] | Белоусов А.Е. Пластическая, реконструктивная и эстетическая хирургия. СПб.: Гиппократ. 1998: 744 [Belousov A.E. Plasticheskaya, rekonstruktivnaya i esteticheskaya khirurgiya. SPb.: Gippokrat. 1998:744. In Russian] |
| [4] | Бялик Е.И. Определение операбельности тяжелопострадавших со сложными переломами длинных костей конечностей и профилактика осложнений. Материалы городской научно-практической конференции. НИИ СП им. Н.В. Склифосовского. 2000; 136: 17-25 [Byalik E.I. Opredelenie operabel'nosti tyazhelopostradavshikh so slozhnymi perelomami dlinnykh kostey konechnostey i profilaktika oslozhneniy. Materialy gorodskoy nauchno-prakticheskoy konferentsii. NII SP im. N.V. Sklifosovskogo. 2000; 136: 17-25. In Russian] |
| [5] | Датиашвили Р.О. Реплантация конечностей. Москва, «Медицина». 1991:240 [Datiashvili R.O. Replantatsiya konechnostey. Moskva, «Meditsina». 1991:240. In Russian] |
| [6] | Поярков В.Д., Данилов В.А. Коррекция кровообращения при лечении сочетанных травматических повреждений конечностей. Бюл Вост.-Сиб. науч центра СО РАМН 2007; 43: 151-151 [Poyarkov V.D., Danilov V.A. Korrektsiya krovoobrashcheniya pri lechenii sochetannykh travmaticheskikh povrezhdeniy konechnostey. Byul Vost. -Sib. nauch tsentra SO RAMN 2007; 43: 151-151. In Russian] |
| [7] | Фомин В.Н. Лечение повреждений магистральных сосудов конечностей в условиях центральной районной больницы. Вест хир. 2008; 167(6): 127-128 [Fomin V.N. Lechenie povrezhdeniy magistral'nykh sosudov konechnostey v usloviyakh tsentral'noy rayonnoy bol'nitsy. Vest khir. 2008; 167(6): 127-128. In Russian] |
| [8] | Штейнле А.В. Ангиография при повреждениях магистральных сосудов конечностей (исторический обзор). Сиб мед журн. 2008; 23(1): 99-112 [Shteynle A.V. Angiografiya pri povrezhdeniyakh magistral'nykh sosudov konechnostey (istoricheskiy obzor). Sib med zhurn. 2008; 23(1): 99-112. In Russian] |
| [9] | Bhandari M., Guyatt G.H., Khera V. et al. Operative management of lower extremity fractures in patients with head injuries. Clin. Orthop. Relat. Res. 2003; (407): 187-198. |
| [10] | Cakir O, Subasi M, Erdem K, Eren N. Treatment of vascular injuries associated with limb fractures. Ann R Coll Surg Engl. 2005; 87(5): 348-52. |
| [11] | Friedel R., Dorow C., Markgraf E. Amputation injures of the supper extremity - early complications after rер1аntаtion and revascularization. // Unfallchirurgie. 1993; 19(4): 298 – 302. doi: 10.1007 / BF02588125. |
| [12] | Pape H., Stalp M., Dahlweid M., Regel G., Tscherne H. Optimal duration of primary surgery with regards to a "vorderline"-situation in polytrauma patients. Unfallchirurg. 1999; 102(ll): 861-869. Article in German. |


















 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML