-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(7): 917-919
doi:10.5923/j.ajmms.20231307.16
Received: Apr. 16, 2023; Accepted: Jun. 19, 2023; Published: Jul. 12, 2023

Shifts in Cytokine Status in Chest Trauma Complicated by Shock
Nutfullo Rakhmonov1, Mamur Abdurakhmanov2, Zufar Abdurakhmanov2
1Department of Thoracic Surgery, Bukhara Branch of Republican Scientific Center of Emergency, Bukhara, Uzbekistan
2Department of Surgical Diseases and Intensive Care, Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Zufar Abdurakhmanov, Department of Surgical Diseases and Intensive Care, Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

One of the factors in the progression of inflammation caused by traumatic injury is the dysfunction of the immune defense, which is regulated by inflammatory mediators. Objective. To determine the dynamics of the content of cytokines with pro- (IL-6, IL-8, IL-18) and antiinflammatory (IL-4, IL-10) activity in blood plasma in patients with chest trauma (CT) complicated by severe traumatic shock. Materials and methods. In the period from 2019 to 2021, 249 patients with CT of various severity degree were treated. Of them, 41 patients with severe CT and shock of grade II, III who received mechanical ventilation were included in the study, with a mean age of 36,4±6,2 years. 20 healthy volunteers made up the comparison group with a mean age of 35,4±2,3 years, which were comparable with the groups of patients in terms of age and gender. Interleukins were determined in blood serum by enzyme-linked immunosorbent assay. Results. The concentration of IL-8 was high (p<0,05) in all groups of patients in the post-traumatic period up to 5 days compared with the SIRS group without complications. An increase in the concentration of IL-6 in the blood serum was found in all patients with severe CT and traumatic shock during hospitalization within 3 hours in comparison with control group (p<0,05). The concentration of IL-18 also tended to increase in all groups of patients with severe CT at all follow-up periods and reached a peak value within 6 hours after CT. The amount of IL-4 in the blood plasma of patients with combined CT was significantly increased during hospitalization of patients with the subsequent occurrence of severe sepsis within 3 hours, which reached normal values on the 2nd-3rd days, while in affected other groups, the value of those did not statistically differ from normal values. during hospitalization within 3 hours, the concentration of IL-10 in patients with severe sepsis is statistically higher than in patients with SIRS without complications (p<0,05) and SIRS with a focus of infection (p<0,05), but then the concentration of IL-10 did not statistically differ among three groups within 4-6 hours after CT. Conclusions. An increase in the blood concentration of pro-inflammatory cytokines, such as IL-8, IL-18, IL-6 were a statistically significant parameter of SIRS, and anti-inflammatory cytokines such as IL-10, IL-6, IL-4 in the first hours after CT are associated with the occurrence of organ dysfunction and severe sepsis in patients with CT complicated by grade II and III shock.
Keywords: Chest trauma, Cytokine, Shock
Cite this paper: Nutfullo Rakhmonov, Mamur Abdurakhmanov, Zufar Abdurakhmanov, Shifts in Cytokine Status in Chest Trauma Complicated by Shock, American Journal of Medicine and Medical Sciences, Vol. 13 No. 7, 2023, pp. 917-919. doi: 10.5923/j.ajmms.20231307.16.
Article Outline
1. Introduction
- To date, the role of the body's immune defence in the occurrence of inflammation in response to a traumatic factor has been established [1,2]. CT, complicated by shock, contributes to the generalized induction of the main mechanisms of the inflammatory process in the systemic response of the body to traumatic exposure. With the development of moderate and severe traumatic shock, patients often have both signs of SIRS and signs of a septic condition and severe sepsis according to the classification established by R.S. Bone in 1992 [3]. SIRS is a key link in the occurrence of sepsis, post-traumatic shock. Severe CT, post-traumatic shock and severe sepsis are associated with the occurrence of multiorgan failure and generalization of inflammation [4,5], which indicates the generalized nature of the inflammatory process. The pathogenetic basis of the generalized inflammatory process is considered to be the induction of the synthesis of pro-inflammatory cytokines by cellular structures at the site of injury and their release into the bloodstream with the activation of the transition of induced cells from the bone marrow to the microvasculature, which contributes to the development of a systemic inflammatory process [6]. At the same time, the inflammatory process loses its protective function, which is the localization of alteration factors, induces a pathological inflammatory process and contributes to the progression of generalized alteration and multiorgan failure, immune system dysfunction [7].Indicators of the severity of the inflammatory response and generalized inflammation in the early period of the body's inflammatory response to traumatic injury are of particular importance for studying the body's immunoreactivity and predicting the course of the inflammatory process in order to perform timely corrective therapy. In order to achieve a solution to the above issues, we conducted a study of the concentration of cytokines in the blood serum in CT complicated by shock or with the development of SIRS, sepsis and severe sepsis.
2. Materials and Methods
- The sample size was 249 patients with CT of different severity shock degree. 41 patients with severe CT and shock of grade II, III who received mechanical ventilation were included in the study, with a mean age of 36,4±6,2 years. 20 healthy volunteers made up the comparison group with a mean age of 35,4±2.3 years who were hospitalized at the Department of Thoracic Surgery of the Bukhara Branch of Republican Scientific Center of Emergency from 2019 to 2021. The severity of CT was determined using injury severity score (ISS). The inclusion criterion for patients with CT was ISS>16. Informed consent was obtained from the next of kin of the patients.All patients were divided into three groups, taking into account the course of injury and the development of SIRS:1) Group of patients with SIRS, but without infectious complications (n=25);2) Group of patients with SIRS and infection focus (n=12)3) Group of patients with severe sepsis after trauma (n=4).All patients underwent a study of the concentration of IL-8, IL-6, IL-18, IL-4, IL-10 in the blood serum at 3, 6, 24 hours and 3rd and 5th day after injury.
3. Results and Discussion
- According to the obtained data, the concentration of IL-8 was high (p<0,05) in all groups of patients in the post-traumatic period up to 5 days compared with the SIRS group without complications. At the same time, the highest levels of the chemokine were observed during hospitalization in patients with progression of SIRS and the occurrence of a focus of infection and severe sepsis. This phenomenon is explained by the fact that IL-8 is the main cytokine that causes the accumulation of neutrophils at the site of inflammation [8,9].An increase in the concentration of IL-6 in the blood serum was found in all patients with severe CT and traumatic shock during hospitalization within 3 hours in comparison with control group (p<0,05) (Figure 1).
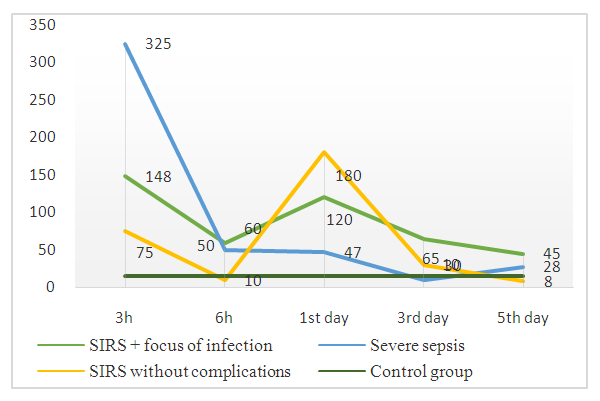 | Figure 1. IL-6 concentration (pg/ml) in blood plasma |
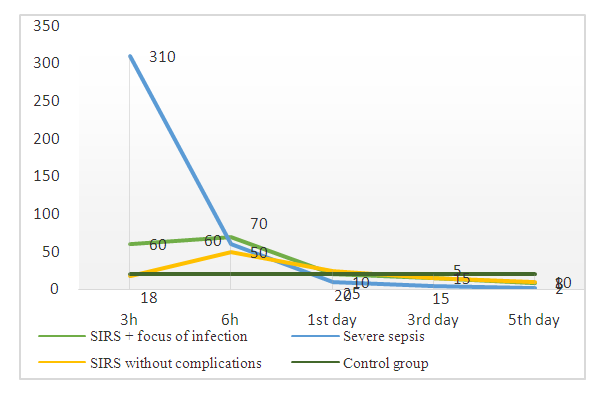 | Figure 2. IL-10 concentration (pg/ml) in blood plasma |
4. Conclusions
- Based on the results of a dynamic study of the concentration of cytokines in the blood plasma of patients with CT complicated by grade II and III shock, it was found that an increase in the blood concentration of pro-inflammatory cytokines, such as IL-8, IL-18, IL-6 were a statistically significant parameter of SIRS, and anti-inflammatory cytokines such as IL-10, IL-6, IL-4 in the first hours after CT are associated with the occurrence of organ dysfunction and severe sepsis. These immunological changes may make it possible to predict SIRS and sepsis in a timely manner and to conduct therapy to prevent the expected severe sepsis in the early post-traumatic period (on the first day after СT).
ACKNOWLEDGEMENTS
- All authors have made significant contributions to the design, execution, analysis and writing of this study, and will share responsibility for the published material. Conflicts of interest: The authors declare no conflicts of interest.Ethics approval: This study was approved by the Institutional Review Board of both institutes, Uzbekistan.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML