-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(7): 913-916
doi:10.5923/j.ajmms.20231307.15
Received: Jun. 4, 2023; Accepted: Jun. 26, 2023; Published: Jul. 12, 2023

Analysis of Factors Influencing the Results of the Laser Obliteration Technique of Short and Complex Rectal Fistulas
Shekhovtsov Stanislav Alexandrovich1, 2, Davlatov Salim Sulaymonovich2
1A Leading Multi-Specialty Clinic Addu City, Republic of Maldives
2Bukhara State Medical Institute named after Abu Ali Ibn Sino
Correspondence to: Shekhovtsov Stanislav Alexandrovich, A Leading Multi-Specialty Clinic Addu City, Republic of Maldives.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article presents an analysis of factors that have the potential to influence the results of laser ablation of short, complex rectal fistulas using the FiLAC technique. A statistical analysis of the significance of these factors was carried out. The analysis carried out during the study, including the assessment of the Odds Relationship, showed that such parameters as: gender, history of the disease, anatomy of the location of the fistula, the diameter of the internal opening of the fistula, the presence of concomitant pathology did not demonstrate a statistically significant effect on the risk of recurrent fistula in patients with short fistulous course in both groups. However, the use of more powerful laser radiation against the background of prolonged exposure to the walls of the fistula leads to a significant improvement in the results of treatment of patients with complex short fistulas.
Keywords: Short rectal fistulas, Complex rectal fistulas, Laser obliteration of rectal fistulas, FiLAC technique
Cite this paper: Shekhovtsov Stanislav Alexandrovich, Davlatov Salim Sulaymonovich, Analysis of Factors Influencing the Results of the Laser Obliteration Technique of Short and Complex Rectal Fistulas, American Journal of Medicine and Medical Sciences, Vol. 13 No. 7, 2023, pp. 913-916. doi: 10.5923/j.ajmms.20231307.15.
1. Introduction
- Despite the centuries that have passed since the first mention of rectal fistulas, the problem of their treatment continues to be relevant. In the last decade, there has been a breakdown in the paradigm of treatment of this pathology. Radical methods, but fraught with a high risk of anal incontinence, are replaced by minimally invasive and, most importantly, sphincter-preserving methods of treating rectal fistulas. Moreover, this direction continues to develop intensively. LIFT, Plug, and VAAFT procedures, which were considered very modern 10 or 20 years ago, fade into the background compared to such techniques as: Over the scope clip (using a special endoscopic nitinol clip with shape memory), FiLAC (elimination of fistulas using a laser) [1,3,7,12,16,17,19].One of the promising sphincter-preserving techniques is laser obliteration of the fistula by the FiLAC method. Despite the already achieved, encouraging results of the use of this technique and its gaining momentum in a wide proctological practice, many aspects related to the use of this technique continue to be poorly studied or not studied at all. Thus, a systematic review of international literature to identify factors that may influence the results of the use of FiLAC technology showed that no more than 2 dozen papers were devoted to this topic. At the same time, they demonstrate very contradictory indicators on a number of studied aspects. For example, only 6 publications were found devoted to the problem of the influence of the anatomical location of the fistula passage in relation to the anal sphincter on the frequency of healing of fistulas after the application of the FiLAC technique. Analysis of the effect of the length of the fistula canal on the healing results also shows contradictory results. Giamundo P. (2015) in his work noted that the best result is achieved with long, more than 4 cm long fistulas [10,11]. On the contrary, Ozturk E. (2014) recorded healing of the fistula in 82% of cases with a length of the fistula not exceeding 4.5 cm [18]. An important point should be noted. In all the publications studied, the use of a diode laser with a wavelength of 1470 nm was noted. and power from 12 to 13 watts. Only in the work of Marref I. et al. (2019) the use of laser radiation of various power (from 12 to 15 watts) was noted.The purpose of the study: To improve the quality of treatment of patients with short and complex rectal fistulas.
2. Materials and Methods of Research
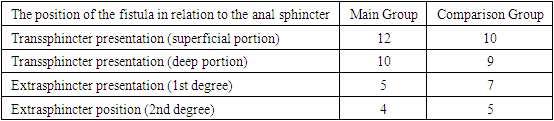
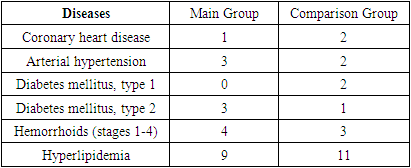
- Taking into account the current situation, in order to identify factors that may influence the results of using the FiLAC technique, we carried out a randomized, single-center, comparative clinical trial in which an assessment of the odds ratio (OR) was used depending on the presence or absence of various components. In total, 8 factors were analyzed: the gender of patients, the duration of the course of the disease, the anatomy of the location of the fistula, the diameter of the internal opening of the fistula, the occurrence of relapse of the disease, the occurrence of postoperative complications, the healing time of the surgical wound, the presence of concomitant pathology. The study was performed on 62 patients with transsphincteric and extrasphincteric fistulas of the rectum using the Cherylas-15N device (manufacturer Wuhan Dimed Laser Technology Co., Ltd., China) and the Lightguide SA600 light guide with radial energy radiation of the same manufacturer. The data on these patients were divided into two equivalent groups. The first group is the main group (MG). In it, laser obliteration of the fistula was performed using a diode laser with a wavelength of 1470 nm. and a power of 14 watts. The extraction speed of the light guide at the same time was 1 mm / 3 seconds. The second group is the comparison group (CG). In it, laser obliteration of the fistula was performed according to the classical technique using a diode laser with a power of 12 watts and a wavelength of 1470 nm. The extraction speed of the light guide at the same time was 1 mm / 1 second. In both groups, the length of the fistula did not exceed 4 centimeters.The patients included in the study were selected on the following principles:• age over 18;• patients with transsphincteric fistulas;• patients with extrasphincteric fistulas of 1-2 degrees of complexity;• the presence of a fistula passage not exceeding 4 centimeters in length;• patients with primary and recurrent fistulas;• absence of additional fistula passages and congestion;• absence of rough deformation of the mucosa in the area of the internal opening of the fistula;• the width of the inner opening of the fistula passage not exceeding 5 mm;As a result, 31 patients were included in both groups who fully met the criteria described above.The results of the study. The analysis of the obtained materials showed the following results. In the Main Group, healing occurred in 23 (74.1%) of 31 patients. In the Comparison Group, healing occurred in 19 (61.2%) patients out of 31. Analyzing the results of the use of different laser radiation power and the duration of its effect on the walls of the fistula in both groups, we obtained an OR (Odds Ratio) equal to 1.211 (greater than 1), which suggests that the use of laser radiation power equal to 14 watts and the extraction speed of the fiber equal to 1 mm \ 3 sec has a positive effect on the result treatment, increasing the probability of healing by 12.1 times.The effect of the gender of patients on the frequency of healing showed the following results. Both groups turned out to be equivalent in terms of the sexual composition of patients. The Main Group included 21 (67%) men and 10 (33%) women. The Comparison Group included 19 (61%) men and 12 (39%) women. When comparing the effect of the sex of patients in both groups of men, we obtained an OR (Odds Ratio) equal to 0.436 (less than 1) in men and 0.870 (less than 1) in women, which suggests that the influence of the gender of patients does not significantly affect the results of treatment.Analysis of the duration of the disease showed the following. In the Main Group, in 5 patients, the duration of the disease did not exceed 6 months, in 10 patients - 12 months, in 12 patients - 24 months, in 4 patients, the duration of the disease exceeded 24 months, with an average duration of the disease equal to 20 (1-48) months. In the Comparison Group, in 8 patients, the duration of the disease did not exceed 6 months, in 11 patients - 12 months, in 5 patients - 24 months, in 4 patients, the duration of the disease exceeded 24 months, with an average duration of the disease equal to 22 (1-56) months. In both groups, we received an OR (Odds Ratio) equal to 0.767 (less than 1), which indicates that the influence of anamnesis lasting up to 1 year does not significantly affect the results of treatment. When comparing the effect of the anamnesis of patients lasting more than 1 year, in both groups we obtained an OR (Odds Ratio) equal to 0.592 (less than 1), which suggests that the effect of anamnesis lasting more than 1 year also does not significantly affect the results of treatment.The study of the location of the fistula revealed the following. In 19 (61%) patients from the Comparison Group, a transsphincteric fistula passed through a superficial or deep portion of the external sphincter. 12 (39%) patients of the same group had an extrasphincteric fistula of 1-2 degrees of complexity. In The Main Group transsphincteric fistula passing through the superficial or deep portion of the external sphincter was detected in 22 (70%) patients. Extrasphincteric fistula of 1-2 degrees of complexity was detected in 9 (30%) patients from the same group (Table 1).
|
|
3. Conclusions
- The analysis carried out during the study, including the assessment of the Odds Ratio, showed that such parameters as: gender, anamnesis of the disease, anatomy of the location of the fistula, the diameter of the internal opening of the fistula, the presence of concomitant pathology did not demonstrate a statistically significant effect on the risk of recurrence of the fistula in patients with a "short" fistula in both groups. On the contrary, such parameters as: the occurrence of postoperative complications and the frequency of healing showed statistically significantly better results in the case of applying the technique using a radiation power of 14 watts and a light guide extraction speed of 1 mm \ 3 sec. That is, our study showed the absence of any prognostic factors affecting the frequency of healing of complex "short" fistulas. However, the use of more powerful laser radiation against the background of prolonged exposure to the walls of the fistula leads to a significant improvement in the results of treatment of patients with complex "short" fistulas.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML