-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(7): 907-909
doi:10.5923/j.ajmms.20231307.13
Received: Apr. 26, 2023; Accepted: Jun. 22, 2023; Published: Jul. 12, 2023

Clinical Picture of Trophic Ulcers of the Oral Cavity in Patients Suffered COVID-19
Inoyatov A. Sh., Saidova M. A.
Department of Hospital Therapeutic Stomatology, Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Saidova M. A., Department of Hospital Therapeutic Stomatology, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

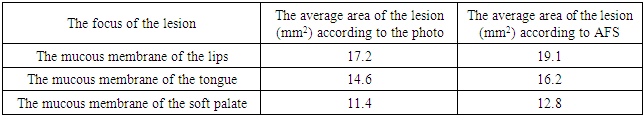
The problem of care for patients with trophic ulcers remains an urgent medical and social problem, which has again aggravated against the backdrop of the COVID-19 pandemic in 2020–2021. As is now known, after a viral infection with COVID-19, most patients with cardiovascular diseases experience a significant exacerbation of these ailments. In many patients after pneumonia associated with COVID-19, the formation of trophic ulcers of the oral mucosa was noted. There were 104 patients with a trophic ulcer of the oral cavity and 21 patients without history of oral mucosal disease, who were included in the control group, examined. Clinical methods, photoplanimetry, and autofluorescent stomatoscopy of the oral mucosa were used in research. In order to characterize the size of the trophic ulcer of the oral mucosa, it is necessary to use the autofluorescent stomatoscopy due to the fact that this research method has the advantage of more accurate determination.
Keywords: COVID-19, Trophic ulcers, Oral mucosa
Cite this paper: Inoyatov A. Sh., Saidova M. A., Clinical Picture of Trophic Ulcers of the Oral Cavity in Patients Suffered COVID-19, American Journal of Medicine and Medical Sciences, Vol. 13 No. 7, 2023, pp. 907-909. doi: 10.5923/j.ajmms.20231307.13.
Article Outline
1. Relevance
- The problem of care for patients with trophic venous ulcers remains an urgent medical and social problem, which has again aggravated against the backdrop of the COVID-19 pandemic in 2020–2021 [1]. As is now known, after a viral infection with COVID-19, most patients with cardiovascular diseases experience a significant exacerbation of these ailments. In many patients after pneumonia associated with COVID-19, the formation of trophic ulcers of the oral mucosa is noted. At the same time, trophic ulcers are highly resistant to traditional therapy (surgery) aimed at their healing [2-3].Virtually every second patient (48%) came to us with the appearance of ulcers on the buccal mucosa. Among other symptoms the patients also presented with pain or discomfort on talking, chewing [4-5].The responsibility of the dentist is to timely diagnose oral manifestations in patients who have had a coronavirus infection and choose the most adapted algorithm for their treatment, excluding surgery, depending on the clinical manifestations in the oral cavity. Now, the issue of conducting a thorough examination and prescribing therapeutic and preventive measures also remains open, to prevent the development of a trophic ulcer of the oral mucosa and its complications [6-9]. Even an asymptomatic course of COVID-19 can leave long-term adverse effects in the form of a weakened immune system or a tendency to autoimmune processes, including in the oral cavity.
2. The Purpose of the Study
- Assessment of the features of the clinical course and diagnosis of trophic ulcers of the oral mucosa in patients who have undergone COVID-19.
3. Materials and Methods
- Scientific research work was carried out by at the Department of Hospital Therapeutic Dentistry of Tashkent State Dental Institute (Uzbekistan) in the period for 2021-2023.A total of 125 patients were screened for dental treatment at the institute. There were 104 patients with a trophic ulcer of the oral cavity and 21 patients had no history of oral mucosal disease, who were included in the control group. The study involved 61 men and 43 women. The study included people aged 18-70 years. The average age of the subjects was 56.7±0.9 years. The study participants were divided according to the following criteria: group 1 (main) - patients with trophic oral ulcers with somatic pathology, as diabetes or cardiovascular diseases (52 patients), group 2 (comparisons) - patients with trophic oral ulcers without somatic diseases (52 patients), group 3 (control) - patients without disease of oral mucosa (21 people). All study participants were consulted with a general practitioner, cardiologist, endocrinologist, virologist and phlebologist. No severe somatic pathology was detected in patients of all groups.To solve the set tasks and achieve the goal of the study, clinical methods, photoplanimetry and autofluorescent stomatoscopy of the oral mucosa were used in the work.
4. Results and Discussion
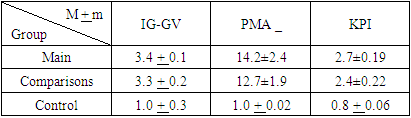
- 125 patients were examined. There were 104patients with a trophic ulcer of the oral cavity and 21patients had no history of oral mucosal disease, who were included in the control group. The study involved 61 men and 43 women. The study included people aged 18-70 years. The average age of the subjects was 56.7±0.9 years. The study participants were divided according to the following criteria: group 1 (main) - patients with trophic oral ulcers with somatic pathology (52 patients), group 2 (comparisons) - patients with trophic oral ulcers without somatic diseases (52 patients), group 3 (control) - patients with a sanitized oral cavity, who are not sick (21 people). All study participants were consulted with a general practitioner, cardiologist, endocrinologist, virologist and phlebologist. No severe somatic pathology was detected in patients of all groups.Age ratios in group 1 were: patients aged 18-39 years 51.5%, aged 40-60 years 48.5%. In group 2 patients aged 18-39 years were 67.2%, aged 40-60 - 42.8%. In group 3 patients aged 18-39 years were 60%, and aged 40-60 - 40%. The total number of patients studied, aged 18-39 years was 56.2%, and aged 40-60 years - 43.8%.Upon admission to the Department of Therapeutic Dentistry of the Tashkent State Dental Institute, most patients presented with a chief complaint of a defect in the oral mucosa in the form of an ulcer (74.8%), pain (47.1%), burning sensation in the oral cavity (13.8%), dryness in the mouth (28.32%), bad breath (42.7%), bad taste or taste disturbance (28.6%) in the main group.While the patients of the comparison group, there were similar, but not significantly different in the number of complaints. So, the presence of a defect in the oral mucosa in the form of an ulcer complained (78.3%) of the patient, pain (11.8%), burning in the mouth (5.4%), dry mouth (32.1%), bad breath (32.1%), unpleasant taste or taste disturbance (28.5%) Patients of the comparison group, who did not have an aggravating background pathology, rarely noted soreness and burning of the oral mucosa, the severity of the pain syndrome was several times lower compared to that in the main group.We analyzed the history data of the main group. All study participants were consulted by a general physician, cardiologist, virologist, and phlebologist.Thus, patients suffered from chronic cardiovascular insufficiency (42.8%), diabetes mellitus (31.6%), polyneuropathy (2.4%), vasculitis (3.2%), rheumatoid arthritis (6.7%), deep venous thrombosis (13.3%). All the above diseases in themselves are risk factors for the development of a trophic ulcer of the oral mucosa. However, in our cases, all patients indicated a past coronavirus infection as the cause of the development of an ulcer. Perhaps the psychological factor played, since at the moment of the development of civilization the entire world community is busy thinking about Covid -19, and with somatics, patients are simply “used to live together”.Regarding the comparison group, it should be noted that in the absence of somatic pathology, the development of a trophic ulcer indicates severe systemic disorders and, possibly, even diseases that have developed under the influence of Covid -19 on the body.The index assessment of the state of the oral cavity gave evidence of an unsatisfactory hygienic state of the oral cavity and the presence of inflammation of the periodontal tissues in both study groups.The hygienic status of the oral cavity was determined by the Green-Vermillion method and gave indicators of the unsatisfactory hygienic state of the oral cavity of the subjects in both groups (Table 1).
|
|
5. Conclusions
- Complex treatment of children with HSV was more effective, as evidenced by the results of the 3rd group. When using PDU, traditional therapy and a biologically active food supplement based on a lipid concentrate from the biomass of snakes of the ERYX genus - Reptin-plant (made in Uzbekistan), patients of the 3rd group observed earlier disappearance of symptoms of HVI intoxication and pain in the oral mucosa, enhanced result of complete epitilization, a decrease in the frequency and severity of relapses, as well as an increase in the duration of remission.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML