-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(6): 769-771
doi:10.5923/j.ajmms.20231306.01
Received: May 16, 2023; Accepted: May 30, 2023; Published: Jun. 2, 2023

Study of Long-Term Results of Myocardial Revascularization in Patients with Сoronary Artery Disease with Damage to the Trunk of the Left Coronary Artery
Kakharov I. I., Fozilov Kh. G.
Republican Specialized Scientific-Practical Medical Center of Cardiology, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the research: to study of long-term results of myocardial revascularization in patients with various forms of coronary artery disease with damage to the trunk of the left coronary artery. 149 patients with сoronary artery disease (CAD) were examined. According to the analysis of the clinical forms of the disease in patients with CAD, chronic coronary syndromes were detected in 75 (50.3%) patients and 74 (49.7) patients acute coronary syndromes (ACS). An analysis of the dependence of the development of PMI on various factors showed that recurrent MI develops significantly more often with an EF<40%. The prognostic indicators of long-term mortality and com-plications was showed out for risk factors for the progression of atherosclerosis of the coronary arteries as diabetes, lack of therapy for hypercholesterolemia (statins, fibrates, etc.), arterial hypertension (AH), aggravated heredity for coronary artery disease and continued smoking by patients after surgery.
Keywords: Left coronary artery, Endovascular interventions, Long-term results
Cite this paper: Kakharov I. I., Fozilov Kh. G., Study of Long-Term Results of Myocardial Revascularization in Patients with Сoronary Artery Disease with Damage to the Trunk of the Left Coronary Artery, American Journal of Medicine and Medical Sciences, Vol. 13 No. 6, 2023, pp. 769-771. doi: 10.5923/j.ajmms.20231306.01.
1. Introduction
- The trunk of the left coronary artery (LCA) is the proximal segment of the left coronary artery, departs from the left aortic sinus and continues until the bifurcation division into the anterior interventricular branch and the circumflex branch of the LCA. In some cases, a trifurcation division of the LCA trunk is determined, which also includes an intermediate branch of the left coronary artery. The length of the LCA trunk varies greatly, but it is usually short and rarely exceeds 1.0 cm [1]. Due to the anatomical features, patients with lesions of the LCA trunk are one of the most severe groups of patients with coronary artery disease (CAD), which are characterized by a high risk of death, frequent development of left ventricular dysfunction and life-threatening arrhythmias [2,3]. With a bifurcation lesion of the LCA trunk, in the vast majority of cases, the atherosclerotic lesion passes from the side walls of the LCA trunk to the anterior interventricular branch and the circumflex branch of the left coronary artery. Part of the artery at the site of blood flow separation remains intact [4]. Such localization of an atherosclerotic plaque in a bifurcation lesion often explains the possibility of successful stenting of the LCA trunk using one stent, followed by inflation with two balloons. A feature of the LCA trunk is the presence of a large number of elastic fibers in the wall, which determines the frequent occurrence of re-narrowing in this area and the development of restenosis after balloon angioplasty [5,6]. Patients with LCA disease, left main artery equivalent, and three-vessel CAD represent an overlapping spectrum of patients with progressive CAD that is associated with poor prognosis. Medical therapy as recommended is a necessary but often not sufficient treatment option, as these patients often require mechanical revascularization with coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI). In patients with advanced CAD secondary to acute myocardial infarction, PCI is clearly the preferred treatment option [7]. With the introduction of coronary stents into clinical practice, encouraging results of LCA stenting have appeared [8]. Good results in the treatment of patients with stable coronary artery disease can be achieved through a combination of drug therapy, coronary endovascular and surgical interventions. It is believed that the restoration of blood flow in the coronary artery during myocardial revascularization is the most modern approach in the treatment of patients with coronary artery disease with lesions of the LCA [9].The aim of the research: to study of long-term results of myocardial revascularization in patients with various forms of coronary artery disease with damage to the trunk of the left coronary artery.
2. Materials and Methods
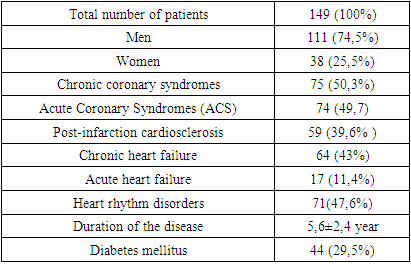
- 149 patients with CAD were examined. According to the analysis of the clinical forms of the disease in patients with CAD, chronic coronary syndromes were detected in 75 (50.3%) patients and 74 (49.7) patients - acute coronary syndromes (ACS). In history, 147 (98%) patients had AH, 59 (39.6%) patients had MI, 44 (29.5%) patients had diabetes mellitus, 64 (43%) patients had chronic heart failure (CHF) (Table 1). Various cardiac arrhythmias were observed in 71 (47.6%) patients.
|
3. Results
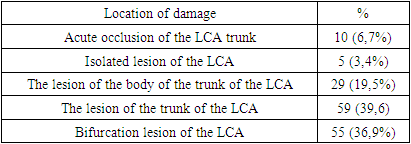
- The analysis of CAG data in patients with coronary artery disease, the degree of stenosis of the trunk of the left coronary artery was 75.3±5.2%. Acute occlusion of the left coronary artery was detected in 10 (6.7%) patients. An isolated lesion of the root of the left coronary artery was observed in 5 (3.4%) patients, a lesion of the trunk body in 29 (19.5%), an ostial lesion in 59 (39.6%) patients (Table 2). Bifurcation lesion of the root of the left coronary artery was observed in 55 (36.9%) patients, and often this condition was accompanied by lesions of other branches of this artery.
|
4. Discussion
- According to coronary angiography, lesions of the LCA trunk are observed in 4–8% of patients with coronary artery disease. Cases of isolated lesions of the LCA trunk in surgical groups of patients account for 1.5–13% [10]. Accordingly, in most cases, lesions of the LCA trunk are combined with lesions of other coronary arteries. Complete occlusion of the LCA trunk during selective coronary angiography is quite rare. Hemodynamic stenosis of the trunk of the LCA is one of the most severe variants of coronary disease. LCA trunk stenosis affects not only the patient's quality of life, but also reduces his life expectancy [11]. Often, the detection of stenosis of the LCA trunk during coronary angiography (CAG) is the only reason for refusing to perform stenting due to the high risk of developing severe complications and the likely subsequent referral of the patient for CABG. At the same time, LCA trunk stenting has ceased to be an exclusive operation and is performed both in Europe and the USA. In recent years, a number of studies have been carried out on the results of LCA stenting compared with CABG. The use of endovascular methods for lesions of the “unprotected” LCA trunk at the initial stage caused serious concern among doctors, however, due to the unsatisfactory results of the first studies in this area, their development did not stop. Currently, X-ray endovascular methods for lesions of the LCA trunk are widely used all over the world [12,13]. A number of studies have been carried out since the beginning of the stage of using antiproliferative coated stents. In the randomized study ISAR-LEFT MAIN (Intracoronary Stentingand Angiographic Results: Drug-Eluting Stents for Unprotected Coronary Left Main Lesions), the results of which were presented by comparing long-term results depending on the type of implanted stents [14].
5. Conclusions
- An analysis of the dependence of the development of PMI on various factors showed that recurrent MI develops significantly more often with an EF<40% and the statistical significance of this distribution is preserved both in the case of fatal and non-fatal MI. The prognostic indicators of long-term mortality and complications was showed out for risk factors for the progression of atherosclerosis of the coronary arteries as diabetes, lack of therapy for hypercholesterolemia (statins, fibrates, etc.), arterial hypertension (AH), aggravated heredity for coronary artery disease and continued smoking by patients after surgery.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML