Khakimov Murod Shavkatovich1, Matkuliev Utkirbek Ismailovich1, Batirov Davronbek Yusupovich2, Umarov Zafarbek Zaripboevich2
1Department of Faculty and Hospital Surgery of the Tashkent Medical Academy, Tashkent, Uzbekistan
2Department of Surgical Diseases and Transplantology of Urgench Branch of the Tashkent Medical Academy, Urgench, Uzbekistan
Correspondence to: Umarov Zafarbek Zaripboevich, Department of Surgical Diseases and Transplantology of Urgench Branch of the Tashkent Medical Academy, Urgench, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The most severe and often fatal complication of portal hypertension is esophageal-gastric bleeding from varicose veins of the esophagus and gastrous. When varicose veins are detected, massive bleeding occurs in 60% of patients. Despite the introduction of new technologies in the treatment of patients with portal hypertension, bleeding from varicose veins is accompanied by a mortality rate of more than 20% during the first 6 weeks after hemorrhage. Currently, medication, endoscopic, endovascular and surgical hemostasis are used to treat and prevent portal bleeding. The abundance of existing treatments indicates dissatisfaction with their results. So, with conservative treatment, mortality ranges from 30 - 51.2%, with surgical - 26 - 40.6%. To date, the world and our country have accumulated extensive experience in the use of minimally invasive endoscopic interventions for the treatment of esophageal varicose veins. However, the role of endoscopic methods of treatment in the prevention of variceal bleeding is assessed ambiguously. On the one hand, endoscopic ligation helps to reduce the frequency of bleeding from varicose veins. On the other hand, endoscopic interventions in 8.3%-19.6% can be complicated by bleeding and in more than 3.8% lead to death.
Keywords:
Liver cirrhosis, Portal hypertension, Varicose veins, Prevention, Endoscopic, Endovascular
Cite this paper: Khakimov Murod Shavkatovich, Matkuliev Utkirbek Ismailovich, Batirov Davronbek Yusupovich, Umarov Zafarbek Zaripboevich, Modern Treatment and Prevention of Bleeding from Esophagus and Gastrous Varicose Veins with Portal Hypertension (Review of Literature), American Journal of Medicine and Medical Sciences, Vol. 13 No. 5, 2023, pp. 762-767. doi: 10.5923/j.ajmms.20231305.46.
1. Introduction
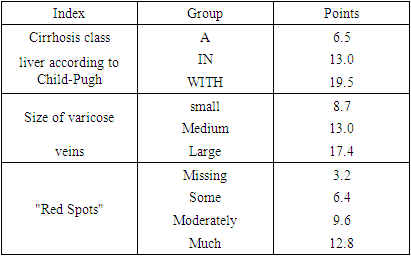
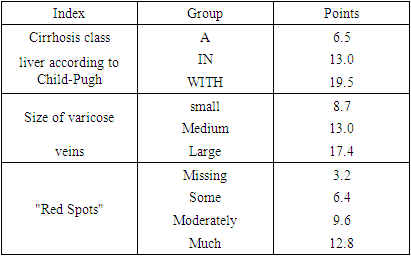
The most severe and often fatal complication of portal hypertension is esophagogastric bleeding (EGB) from varicose veins (VV) of the esophagus and gastrous (VVEG). When VRV is detected, massive bleeding occurs in 60% of patients [1,5,8]. Despite the introduction of new technologies in the treatment of patients with portal hypertension (PH), bleeding from VV is accompanied by a mortality rate of more than 20% during the first 6 weeks after hemorrhage [6].Currently, medication, endoscopic, endovascular and surgical hemostasis are used to treat and prevent portal bleeding. The abundance of existing treatments indicates dissatisfaction with their results. So, with conservative treatment, mortality ranges from 30–51.2%, with surgical treatment - 26–40.6% [2,9,11]. To date, the world and our country have accumulated extensive experience in the use of minimally invasive endoscopic interventions for the treatment of esophageal varicose veins. However, the role of endoscopic methods of treatment in the prevention of variceal bleeding is assessed ambiguously. On the one hand, endoscopic ligation helps to reduce the frequency of bleeding from varicose veins [13]. On the other hand, endoscopic interventions in 8.3%-19.6% can be complicated by bleeding and in more than 3.8% lead to death [12].The high mortality rate in the first episode of bleeding from VVEG determines the importance of developing clear criteria for the risk of bleeding, which would make it possible to determine the indications for primary prevention, the choice of prevention method and the timing of its implementation.In his observation Arun J Sanyal (2013) noted that patients at increased risk of variceal bleeding (patients with Child-Pugh class B or C cirrhosis, large varicose veins, and/or red marks on the esophageal RV) need primary prevention. In addition, primary prophylaxis may also be considered for patients with VV without the threat of bleeding [3,4,9,19].Varicose veins with a “high risk” of bleeding need preventive measures. Threatened by bleeding are considered medium or large veins with the presence of red marks. A generally accepted statement is that varicose veins larger than 5 mm are threatening to cause bleeding [11,13]. However, the proportion of patients with small varicose veins at risk of bleeding with red marks does not fall within this definition. In the Arun study J Sanyal (2013) data were limited on the effectiveness of prevention in certain categories of patients. From this, the author concludes that further research is needed to determine their genesis and the need for therapeutic interventions [5].The algorithm for assessing the prognosis of bleeding risk based on the index proposed by the North Italian Endoscopic Club seems to be interesting (Table 1).Table 1. Index values proposed by the North Italian Endoscopy Club (NIEC)
 |
| |
|
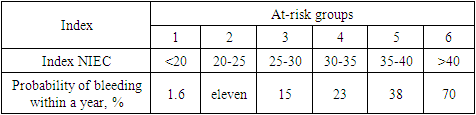
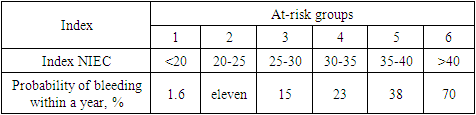
This algorithm takes into account the size of the VV, the presence of signs of vasculopathy, as well as the class of cirrhotic transformation of the liver, on the basis of which the NIEC index is calculated. The scores are summed up for all three indicators (Child-Pugh cirrhosis class, varicose vein size, red spots) on the basis of which the NIEC index is obtained. This index makes it possible to assess the risk of bleeding during the year (Table 2).Table 2. The risk of bleeding depending on the value of the index NIEC within 1 year
 |
| |
|
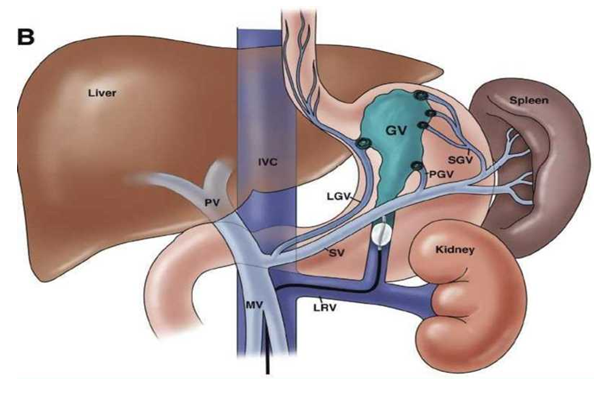
It is noteworthy that the most significant factor predetermining bleeding is the decompensation of the underlying disease - cirrhosis of the liver (Child-Pugh class C).The superficial location of VVs, their relationship with blood-filled intraepithelial elements of vasculopathy, as well as inflammatory changes in the mucous membranes of the esophagus and gastrous play a significant role in the rupture of varicose veins.Based on endoscopic findings Garbuzenko D.V. (2004) calculated a prognostic index (PI) that allows predicting the risk of bleeding, which includes three independent indicators: the degree of esophageal (A) and gastrous (B) RVV, the severity of gastropathy (C):PI = (A x 0.0395) + (B x 0.705) + (C x 0.878).According to the author, with index values less than 2.56, the probability of bleeding from VV is 0-20% during the first year of observation. If it exceeds 4.51, then the risk of bleeding increases to 81-100%.In addition to visual assessment of changes in the mucous membrane of the esophagus and gastrous, an indicator of the risk of variceal bleeding is the expansion of paraesophageal and paragastric veins of more than 5 mm, detected by endoscopic ultrasonography.Another equally important factor in the prognosis of bleeding is an increase in the hepatic pressure gradient above 12 mm Hg. Art., which largely depends on the stage of cirrhosis of the liver. On the other hand, the value of this indicator cannot be considered statically. So, in patients with portal hypertension, diurnal fluctuations in the port-hepatic gradient were noted: a decrease from noon to evening with minimal values by 19:00 and a gradual rise during the night, reaching the initial level by 9:00. Also, an increase in the pressure gradient was recorded after a meal, ethanol, with an increase in intra-abdominal pressure, for example, due to ascites [4,7,9,12].Obviously, in patients at high risk of developing variceal bleeding, even small changes in portal pressure can be clinically significant. However, pressure gradient measurement has limitations of use - invasiveness and impossibility of wide access, and therefore, its regular use in clinical practice cannot be recommended. In this connection, we need a safe and accurate atraumatic method for measuring portal pressure. Until this goal is achieved, pressure gradient measurement remains the only way to assess response to pharmacological therapy and develop an individualized approach to prevent variceal bleeding in patients with portal hypertension. Measurement of the pressure gradient is recommended to identify patients at high risk of VV bleeding and patients not responding to medical treatment [3,5,8,13].In recent years, Doppler ultrasonography has been introduced into research and medical practice, thanks to which it has become possible to measure blood flow in the vessels of internal organs. It has been established that the congestion index (congestion ingex) (CI) of the portal vein system correlates with the magnitude of the portohepatic pressure gradient and may serve as an independent risk factor for variceal bleeding [8].The stagnation index is calculated by the formula:CI = See / Vср. вв,where S BB is the cross-sectional area of the portal vein, V cp. cc - the average linear velocity of blood flow in the portal vein.In his works Koshevoy A.P. et al (2012) based on accurate measurement of vein and mucosal wall thickness by endosonography to determine the risk of bleeding from esophageal varices. The risk of gastric bleeding was assessed by studying the diameter of the vein.According to many authors, the predictors of a high risk of bleeding from the gastric varices are the diameter of the varicose veins of the gastrous up to 5 mm or more, class B or C according to Child-Pugh and the presence of red marks [3,5,7,19].In patients with extrahepatic portal hypertension, decompensation of the functional state of the liver cannot serve as a prognostic factor for bleeding. Most of the patients in this group did not have any hepatic dysfunction. In his research, Fandeev E.E. (2014) outlined the factors associated with an increased risk of bleeding in patients with HSV, the etiological factor being congenital or acquired thrombophilia. According to the author, the most significant prognostic criteria are: varicose veins of the esophagus and gastrous of the 3rd degree (corresponding to an increase in the risk of hemorrhage by 5.05 and 5.77 times, respectively), the presence of vasculopathy and inflammatory changes in the mucosa (increased risk by 5.24 and 2.85 times, respectively), the spread of VV of the gastrous beyond the cardia to the body and fundus of the gastrous (4.21 times). Also, a connection was established between total thrombosis of the vessels of the portal system and an increase in the risk of EGB by 2.41 times [3,8].For a long time, the concept of prevention did not exist at all. For a long time, the clinic was engaged in the treatment of bleeding and secondary prevention of bleeding.Two methods of esophagus VV endoscopic sclerotherapy (ES) have been described: intravasal and paravasal. With intravasal administration of a sclerosant (which is injected into the lumen of a vein), an intravascular thrombus is formed due to the inflammatory reaction of the intima of the vein and the development of connective tissue at the site of the thrombosed varicose vein. With the paravasal ES method (in which the sclerosant is injected into the submucosal layer), aseptic inflammation develops, and then connective tissue forms in the paravasal tissue, followed by the involvement of the vein wall in the cicatricial process [2]. The paravasal ES method has proven itself due to a lower complication rate in contrast to the intravasal one [2,4,5,8].In recent years, most authors have almost abandoned intravasal thrombosis, since the technique has serious drawbacks in the form of a significant number of severe complications, such as purulent and necrotic thrombophlebitis, esophageal perforation, mediastinitis [2]. It was also noted that the cause of about 50% of bleeding in the immediate period after ES is ulceration of the mucous membrane of the esophagus and gastrous. Unlike peptic ulcers of the esophagus, which are most often limited to the mucous membrane, after sclerotherapy, the process often extends to all layers of the esophageal wall [2].Initially, sclerotherapy was used only for medicinal purposes, and now ES has no place in primary prevention, due to a large number of complications and high mortality.In the mid-1990s, a method was developed for the treatment of VVEG - endoscopic ligation (EL) of VV with latex rings (Fig. 1) [5]. | Figure 1. Ligator for ligation of VV of the esophagus |
Simultaneously with the advent of the multi-charge device with latex rings, EL VVEG was performed for the first time in Japan with a sliding nylon loop. The use of the EL method in the practice of surgeons both in Russia and abroad made it possible to increase the efficiency of stopping ongoing bleeding from the esophageal VVEG to 90-96% and reduce the frequency of rebleeding to 12-36%. In literature there is evidence of positive results of the use of EL to prevent recurrence of portal bleeding [2,9,12,16].The goal of EL is to eradicate varicose veins. Based on international standards and Baveno consensus resolutions I and Baveno III, eradication of VV is achieved with an endoscopic picture, which is characterized by the disappearance of varicose veins (F0) or their reduction to longitudinally limited white bands with a diameter of less than 3-5 mm (F1).The American Association for the Study of Liver Diseases (AASLD) published guidelines in 2007 on primary prevention of variceal bleeding [6,9], and in 2010 the Baveno consensus recommendations were published. V [6,12,15].AASLD Recommendations similar to Baveno recommendations. Both communities recommend non-selective β-blocker prophylaxis in patients with compensated cirrhosis and small varices who have not previously bled but meet criteria for increased risk of bleeding (grade B). or C cirrhosis of the liver according to Child-Pugh or the presence of red marks). In addition, the guidelines state that non-selective β-blockers may be considered for patients with cirrhosis and small varices who do not have a history of bleeding and do not have any criteria for increased risk of bleeding. Finally, AASLD and Baveno recommend prophylaxis with non-selective β-blockers or EL for patients with moderate to large VV.According to a literature review, patients with small varicose veins without evidence of bleeding threat (red markers) or Child-Pugh C cirrhosis may be considered candidates for treatment with non-selective β-blockers, but further studies are needed to confirm the benefit of this approach.Arun J Sanyal et al (2013) provide primary prophylaxis for patients with moderate or large VV or non-selective blockers or EL. The choice of a non-selective β-blocker or EL depends on the patient's tolerance to non-selective β-blockers, and whether the patient is willing to accept the risks of EL and undergo the many necessary endoscopic procedures. Since some evidence suggests that EL may be more effective than β-blockers in patients with large VVs, it is the author's preference to treat such patients with EL whenever possible [19]. It is also important to note that β-blockers reduce cardiac output in cirrhosis, which is an important predictor of hepatorenal syndrome. The author believes that a possible explanation for the increased mortality in patients treated with β-blockers is that β-blockers may precipitate the onset of hepatorenal syndrome.Andrew K. Burroughs (2010) recommends non-selective β-blockers as first-line therapy for the primary prevention of bleeding in patients with cirrhosis, while endoscopic ligation does not sufficiently reduce the risk of bleeding. However, β-blockers, according to the author, have many contraindications and can cause various side effects such as dizziness, drowsiness, fatigue, nausea, diarrhea, sleep disturbance, pain in the legs, visual disturbances, blue fingers and toes, numbness / swelling of the hands. and legs, decreased libido, irreversible hair loss, mood changes, joint damage, butterfly rash on the face, difficulty breathing, cough, unexplained weight gain, thirst, increased urine output. In patients who have contraindications or intolerance to non-selective β-blockers, EL should be, according to Andrew K. Burroughs, the method of choice [5,9]. The combination of non-selective β-blockers with vasodilators or with EL in the author's works did not show any advantages in the primary prevention of bleeding from VV. In this connection, their combination is not appropriate.Andrew K. Burroughs believes that statins and renin-angiotensin-aldosterone inhibitors are promising for the treatment of portal hypertension, but randomized controlled trials of their effectiveness should be conducted [5,9].Nitroglycerin preparations effectively reduce portal pressure in patients with cirrhosis due to peripheral vasodilation. The drugs cause vasodilation by acting as NO donors. The use of sublingual nitroglycerin in patients with cirrhosis showed a decrease in the portosystemic pressure gradient after 2-12 minutes. Nitrates mainly reduce the tone of the venules, which leads to an increase in the capacity of the venous bed and a decrease in the portal pressure gradient, on average, by 30%. However, most researchers [5,9,13,14] currently do not recommend the use of drugs of this group for the primary prevention of bleeding from VV, due to the lack of a significantly significant clinical result. It is still unclear whether nitrates can reduce the risk of first bleeding.Christos Triantos and co-authors (2014) define the basic requirements for drugs used for preventive treatment. The drugs of this group should have a small number of side effects, an easy way to use and low cost. EL is invasive and can lead to fatal iatrogenic bleeding as well as increased medical costs. There is a need for specialized personnel and lengthening of the bed-day. In connection with this economic aspect, the author believes that non-selective β-blockers should be the method of choice in primary prevention. EL should be considered in patients with contraindications to non-selective β-blockers or who are not responding to therapy.In his observation, Bakulin I.G., (2014) noted that in case of varicose veins of the esophagus of III and IV degrees (according to the classification of K. J. Paquet ), in addition to conservative therapy with non-selective β-blockers and / or carvedilol, endoscopic therapy is indicated (mainly endoscopic ligation of the VV of the esophagus), and in some cases, transjugular intrahepatic shunting due to a high risk of bleeding [3,9,11].Shiv Kumar Sarin (2008) favors pharmacotherapy, in particular β- blockers. The author also compared groups of patients receiving EL and combination therapy (EL plus non-selective β-blockers). There were no differences in the incidence of bleeding or mortality between groups. Varicose veins recurred more frequently in the EL group, while side effects were more common in the combination therapy group. Thus, it can be concluded that there is no need for combination therapy (EL plus non-selective β-blockers).In his works, Filin A.A. (2011) noted a combined approach to the treatment of patients with VVEG, which included medical, endoscopic and surgical components. Numerous studies have shown that non-selective β-blockers (propranolol, nadolol, timolol, etc.) are effective. They are currently recommended as the drug of choice until first bleeding, with dosage adjustments to reduce portal pressure below 12 mm Hg. Art.According to Rayan Kochar (2010) there are no studies evaluating pharmacotherapy or endoscopic treatment for the primary prevention of gastric VV bleeding. Most of the recommendations relate to the treatment of esophageal VVs. According to the author, the predictors of bleeding from the VV of the gastrous are: the large size of varicose veins, the presence of red signs, Child -Pugh class C. Rajan Kochar indicates that these patients may be treated with non-selective β-blockers to prevent bleeding from varices.Separate analysis deserves surgical interventions, the use of which a number of authors call "operations of desperation", when medical and endoscopic measures do not give the desired effect. We are talking about azigo-portal uncoupling (APU) operations. It is advisable to divide this group of operations according to the degree of separation into partial ones (endoscopic sclerotherapy, X-ray endovascular embolization of the left gastric vein, transesophageal and transgastric suturing of the VV, dissection of the esophagus and devascularization operations) and total (gastrectomy, proximal resection of the gastrous and abdominal esophagus, Sugiura, Futagava, Hassab operations). The effectiveness and duration of the effect of these operations is directly proportional to the extent of separation and termination of the discharge of blood from the portal system into the esophageal venous plexus systems.Using APU operations in their practice, the authors note among the advantages of the operations of the first group the absence of impaired blood supply to the liver and, as a result, the prevention of aggravation of chronic liver failure in patients with liver cirrhosis. In addition, the advantages of some operations of this group include the simplicity of technical execution and acceptable long-term results, which contributes to the breadth of their application [2,6].In the historical aspect, some interventions of this kind deserve attention. J. Boerema, G. Crile, F.Burcharth, V. Rapant, R. Walker, R. Linton, D. Skinner - each of these surgeons offered his own version of the APU operation, but the general essence was reduced to dissection of the esophageal wall (longitudinal or transverse), with one or several incisions, followed by restoration, ligation or stitching of bleeding VVs, with separate threads or a continuous suture. Operation X.Tanner who used first thoracotomy for esophagotomy, and then a more sparing laparotomy access, modified by M.D. Patsiora [8]. This intervention involves gastrotomy followed by suturing of the veins of the gastrous near the cardiac opening, as well as the veins of the abdominal part of the esophagus at a distance of about 4-5 cm.The main cause of recurrence is the redirection of blood flow through VVs left unsutured, followed by their rupture [2,12]. Despite the quite acceptable long-term results of the use of such operations, it is palliative in nature. The possibility of bleeding recurrence in the postoperative period remains in almost 50% of patients [2]. The main disadvantages of uncoupling operations include the destruction of the cardiac sphincter. Subsequently, these patients develop reflux esophagitis, which can cause bleeding from the VVEG.In the world literature, the attitude to these types of operations is ambiguous. Thus, some surgeons [3,4,7,8] consider their use justified as a "despair operation", while others believe that operations on the esophagus and gastrous are the most effective of the existing methods of treating and preventing bleeding from esophageal and gastric varicose veins. It has long been well known that esophageal-gastric hemorrhages, as well as their recurrences, greatly exacerbate hepatic-renal failure in such patients and drastically worsen the prognosis [10]. The high mortality associated with this and other factors when using the above methods became the reason for the search for such a method of portal decompression, which could combine efficiency, namely, the achievement of the result in the form of an acceptable reduction in pressure in the IV system, residual to stop hemorrhage and prevent relapses of the esophageal bleeding, and tolerability of the intervention by patients with severe underlying pathology - cirrhosis.The idea of creating a transdermal transjugular porto-caval shunt (transjugular intrahepatic portosystemic shunt - TIPS) as a method of treating PH was proposed in 1969 by J. Rosch et al. [13]. First TIPS with balloon dilatation of the intrahepatic canal was used in 1982. R. colapinto et al, with stent - M. Rossle et al. in 1988 [4,5].With regard to the primary prevention of bleeding from VV of the gastrous according to Shiv Kumar Sarin EL, which is the gold standard for the treatment of bleeding and secondary prevention for esophageal varicose veins, has not justified itself as a primary prevention of bleeding from gastric varices. According to the author, the low efficiency of the method limits its ability to prevent the first bleeding. In this regard, an alternative procedure was proposed - balloon occlusive retrograde transvenous obliteration (B - RTO), which in 90% of cases was effective and safe in the obliteration of VV of the fundus of the gastrous (Fig. 2). B - RTO feasible only in the presence of a gastrorenal shunt. The latter is determined in 85% of patients with liver cirrhosis [9,18]. Complications B - RTO include transient fever, deterioration of liver biochemistry, hemoglobinuria, abdominal pain, pleural effusion, atrial fibrillation, risk of hepatic and renal failure, shock, and embolism due to the relatively large volume of sclerosant that is injected when performing a B - RTO [5].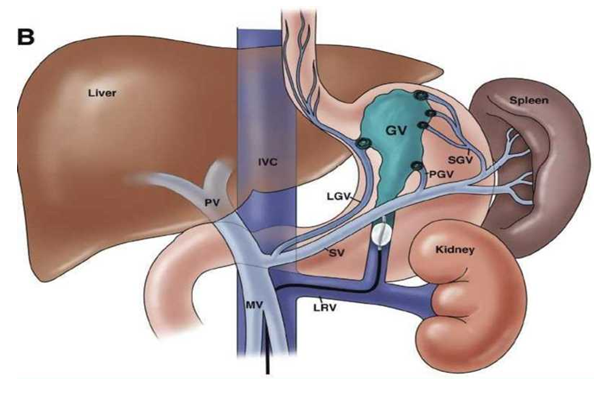 | Figure 2. Balloon retrograde transvenous obliteration (B - RTO) (J. C. Garcia - Pagan 2014) |
Randomized trial of Shiv Kumar Sarin (2008) of patients showed that balloon occlusive endoscopic injection sclerotherapy (BO - EIS) was as effective as B - RTO and requires less sclerosant compared to B - RTO and safer for the purpose of prophylactic treatment of varicose veins of the gastric fundus with the threat of bleeding [11,17]. BOEIS has the advantage of being applicable to patients with gastric varicose veins without a gastrorenal bypass.
2. Conclusions
1. Summarizing all of the above, most authors prefer pharmacotherapy. Most often, β-blockers are used for the purpose of primary prevention of bleeding from the esophageal varices. In case of ineffectiveness of drug therapy or contraindications to the appointment of β-blockers, vein EL is recommended.2. In domestic and foreign literature, there are practically no reports on the prevention of bleeding from gastric VV. Also, all recommendations are aimed at preventing bleeding in patients with cirrhosis of the liver. The question of the need for prevention and treatment of hepatic portal hypertension is not considered and remains open.3. Thus, despite the numerous studies carried out in this area, the question of treatment and prevention of bleeding from varicose veins of the esophagus and gastrous remains relevant and little studied to date.
References
| [1] | Akilov Kh.A., Devyatov A.V., Ibadov R.A., Ikramov A.I. The use of adhesive composition TachoComb in the formation of portosystemic anastomosis // Bulletin of Surgery. - 2001. - T. 160, No. 2. - pp. 87 - 90. |
| [2] | Akilov H.A. Khashimov Sh.Kh., Devyatov A.V. The role of individual factors in the pathogenesis of varicose veins of the esophagus and bleeding from them in patients with liver cirrhosis. // Annals of surgical hepatology. 1998. - Volume 3. - No. 3- - p, 130. |
| [3] | Granov A.M., Borisov A.E. Endovascular surgery of the liver. - L.: Medicine, 1986. – p.224. |
| [4] | Kadyrov R.N., Improvement of the endoscopic method of stopping bleeding from varicose veins of the esophagus - Abstract of the thesis. diss.... candidate of medical sciences. Tashkent 2010. – p.22. |
| [5] | Karimov Sh.I., Borovsky S.P., Rakhmanov S.U., Atakhanov D.A. The choice of access for performing transhepatic endovascular and endobiliary interventions // Surgery. - 2003. - No. 3. pp. 69 - 72. |
| [6] | Myznikov IV, Endoscopic ligation in the prevention of bleeding from esophageal varices in patients with liver cirrhosis and portal hypertension. dissertation abstract for the degree of candidate of medical sciences. specialty code 14.01.17 - surgery. 2012. |
| [7] | Nazyrov F.G., Akilov Kh.A., Ibadov R.A., Asabaev A.Sh., Zainutdinov U.I., Khafizov B.B. Some pathogenetic aspects of the development of liver failure and its prevention in patients with liver cirrhosis after portosystemic shunting. // Bulletin of Surgery. I.I. Grekov. 2002. -№1, -pp. 87-90. |
| [8] | Olevskaya E. R. Endosonographic measurement of pressure in the veins of the esophagus - a new technology for determining the risk of complications of portal hypertension. Perm Medical Journal. - 2013 (T. 30, No. 3. 2013 pp. 78-81). |
| [9] | Bátovský M. [Do we need endoscopic sclerotherapy of oesophageal varices or the last turn off the light]. Vnitr Lek. 2011 Dec; 57(12): 989-92. Slovak. PMID: 22277030. |
| [10] | Chen S, Li X, Wei B, Tong H, Zhang MG, Huang ZY, Cao JW, Tang CW. Recurrent variceal bleeding and shunt patency: prospective randomized controlled trial of transjugular intrahepatic portosystemic shunt alone or combined with coronary vein embolization. Radiology. 2013 Sep; 268(3): 900-6. doi: 10.1148/radiol.13120800. Epub 2013 May 8. PMID: 23657891. |
| [11] | Dell'Era A, Iannuzzi F, Fabris FM, Fontana P, Reati R, Grillo P, Aghemo A, deFranchis R, Primignani M. Impact of portal vein thrombosis on the efficacy of endoscopic variceal band ligation. Dig Liver Dis. 2014 Feb; 46(2): 152-6. PMID: 24084343. |
| [12] | El Atrache M, Abouljoud M, Sharma S, Abbass AA, Yoshida A, Kim D, Kazimi M, Moonka D, Brown K. Transjugular intrahepatic portosystemic shunt following liver transplantation: can outcomes be predicted? Clin Transplant. 2012 Jul-Aug; 26(4): 657-61. doi: 10.1111/j.1399-0012.2011.01594.x. Epub 2012 Feb 6. PMID: 22309034. |
| [13] | Kang KS, Yang HR, Ko JS, Seo JK. Long-term outcomes of endoscopic variceal ligation to prevent rebleeding in children with esophageal varices. J Korean Med Sci. 2013 Nov; 28(11): 1657-60. PMID: 24265531. |
| [14] | Batirov, DY; Allanazarov, AX; Raximov, AP; Simultan laparoskopik operatsiyalarni surunkali kamqonlik kuzatilgan bemorlarda o ‘tkazilish natijalarini yaxshilash,Gospodarka i Innowacje., 32,, 90-93, 2023. |
| [15] | Batirov, DY; Kh, Allanazarov A; Rakhimov, AP; Rojobov, RR;, Improving the results of simultaneous laparoscopic surgery in patients with chronic deficiency, european journal of modern medicine and practice, 3, 2, 43-45, 2023. |
| [16] | Shavkatovich, Xakimov Murod; Ismoilovich, Matkuliev Utkirbek; Zaripboyevich, Umarov Zafarbek; Portal gipertenziya asoratlarini oldini olish va davolashda kaminvazivli aralashuvlar kompleksining samaradorligi, Science and innovation, 1, Special Issue 2, 379-383, 2022, OOO «Science and innovation». |
| [17] | Matkuliev, Utkirbek Ismailovich; Umarov, Zafarbek Zaripboevich; Minimally invasive interventions in the prevention and treatment of bleeding in patients with portal hypertension, SCIENTIFIC REVIEWER SCIENTIFIC-ANALYTICAL JOURNAL, 10, 118, 47-50, 2020, © Infiniti LLC. |
| [18] | Matkuliev, U.I.; Batirov, D.Yu.; Umarov, Z.Z.; Allanazarov, A.Kh.; Rakhimov, A.P.; Kalandarov, M.B.; Portal hypertension va uning asoratlarini davolashda endoscopic hamda endovascular usullar, Scientific perspective Scientific and analytical journal, 3, 157, 60-62, 2023, © Infinity LLC. |
| [19] | Ismailovich, Maktkuliev Utkirbek; Yusupovich, Batirov Davronbek; Zaripbaevich, Umarov Zafarbek et all; Minimally Invasive Interventions in Portal Hypertension Complication with Esophageal and Gastric Varicose Veins, Scholastic: Journal of Natural and Medical Education, 2, 4, 274-279, 2023. |




 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML