-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(5): 730-734
doi:10.5923/j.ajmms.20231305.38
Received: May 13, 2023; Accepted: May 26, 2023; Published: May 27, 2023

Laboratory–Instrumental and Anthropometric Research Methods for Hypertension in Patients with Migraine
N. Kh. Fattakhov1, N. S. Mamasoliev2, Sh. B. Turgunboev3, A. R. Abdulkhakimov1, G. B. Tilyakhodjaeva1
1Fergana Medical Institute of Public Health, Fergana, Uzbekistan
2Andijan State Medical Institute, Andijan, Uzbekistan
3Fergana Branch of the Republican Scientific Center for Emergency Medical Care, Fergana, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article describes the use of laboratory–instrumental and anthropometric research methods for hypertension in patients with migraine. The features of this disease, which combines hypertension and migraine headaches, as well as approaches to its diagnosis and treatment, are considered. The main laboratory and instrumental methods used in the diagnosis of hypertension, such as electrocardiography, blood pressure measurement, echocardiography, computed tomography and magnetic resonance imaging, are described. Anthropometric methods are also considered to assess the degree of obesity, the level of physical activity and metabolic parameters in patients with hypertension and migraine. The authors of the article emphasize the importance of an integrated approach to the diagnosis and treatment of this disease, which should include not only drug therapy, but also correction of the patient's lifestyle and diet.
Keywords: Electrocardiography, Ischemia, Age, Cardiology, Hypertension, Thrombosis, Blood, Clotting, Age, Hemostasis, Hypertension
Cite this paper: N. Kh. Fattakhov, N. S. Mamasoliev, Sh. B. Turgunboev, A. R. Abdulkhakimov, G. B. Tilyakhodjaeva, Laboratory–Instrumental and Anthropometric Research Methods for Hypertension in Patients with Migraine, American Journal of Medicine and Medical Sciences, Vol. 13 No. 5, 2023, pp. 730-734. doi: 10.5923/j.ajmms.20231305.38.
1. Relevance
- In the organisms of all multicellular creatures with shelter or hemolymph, protective systems function to prevent the loss of this fluid in the event of a violation of the integrity of the vessels. The combination of these protective mechanisms is called the hemostasis system. There are two main links in the human hemostasis system: vascular–platelet hemostasis and plasma blood clotting system. Blood clotting is a complex network of biochemical reactions that is activated when the integrity of the vascular system is violated. Any disturbances in the delicate balance of this system lead to serious consequences associated with thrombosis or bleeding.The problem of cardiovascular diseases is one of the priority problems of modern medicine, due to the increase in the percentage of mortality of the population every year, while special attention is paid to the role of the human constitution in the development of cardiovascular diseases. Functional and structural changes in the intracerebral arteries that occur in patients with GB during the long course of the disease can cause a variety of neurological and mental disorders, as well as predispose to the development of stroke or transient ischemia. Electrocardiography is a technique for recording and studying the electric fields formed during the work of the heart. Electrocardiography is a relatively inexpensive but valuable method of electrophysiological instrumental diagnostics in cardiology [1,2,4].The problem of the association of migraine with arterial hypertension continues to be studied. Despite numerous studies, the relationship of certain types of migraine (migraine with aura and migraine without aura) with arterial hypertension has not been fully clarified. This question is especially relevant, since these forms differ both clinically and pathophysiologically. Even more important are the analysis and prediction of the links between migraine and cardiovascular diseases – (ischemic stroke, myocardial infarction, coronary heart disease).For the first time, the assumption of a possible connection between headache and arterial hypertension was made by T.C. Janeway back in 1913. After the release of this classic work, the relationship between arterial hypertension and headache became the subject of special attention over the following decades [12,13,23,24,25]. Observations in daily clinical practice revealed cases of a combination of headache and a moderate increase in arterial hypertension. For a long time it was believed that headache is one of the brightest markers of increased arterial hypertension. However, clinical studies often gave contradictory results and did not reveal a link between headache and an increase in arterial hypertension [14,26,27,28]. At the same time, according to some studies, there was a higher frequency of headache [13,29] and migraine [15,30,30] in patients with arterial hypertension. Other studies have demonstrated the prevalence of higher numbers of arterial hypertension in patients with recurrent headache and migraine compared with patients without headache.Hypertension, also known as high blood pressure, is a common medical condition that affects millions of people worldwide. The article defines hypertension as a condition in which the force of blood against the walls of the arteries is consistently too high. The article goes on to describe the symptoms of hypertension, including headaches, shortness of breath, and nosebleeds. It emphasizes the importance of regular blood pressure monitoring and early detection of hypertension to prevent the development of serious complications, such as heart disease, stroke, and kidney failure [1].The article also provides practical tips for preventing hypertension, including maintaining a healthy weight, engaging in regular physical activity, reducing salt intake, and limiting alcohol consumption. It concludes by stressing the need for a comprehensive approach to hypertension management, including lifestyle modifications and medication when necessary.Hypertension is a chronic medical condition that is typically treated with medications, but early stage hypertension can often be managed through lifestyle modifications and non–pharmacological therapies.The article provides an overview of the different non–pharmacological therapies that have been shown to be effective in managing hypertension, including diet modifications, physical exercise, stress reduction techniques, and alternative therapies such as acupuncture and meditation. It highlights the importance of patient education and empowerment in adopting and adhering to these therapies [2].The article also explores the potential benefits of using a multidisciplinary approach to hypertension management, which involves collaboration between healthcare professionals from different disciplines. This approach can help address the complex underlying factors that contribute to hypertension and support patients in making lasting lifestyle changes.The article concludes by stressing the importance of early detection and intervention in hypertension management, and the potential for drug–free therapies to improve outcomes for patients with early stage hypertension.This article examines the effectiveness of drug–free therapies in managing arterial hypertension in the early stages of the disease. The article defines arterial hypertension as a medical condition in which there is persistent high blood pressure in the arteries, and highlights the importance of early detection and intervention to prevent complications [8]. This scientific work reviews various non–pharmacological therapies, including lifestyle modifications such as diet and exercise, stress reduction techniques, and alternative therapies such as acupuncture and biofeedback. It discusses the potential benefits of these therapies, such as reducing blood pressure, improving cardiovascular health, and improving quality of life. The article also discusses the challenges associated with implementing drug–free therapies, such as patient adherence, lack of access to resources, and the need for multidisciplinary care. It emphasizes the importance of individualized care plans and ongoing support from healthcare providers. The article concludes by stating that drug–free therapies have been shown to be effective in managing arterial hypertension in the early stages of the disease. It emphasizes the need for further research to determine the most effective non–pharmacological therapies and to develop strategies to promote their adoption and adherence.This article explores the potential links between migraine and cardiovascular diseases, and the possible mechanisms of interaction between the two conditions. The article defines migraine as a neurological disorder characterized by recurring headaches, and highlights the high prevalence of cardiovascular diseases in individuals with migraine [30].This scientific work is reviews the potential mechanisms of interaction between migraine and cardiovascular diseases, including shared risk factors such as hypertension, dyslipidemia, and obesity. It also discusses the role of endothelial dysfunction, inflammation, and oxidative stress in both conditions. The article also explores the impact of migraine on cardiovascular disease outcomes, such as increased risk of stroke and cardiovascular events. It emphasizes the need for healthcare providers to be aware of the potential links between migraine and cardiovascular diseases and to consider cardiovascular risk assessment in patients with migraine [30].The article concludes by stating that the relationship between migraine and cardiovascular diseases is complex and requires further research to fully understand. It highlights the importance of multidisciplinary care and collaboration between neurologists and cardiologists in managing patients with both conditions.The purpose of the study: to analyze the results of electrocardiography and to study the coagulation system in hypertension.The object of the study: blood taken from patients who have applied for medical help in our clinic of Traditional Medicine.
2. Materials and Methods
- The study included 82 patients of both sexes of a private clinic for convenience, based on gender characteristics, these patients were divided into two age groups, the first group included persons from 35–45 years of age, 18 of them women and 14 men. The second group included persons aged 46 and above, of whom 24 were men and 26 were women. All examined persons of both groups are hypertensive at different stages of the disease. The collection and examination of blood was carried out according to the Sukharev method, i.e. the skin of the ring finger was pierced with a scarifier and blood was placed in a ROE pipette. After that, the time was recorded. Using this method, the beginning and end of the formation of a blood clot, i.e. clotting, were determined.The ECG was taken with the device “Electrocardiograph SE–3”
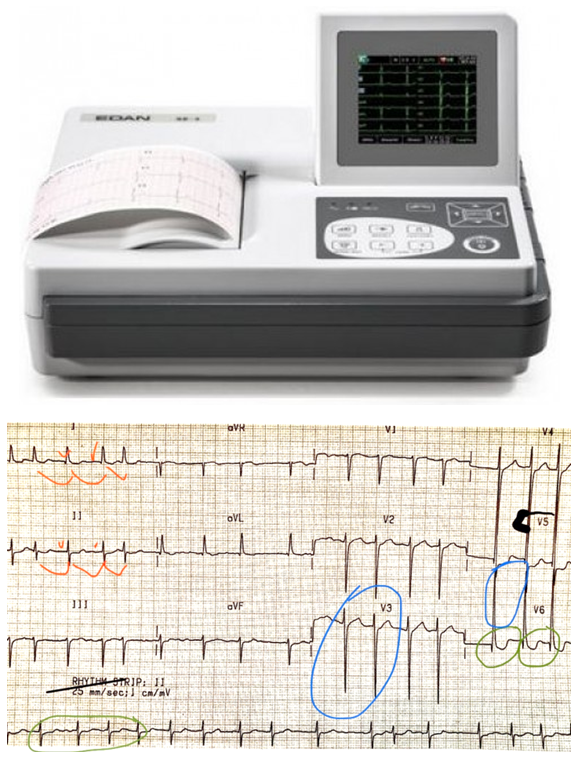 In our patients, we noticed a sign of hypertension is an increase in the left parts of the heart. This occurs due to myocardial volume overload [20,21]. On the ECG, we see an increase in the R teeth in the left thoracic leads and an increase in the S teeth in the right ones. (There is a blue mark in the picture). If you measure the length of these teeth with a millimeter ruler, we get a sum greater than 35 mm. This is the Sokolovsky index–in medicine, a sign of hypertrophy of the left parts of the heart. This means that hypertension has already reached the stage at which the target organs are affected: heart, kidneys, brain [3,5,8,10,17,18].Also on the film we can see signs of myocardial ischemia (marked in green) –this is depression of the S–T segment. Myocardial ischemia is a process of disruption of its nutrition and oxygen delivery, in the future this state of affairs may lead to a heart attack [6,7,9,11,14,16].The anthropometric study was conducted according to the generally accepted rules of anthropometric measurements.
In our patients, we noticed a sign of hypertension is an increase in the left parts of the heart. This occurs due to myocardial volume overload [20,21]. On the ECG, we see an increase in the R teeth in the left thoracic leads and an increase in the S teeth in the right ones. (There is a blue mark in the picture). If you measure the length of these teeth with a millimeter ruler, we get a sum greater than 35 mm. This is the Sokolovsky index–in medicine, a sign of hypertrophy of the left parts of the heart. This means that hypertension has already reached the stage at which the target organs are affected: heart, kidneys, brain [3,5,8,10,17,18].Also on the film we can see signs of myocardial ischemia (marked in green) –this is depression of the S–T segment. Myocardial ischemia is a process of disruption of its nutrition and oxygen delivery, in the future this state of affairs may lead to a heart attack [6,7,9,11,14,16].The anthropometric study was conducted according to the generally accepted rules of anthropometric measurements.3. Results and Discussion
- The Sukharev method is used to measure blood clotting time and determines how long it will take for a fibrin clot to form. The normal parameters of this method are from 30 to 120 seconds for the beginning of fibrin formation and from 3 to 5 minutes for the end of clotting.It can be seen from the observed patients that in all age groups, both men and women, the onset of blood clotting occurred earlier than normal, which may indicate increased blood clotting. The end of blood clotting in all groups occurred a little earlier.In the age group of 35–45 years, women and men had the same blood clotting onset (50 seconds), and the clotting end time was lower than normal (2 minutes 20 seconds for women and 1 minute 50 seconds for men). This may be due to the fact that young people in general have higher blood clotting.In the age group over 46 years, the onset of blood clotting was earlier than normal in women (40 seconds) and men (30 seconds), which may indicate possible hypercoagulation. The end of blood clotting occurred earlier (2 minutes in women and 1 minute 30 seconds in men).Clinical signs of left ventricular hypertrophy occurred in more than 80% of the examined patients with arterial hypertension. Muffling of heart tones in 34%, weakening of the I tone at the apex of the heart in 28%, the presence of a resistant apical shock in 12% of patients. According to literature data, the incidence of left ventricular hypertrophy depends on the severity and duration of arterial hypertension, age, gender, body weight of the patient [9,12,13,15,19,22].Among the patients with arterial hypertension examined by us, the duration of the disease was 8–9 years.To determine individual typological features, all the examined women were divided on the basis of anthropometric data on somatotypes. The analysis of the frequency of occurrence of various constitutional types in patients, depending on the presence of arterial hypertension. The incidence of arterial hypertension was higher in patients with hepersthenic somatotype.
4. Conclusions
- Our studies have shown that in both age groups, coagulation rates were higher in men, i.e. in both studied groups, the blood in men was higher than normal, with prolonged arterial hypertension, left ventricular myocardium overload occurs, an increase in the R teeth in the left thoracic leads and an increase in the S teeth in the right ECG., myocardial ischemia occurs, which is characterized by depression of the S–T segment. It was revealed that the most common areterial hypertension was observed in patients with hypersthenic body type. The currently accumulated clinical, epidemiological and experimental data allow us to speak about the close relationship of pain syndromes, in particular with migraine, with the level of blood pressure. A distinctive feature of the group of patients with migraine is a pronounced direct positive relationship with elevated values of diastolic blood pressure and an inverse relationship with the level of systolic blood pressure. This pattern may be related to the dysfunction of the general mechanisms of regulation of pain and blood pressure. A close anatomical and functional relationship between the antinociceptive system and the control of blood pressure regulation has been proved. Based on experimental and clinical data, a reliable association was revealed between an increase in blood pressure and a decrease in response to pain stimuli. At the same time, blood pressure indicators may remain within the normal range (below 140/90 mm Hg).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML