-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(5): 691-694
doi:10.5923/j.ajmms.20231305.31
Received: May 10, 2023; Accepted: May 22, 2023; Published: May 23, 2023

Signs of Morphofunctional Insufficiency of the Fallopian Tube in the Development of Ectopic Pregnancy
M. I. Shamsutdinova1, F. N. Narkuziev2, D. S. Shadmanova1, R. I. Isroilov1
1Tashkent Medical Academy, Tashkent, Uzbekistan
2Jizzakh Branch of the Republican Research Centre of Emergency Medicine, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the research was to study morphological data on the identification of morphofunctional insufficiency of structural elements of the fallopian tube wall. Background. An ectopic pregnancy (graviditas extrauterina seu ectopica) is a pathological pregnancy in which a fertilized egg develops outside the uterine cavity. The frequency of ectopic pregnancy in relation to the number of gynecological diseases, ranges from 1 to 6%. The causes of ectopic pregnancy are varied. Material and methods. 144 patients with a diagnosis of ectopic pregnancy were admitted to the Department of Emergency Gynecology of the Jizzakh branch of the Republican Research Centre of Emergency Medicine in 2021. The majority of women were represented in the age range from 21 to 34 years (68.0%). The following surgical interventions were performed: 91 cases of laparotomies, 53 laparoscopies. Results. If normally the proper plate of the folds was represented by a loose, unformed connective tissue, then in our studies, various pathomorphological changes were found in the stroma of the folds: in some cases, inflammatory infiltrates predominated in the composition of the lamina propria, in other cases, sclerotic and dysregenerative changes occupied most of the stroma, in the third cases, foci of hemorrhage and necrosis were found. Conclusion. The development of inflammatory, sclerotic and dysregenerative changes in the unformed connective tissue proper lamina of the mucous membrane of the fallopian tube is accompanied by a violation of the elasticity of structural elements and leads to morphofunctional insufficiency in the form of a violation of the egg cell advancement. The defeat of the muscular layer of the fallopian tube wall by inflammatory, sclerotic and dysregenerative changes leads to a weakening of peristalsis and egg retention in the lumen of the tube, which may be accompanied by implantation to the tube wall.
Keywords: Fallopian tube, Ectopic pregnancy, Uterine pregnancy, Morphofunctional insufficiency
Cite this paper: M. I. Shamsutdinova, F. N. Narkuziev, D. S. Shadmanova, R. I. Isroilov, Signs of Morphofunctional Insufficiency of the Fallopian Tube in the Development of Ectopic Pregnancy, American Journal of Medicine and Medical Sciences, Vol. 13 No. 5, 2023, pp. 691-694. doi: 10.5923/j.ajmms.20231305.31.
1. Introduction
- An ectopic pregnancy (graviditas extrauterina seu ectopica) is a pathological pregnancy in which a fertilized egg develops outside the uterine cavity. Depending on the place of egg implantation, tubal pregnancy is most common (98.5-99.5%). Ovarian pregnancy (0.2%), abdominal pregnancy (0.11%) and pregnancy in the rudimentary uterine horn (0.19%) are much less common. The frequency of ectopic pregnancy in relation to the number of gynecological diseases, ranges from 1 to 6%. [1-4]. A large number of studies by domestic and foreign authors had accumulated by the end of the 70s of the 20th century, which provide comprehensive coverage of this frequent pathology of pregnancy. The causes of ectopic pregnancy are varied [5-6]. Sometimes it can occur in connection with the accelerated development of the trophoblast and premature implantation of the egg in the tube on the way to the uterine cavity, especially when the egg moves externally. In the vast majority of cases, the main cause of ectopic pregnancy is a violation of the mechanism for transporting a fertilized egg to the uterine cavity.Most often, violations in the rate of the fallopian tubes contraction and their shape are caused by a transferred or chronically ongoing inflammatory process in the appendages of the uterus, which causes its characteristic changes in the mucosa, muscle membranes, serous membrane, in the nervous and vascular apparatus of the tube [7-10]. The inflammatory process changes the structure and function of the ciliated epithelium of the endosalpinx, leads to the adhesion of the folds of the mucous membrane, the formation of diverticula, narrowing of the lumen The adhesions of the serous cover with the surrounding tissues not only disrupt the motility of the tubes, but also reduce their lumen. All this promotes the delay of the developing egg in the tube cavity, followed by its notation in it. Ectopic pregnancy is characterized by a combination of several contributing causes, but the most common are inflammatory diseases of the uterine appendages.The aim of the research was to study morphological data on the identification of morphofunctional insufficiency of structural elements of the fallopian tube wall.
2. Material and Methods
- 144 patients with a diagnosis of ectopic pregnancy were admitted to the Department of Emergency Gynecology of the Jizzakh branch of the Republican Research Centre of Emergency Medicine in 2021. The majority of women were represented in the age range from 21 to 34 years (68.0%) - in active reproductive age. The mean age of the patients was 29 years. 54 (37.5%) of them had a first pregnancy, 90 (62.5%) ones were with repeated pregnancy. The following surgical interventions were performed: 91 cases of laparotomies, 53 laparoscopies. A pathomorphological study of 30 fallopian tubes was conducted in order to identify the causes of trophoblast dislocation in the isthmic-interstitial, ampullary part of the fallopian tube.
3. Results
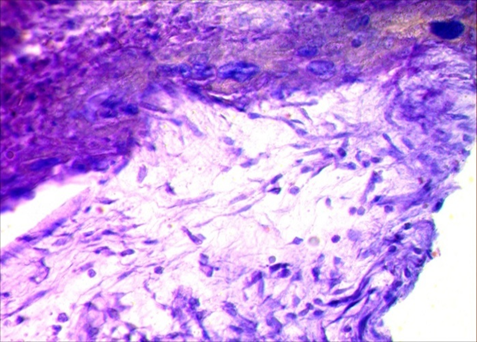
- The results of microscopic examination of the mucous membrane of the fallopian tube during ectopic pregnancy showed that the main morphofunctional deficiencies were found on the part of the integumentary epithelium of the folds of the ampullar part of the tube. Normally, if there is one secretory cell for 3-4 ciliated cells in the ampullary part of the tube among the integumentary epithelium, then in our case there was one secretory cell for 6-8 ciliated cells, which apparently did not produce enough fluid and the ciliated cells did not sufficiently carry out the beating of the egg with their cilia towards the uterus. Another pathomorphological feature of the morphofunctional insufficiency of the fallopian tube was identified from the side of the own plate of folds. If normally the lamina propria was represented by loose, unformed connective tissue, then in our studies, various pathomorphological changes were found in the stroma of the folds: in some cases, inflammatory infiltrates prevailed in the composition of its own plate, in other cases, sclerotic and dysregenerative rearrangements occupied most of the stroma, foci of hemorrhage and necrosis were found in third cases.The fallopian tube performs active movements especially at the time of ovulation due to the increased peristalsis of the muscle layer and activation of the beating of the cilia of ciliated cells. The peristalsis of the muscle layer and the movement of the cilia of the integumentary epithelium are weakened in the presence of the above mentioned pathomorphological changes in the fallopian tube. The movement of the egg is disrupted due to the lack of peristalsis and there is a delay in the lumen of the tube, which leads to implantation to the wall of the tube. During microscopic examination, it was noted that in the presence of the above-described morphofunctional deficiencies on the part of the structural elements of the fallopian tube wall, trophoblasts easily adhered to the integumentary epithelium of the folds, destroying them, possibly due to the enzymatic activity of the trophoblast. In some cases, it was determined that the blastocyst was completely immersed in its own membrane of folds, the surface defect of the integumentary epithelium was covered with a fibrin plug and blood cells. Around the blastocyst, the connective tissue cells of the lamina propria of the tube mucosa became large and light due to true decidualization. The wall of veins and venules ruptured with the appearance of massive hemorrhage foci, especially directly in the circumference of the blastocyst. The trophoblast cells form two layers by this time of the blastocyst implantation to the wall of the fallopian tube. The cells of the inner layer become light and clearly limited and turn into cytotrophoblasts. In the outer layer, trophoblasts are enlarged in size, hyperchromic, the cytoplasm is wide with many nuclei and are called syncytiotrophoblasts. These two types of trophoblasts tightly surround venous vessels, some of them form cavities, others invade the vein wall and lead to hemorrhage. At this stage of blastocyst development in the fallopian tube, the development of massive hemorrhage in the lumen and in the wall of the tube is noted. At the same time, microscopically, in the wall of the fallopian tube, especially in the mucous and submucosal membranes, we observed diffuse germination of blastocyst cell elements, loosening of the structural elements of the tube wall, expansion of venous vessels with massive hemorrhages, in places with the formation of cavities in the form of intermediate lacunae (Fig. 1).
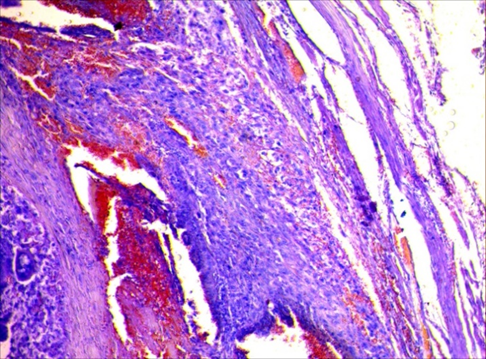 | Figure 1. Infiltration of the tube wall with blastocyst cells, the formation of multiple foci of hemorrhage. HE staining (x400) |
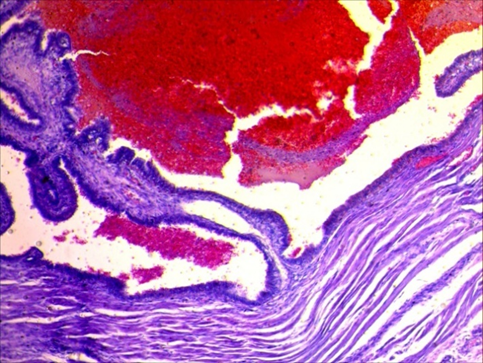 | Figure 2. Fallopian tube: there are blood clots in the lumen due to hemorrhage and bleeding. HE staining (x100) |
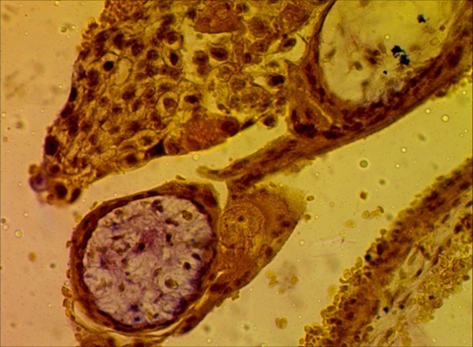 | Figure 3. Primary villi consisting of cytotrophoblasts surrounded by syncytiotrophoblasts. HE staining (x400) |
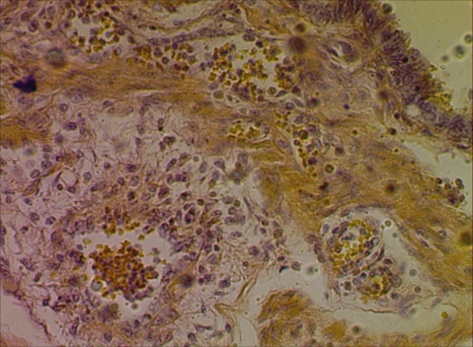 | Figure 4. Hypochromasia of fibrous structures. Van Gieson staining (x400) |
 | Figure 5. Loose connective tissue mesoderm grows into the layer of trophoblasts. HE staining (x400) |
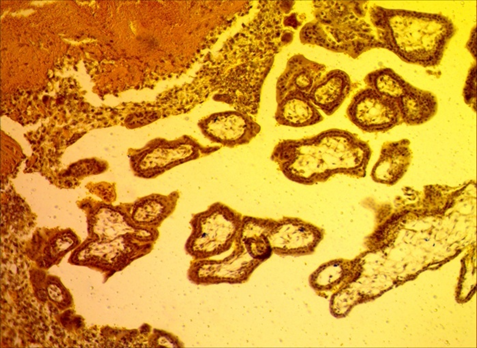 | Figure 6. There is a positively colored fibrinoid in the tube wall, and weakly colored connective tissue is in the chorionic villi stroma. Van Gieson staining (x100) |
4. Conclusions
- The presence of alterative, dystrophic, inflammatory, dysregenerative processes in the wall of the fallopian tube is accompanied by the development of morphofunctional insufficiency of the fallopian tube, which is the reason for the implantation of the blastocyst in the wall of the tube. The dishormonal state of the female body is accompanied by a restructuring of the integumentary epithelium of the fallopian tube with a decrease in the number of secretory cells by half and a shortening of the cilia of the ciliated cells, as a result of which an insufficient amount of fluid is produced and the beating of the egg towards the uterus is weakened, adhesion and implantation of the egg into the wall of the tube occurs.The development of inflammatory, sclerotic and dysregenerative changes in the unformed connective tissue proper lamina of the mucous membrane of the fallopian tube is accompanied by a violation of the elasticity of structural elements and leads to morphofunctional insufficiency in the form of a violation of the movement of the egg.The defeat of the muscular layer of the fallopian tube wall with inflammatory, sclerotic and dysregenerative changes leads to a weakening of peristalsis and retention of the egg in the lumen of the tube, which may be accompanied by implantation to the tube wall. The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML