-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(5): 681-685
doi:10.5923/j.ajmms.20231305.29
Received: May 3, 2023; Accepted: May 16, 2023; Published: May 23, 2023

Tactics of Treatment of Patients with Fournier Gangrene in Patients with Diabetes Mellitus
К. J. Matmurotov, S. A. Parmanov, O. M. Khalikova
Department of General Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: К. J. Matmurotov, Department of General Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The present investigation involved an examination of the outcomes of inpatient therapy for 29 individuals diagnosed with Fournier's gangrene. The study was conducted within the purulent surgery and surgical complications of the diabetes department at the multidisciplinary clinic of Tashkent Medical Academy, spanning the timeframe from 2015 to 2022. The successful management of Fournier's gangrene in patients with diabetes mellitus involved intricate surgical interventions that led to prompt scrotal wound healing. The resulting wound defects were addressed through diverse skin plastic and reconstructive procedures utilizing local tissue, thereby averting disability in this challenging patient population.
Keywords: Diabetes mellitus, Fournier's gangrene, Sepsis
Cite this paper: К. J. Matmurotov, S. A. Parmanov, O. M. Khalikova, Tactics of Treatment of Patients with Fournier Gangrene in Patients with Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 13 No. 5, 2023, pp. 681-685. doi: 10.5923/j.ajmms.20231305.29.
Article Outline
1. Introduction
- Despite the significant advancements in modern medicine, the issue of anaerobic infection in soft tissues remains a topic of great interest among medical professionals across various fields of specialization. The aforementioned scenario is attributed to the distinctive position held by anaerobic infection, characterized by the ailment's seriousness, the intricacy of selecting appropriate therapy, and a significant fatality rate ranging from 14% to 80% [1,5,9].The etiology and pathogenesis of necrotizing fasciitis of the genital organs remain a topic of ongoing debate and lack a definitive consensus. The investigation of exudate derived from wounds typically reveals the presence of Staphylococcus aureus, hemolytic streptococcus in associations, Escherichia coli Enterococcus, and Proteus in the majority of cases. Research on the culture extracted from the wound confirmed the presence of anaerobic-aerobic associations in 33% of the cases, with the fungal flora becoming a part of the culture in the advanced stages of the wound [4,7].Familiarity with the clinical characteristics of anaerobic infection in the context of diabetes mellitus enables timely identification of this perilous ailment in its incipient stages and initiation of a therapeutic regimen without delay. Various terms have been used in the literature to describe Fournier's gangrene (phlegmon), including fulminant gangrene of the vulvar skin, idiopathic phlegmon of the scrotum, epi fascial necrosis, spontaneous gangrene of the scrotum, gangrenous erysipelas of the scrotum, and Fournier's syndrome [2,3,10].Phlegmon Fournier, also known as gangrene Fournier, is a medical condition characterized by acute necrosis of the tissues of the scrotum and penis. This condition is caused by the introduction of anaerobic microorganisms into the skin. One of the contributing factors to the incidence of Fournier's phlegmon is the unique characteristics of the blood supply to the scrotum. The presence of a limited arterial network and a substantial venous bed contributes to a reduced rate of blood efflux. The occurrence of edema leads to a further disturbance in the flow of arterial blood, creating a conducive environment for the advancement of the putrefactive process [8,12].The scrotal skin and subcutaneous fatty layer undergo necrosis, which gradually extends over the superficial and deep fascia, as documented in sources 3 and 11. The testes and their associated appendages are typically not implicated as they possess an independent vascular network. The scientific community lacks agreement regarding the management of patients afflicted with Fournier's gangrene, particularly those with diabetes mellitus. Fournier's gangrene presents atypically in DM patients and frequently results in septic complications, thereby elevating the probability of mortality [6,13].The objective of this study was to examine the clinical progression of Fournier's phlegmon and the treatment options available in the context of diabetes mellitus.
2. Material and Methods
- The present investigation involved an examination of the outcomes of inpatient therapy for 29 individuals diagnosed with Fournier's gangrene. The study was conducted within the purulent surgery and surgical complications of the diabetes department at the multidisciplinary clinic of Tashkent Medical Academy, spanning the timeframe from 2015 to 2022. The study population consisted of individuals diagnosed with type 2 diabetes mellitus, with a mean age of 53.6±6.2 years. The mean duration of inpatient treatment, as measured by bed days, was 10.4 days. Although intricate therapeutic interventions were employed, 3 patients (10.3%) experienced a fatal outcome as a result of multiple organ failure in the context of severe intoxication and sepsis syndrome. The findings indicate that the majority of patients, specifically 86.2%, experienced an abrupt onset of Fournier's phlegmon, which is characterized as a spontaneous form of the disease. A smaller proportion of patients, 13.8%, developed the condition as a secondary occurrence following scrotal or perineal surgery. Additionally, 10.3% of cases were observed in patients with a history of orchoepididymitis, while one patient, accounting for 3.4% of cases, developed the condition after undergoing a Winkelmann operation for the treatment of scrotal dropsy.Upon admission to the clinic, all patients underwent comprehensive clinical and instrumental evaluations, including radiological examinations and electrocardiograms. Additionally, blood cultures and cultures of wound exudate were obtained to identify the pathological flora and determine the appropriate antibiotic therapy strategy. The patients were administered volume infusion therapy with forced diuresis in addition to antibiotic therapy. The cardiologist and endocrinologist provided additional consultation to the patients to correct any issues about their respective organs and systems.Intensive care was administered to all patients, as it constituted a crucial component of the anaerobic infection treatment regimen. The process of correcting blood sugar levels through the administration of insulin therapy. Antibiotic therapy refers to the use of antibiotics to treat bacterial infections. Initially, a combination of broad-spectrum antibiotics (III-IV generation fluoroquinolones, combined III-IV generation cephalosporins, carbohydrates, and clindamycin) along with systemic antifungal agents were administered due to the presence of a mixed microbial etiology. Subsequently, the prescription was adjusted based on the results of the bacteriological analysis of the wound discharge.The patient received a significant amount of infusion therapy, with a maximum infusion volume of three liters per day. The infusions included colloids, crystalloids, and protein preparations. Prophylaxis for thrombosis and embolism involves the use of low molecular-weight heparin and antiaggregants. Antihypoxants and immunomodulators, specifically Neupogen, are under consideration.
3. Result and Discussion
- Symptomatic therapy refers to the treatment of symptoms associated with a particular medical condition, without addressing the underlying cause of the condition itself. In 8 instances, comprising 27.6% of the cases, patients were transferred to an intensive care unit for infusion therapy and short-term preparation for surgery due to a critical condition, specifically severe intoxication. In all instances, the patients underwent emergency surgery.The findings of the data analysis indicate that diabetes mellitus is a significant contributing factor to the onset of Fournier's gangrene, as evidenced by its presence in all patients and the consistent observation of perineal or inguinal fasciitis symptoms in all cases. The study revealed that a proportion of 24.1% of patients was diagnosed with cardiovascular diseases, including hypertension, IBS, and PICS. Additionally, 6.7% of patients were found to have alcoholism, while 13.4% presented with urinary tract and pararectal infections. Furthermore, one patient had a history of long-term use of hormones and cytostatics for rheumatoid arthritis.Typically, the start of the illness is acute, characterized by symptoms of intoxication such as general weakness, a sudden elevation of body temperature to febrile levels (40°C), tachycardia, chills, and hyperdynamic. The presence of a foul-smelling and stinking lesion in the soft tissues was a distinctive feature, with the typical local indicators of infection being absent and instead, symptoms of systemic toxicity being prevalent.The usual clinical manifestations observed in the local area include swelling and hyperemia of the scrotum and penis, which appear 12-24 days after the onset of the condition. In most cases, the scrotum turns black on day 3. The scrotal skin exhibited a progressive discoloration towards a purplish-blue color, accompanied by the development of areas of skin and subcutaneous fat necrosis. The discharges that come from the infections on the scrotal region exhibited a grayish color accompanied by the presence of fluid bubbles and an unpleasant olfactory perception. The affected region exhibited a lack of tactile sensitivity.Clinical observation.The patient under consideration, identified as T.I. and born in 1967, carries the unique identifier №7651/672. The patient was admitted on March 12th, 2020, with symptoms including pain, redness, a purulent-necrotic wound, and blackening in the scrotal area. Additionally, the patient had an elevated body temperature of up to 39.5°C and reported a loss of appetite. The patient has had a medical history of diabetes mellitus for 13 years and is currently undergoing continuous treatment with antidiabetic medication, specifically insulin. The patient underwent a three-day course of outpatient treatment at their place of residence. Despite receiving treatment, the patient's condition deteriorated, prompting him to seek inpatient care at our clinic.Upon admission, the patient's condition was considered to be severe. The coloration of the skin and mucous membranes is sickly pale. The individual's blood pressure reading is 90/60 mmHg. The individual's pulse rate is 110 beats per minute. The examination of the lungs revealed the presence of weak vesicular breathing. The abdominal region exhibits a visible softness and absence of discomfort. There is no evidence of swelling. The stool movements were consistent, while there was a reduction in the quantity of urine passed over the past day.Blood analysis: Hb - 123 g/l, Erythrocyte - 3.3 x1012, Leukocyte – 28 x 109, stab neutrophils- 11, segmented neutrophils- 86, ESR-19, blood glucose level - 11.5 mmol/l. Urea - 9.5 µmol/l, kreatinine - 128.7 mmol/l. Fibrinogen - 788. BFT- start: 4-50- end: 5-50.Locally: The scrotum exhibits significant swelling, discomfort, and the formation of e accompanied by indications of the under-the-skin condition. The affected region exhibits pain and erythema that radiates towards the inguinal and pararectal regions inferiorly. Necrosis of the skin and subcutaneous tissue measuring 15.0 cm x 10.0 cm can be seen as depicted in Figure 1. Bilateral inguinal lymphadenopathy is present with associated tenderness. The scrotal ultrasound reveals a significant infiltration of soft tissue in the scrotal area, accompanied by the accumulation of fluid. The individual is diagnosed with Fournier's gangrene.
 | Figure 1. Condition of scrotum and perineum on admission |
 | Figure 2. Condition after surgery (3rd day) |
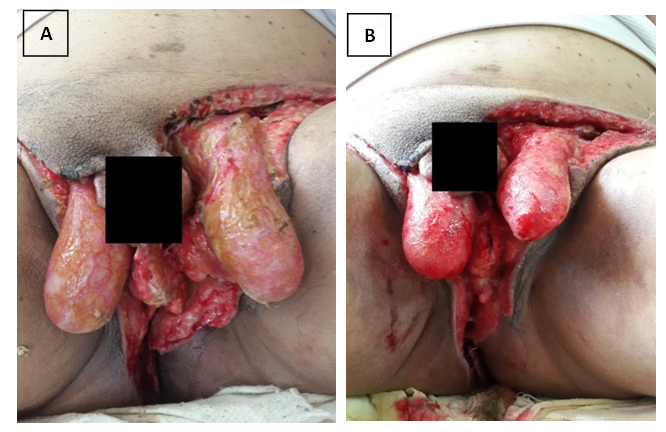 | Figure 3. View of the wound on day 7 (A) and day 18 (B) after surgery |
 | Figure 4. Phase 3 of the wound process (32nd postoperative day) and outcome (64th day) |
4. Discussion
- The prompt and appropriate implementation of surgical procedures and personalized, all-encompassing intensive care are crucial factors in managing and achieving a positive prognosis for anaerobic infections.The temporal aspect of surgical care organization holds significant and occasionally conclusive sway over the prognosis of the disease direction, given the rapid and expansive propagation of anaerobic infection in both distal and proximal directions, thereby exacerbating the patient's overall state and augmenting the likelihood of surgical intervention.The primary steps in an integrated treatment approach for patients with Fournier's gangrene with DM involve the radical surgical intervention of the purulent-necrotic focus, subsequent daily dressings, de-escalating antibiotics, and planned infusion therapy, contingent upon the patient's condition, according to our perspective. The surgical intervention necessitates an extensive excision of the infected tissue, encompassing the visually unaffected regions, and a meticulous neurectomy procedure while avoiding the exposure of the testes. Despite the removal of all affected layers from the testes, preservation is prioritized to prevent dyshormonal conditions. Our observations have consistently shown that even with massive lesions, the testes can be preserved. It is recommended that surgical intervention be conducted following a brief preoperative preparation period, which should not exceed two hours. Surgical intervention in patients with septic shock was conducted exclusively after the stabilization of arterial pressure. Furthermore, surgical intervention upon admission was restricted to incisions for pus drainage and tissue aeration. A staged neurectomy was carried out along with wound debridement to address the progression of inflammation and removal of necrotic tissue.Typically, the third stage of the wound healing process was resolved through the implementation of diverse dermal plastic techniques. The timely execution of reconstructive plastic surgery in individuals with diabetes mellitus is crucial due to the loss of proteins and electrolytes through the extensive wound surface, as well as the contamination of the wound with antibiotic-resistant flora commonly found in hospital settings. This is a significant aspect of the management of patients with diabetes mellitus.The successful management of Fournier's gangrene in patients with diabetes mellitus involved intricate surgical interventions that led to prompt scrotal wound healing. The resulting wound defects were addressed through diverse skin plastic and reconstructive procedures utilizing local tissue, thereby averting disability in this challenging patient population.
5. Findings
- 1. In the context of diabetes mellitus, the growth of the putrefactive process in Fournier's gangrene exhibits a more aggressive course compared to cases without the condition. The aforementioned phenomenon can be attributed to a reduction in bodily reactivity, the diverse nature of bacterial flora, and the anatomical composition of the perineum and inguinal regions.2. The treatment necessitates prompt surgical intervention, including radical surgery, staged neurectomy, skin grafting, and reconstruction of the wound with local tissue, as well as multicomponent intensive care.3. The timely and appropriate initiation of de-escalation antibiotic therapy is crucial for achieving the desired outcome, particularly in cases where patients have undergone multiple surgical interventions and received insufficient antibiotic treatment.
Competing Interests
- The authors have declared that no competing interests exist.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML