-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(5): 678-680
doi:10.5923/j.ajmms.20231305.28
Received: May 1, 2023; Accepted: May 15, 2023; Published: May 23, 2023

Efficiency of the Ursodeoxycholic Acid in Patients with Metabolic Syndrome
Avazova Takhmina Akhtamovna, Ziyadullaev Shukhrat Khudoyberdiyevich
Department of Internal Medicine No.1, Samarkand State Medical University, Uzbekistan
Correspondence to: Avazova Takhmina Akhtamovna, Department of Internal Medicine No.1, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Metabolic syndrome is a cluster of factors associated with an increased risk of atherosclerotic cardiovascular disease and diabetes mellitus. In recent years, this syndrome has attracted close attention from cardiologists, endocrinologists and general practitioners. This is due to the widespread occurrence of this symptom complex in the population. Forty patients with MS were examined. All persons determined by the content IL-6, IL-17 in the blood serum before and after immune disorders correctiveby Ursosan forte. It is established that the MS increases the level of IL-6 and IL-17. The therapy had a positive impact on cytokine status. The activation of cytokine system occurs in metabolic syndrome and manifests as a significant in-crease of IL-6 and IL-17 in blood serum.
Keywords: Metabolic syndrome, Cytokines, IL-6, IL-17, Ursodeoxycholic acid
Cite this paper: Avazova Takhmina Akhtamovna, Ziyadullaev Shukhrat Khudoyberdiyevich, Efficiency of the Ursodeoxycholic Acid in Patients with Metabolic Syndrome, American Journal of Medicine and Medical Sciences, Vol. 13 No. 5, 2023, pp. 678-680. doi: 10.5923/j.ajmms.20231305.28.
1. Introduction
- Metabolic syndrome is a cluster of factors associated with an increased risk of atherosclerotic car-diovascular disease and diabetes mellitus [4-17]. In recent years, this syndrome has attracted close attention from cardiologists, endocrinologists and general practitioners. This is due to the widespread occurrence of this symptom complex in the population.Currently, one of the main factors in the development of cardiovascular vascular pathology is considered to be immune inflammation. Elevated inflammatory indicators such as interleukins (IL)-1, 6, tumor necrosis factor- (TNF-α) are associated with a high risk of complications in cardiac pathology and considered to be immunological markers of cardiovascular risk [2]. The main 'metabolic risk factors' are atherogenic dyslipidaemia, elevated blood pressure, elevated plasma glucose, prothrombotic state and pro-inflammatory state. The presence of this cluster of factors in a particular patient is referred to using the clinical concept of "metabolic syndrome" [18], and it is not necessary for all metabolic risk factors to be present in order to diagnose this phenomenon.Interleukin-6 (IL-6) is synthesized by monocytes / macrophages, less by fibroblasts, endothe-lial cells during inflammation, trauma, hypoxia and exposure to bacterial endotoxins [1]. The bio-logical role of IL-6 lies primarily in the induction of repair mechanisms and activation of immune protection (activation and differentiation of T-cells, maturation of B-cells, synthesis of C-reactive protein in the liver, enhancement of hematopoiesis). In addition, IL-6 is also known to inhibit the inflammatory response by inhibiting the synthesis of a number of pro-inflammatory substances, including tumour necrosis factor a (TNFa) [1]. In the last decade, the role of IL-6 in the regulation of metabolism has been established. Interest in IL-6 has particularly increased with the discovery of the adipose tissue inflammation phenomenon in obesity and the search for its pathogenetic mechanisms. Besides the research interest in this side of cytokine action, the practical aspect is important due to the increase in metabolic diseases: obesity, metabolic syndrome (M.S.), type 2 diabetes mellitus (DM-2) and related atherosclerosis and its consequences.Due to the range of inherent pleiotropic properties (choleretic, cytoprotective, immuno-modulatory, anti-apoptotic, hypocholesterolemic, and litholytic), Ursosan forte has a wide range of therapeutic effects. The aim of our work was to study the content of interleukins 6 and 17 in patients with metabolic syndrome before and after therapy with Ursosan forte.
2. Materials and Methods
- We examined the clinical and immunological parameters of 40 subjects, including 18 females and 22 males aged 25-55, with a body mass index of 25.0-32.2 kg/m2 and 30 healthy controls.Metabolic syndrome was identified based on the International Diabetes Federation criteria (IDF, 2007). All subjects were measured for interleukin IL-6 and IL-17 in blood serum by ELISA test using the Vector-Best test system, Russia, and a set of anthropometric data (height, weight, body mass index, waist circumference and hip circumference).All patients have prescribed Ursosan forte 500 mg at night for 30 days on a hypocaloric diet.All patients were informed about the forthcoming treatment, and their written consent was taken.The patients were divided into groups according to their B.P. and BMI.Depending on blood pressure level, patients were divided into 2 groups: those whose blood pressure did not exceed 140/80 mmHg (19 people) and those with blood pressure higher than 140/80 mmHg (21 people).Depending on BMI, Group 1 included 20 patients with BMI less than 30 kg/m2 and Group 2 included 20 patients with type I obesity (BMI greater than 30 kg/m2).The data were statistically processed using a R-studio version 3.6.2. as well as using the programs developed in the EXCEL package with the library of statistical functions.
3. Results
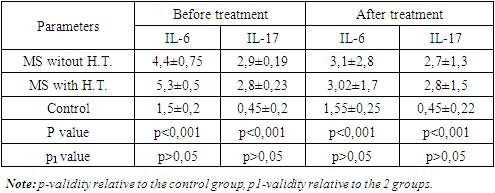
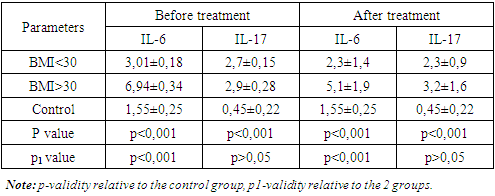
- Table 1 presents data on IL-6 and IL-17 content in blood serum in MS depending on B.P. level before and after monotherapy with ursosan forte.
|
|
4. Conclusions
- The activation of the cytokine system occurs in metabolic syndrome and manifests as a significant increase of IL-6 and IL-17 in blood serum. IL-6 and IL-17 levels are significantly higher in obese and overweight patients. Therapy with ursosan forte showed a positive effect on cytokine status.
ACKNOWLEDGEMENTS
- We acknowledge the support of Khasan IBRAGIMOV on preparation of this manuscript.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML