-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(5): 672-677
doi:10.5923/j.ajmms.20231305.27
Received: Apr. 25, 2023; Accepted: May 10, 2023; Published: May 17, 2023

Identifying the Key Anatomic Structures Contributing to Reduction Loss Following Hybrid Stabilization of Osteoporotic Thoracolumbar Spine Fractures
Mukhsin Rajabov1, Abdurakhmon Norov2
1Bukhara Branch of the Republican Scientific Center of Emergency Medical Care, Bukhara, Uzbekistan
2Bukhara Regional Multidisciplinary Medical Center, Bukhara, Uzbekistan
Correspondence to: Abdurakhmon Norov, Bukhara Regional Multidisciplinary Medical Center, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction. Hybrid stabilization has been established as a viable treatment strategy for unstable osteoporotic thoracolumbar fractures. However, reduction loss remains a concern, and the specific anatomical structure responsible for this loss is not well-defined.Methods. This retrospective study was conducted at Bukhara Regional Multidisciplinary Medical Center and involved patients aged 61 and older who underwent hybrid stabilization following acute and unstable osteoporotic vertebral body fractures in the thoracolumbar spine. Posterior stabilization was performed using short-segmental and minimally invasive techniques with cement-augmentation of all pedicle screws. The minimum follow-up period was 2 years, and outcome parameters included reduction loss, relative loss of height of adjacent intervertebral discs, fractured vertebral body, and a reference disc (the intervertebral disc superior to the stabilization) between postoperative and latest lateral radiographs. Implant positioning and loosening were also analyzed. Results. The study included 29 patients, mainly female (72%), with a mean age of 73.3 ± 6.0 years. Fractures consisted of 26 incomplete burst fractures and 3 complete burst fractures, primarily located at the thoracolumbar junction (86%) and midlumbar spine. The mean follow-up time was 36 months (range: 24–58 months). The mean reduction loss was 7.7° (range: 1–25), and significant relative loss of heights was observed in both adjacent intervertebral discs, the reference disc, and the central vertebral body. The superior adjacent disc height had the highest loss and was significantly greater than the reference disc. The relative loss of central vertebral body height and reduction loss showed significant correlation. No implant loosening was observed in any patient. Conclusions. Moderate reduction loss was observed 3 years after hybrid stabilization of unstable osteoporotic vertebral fractures of the thoracolumbar spine. Significant loss of heights was observed in both adjacent intervertebral discs and the central vertebral body, with the highest loss occurring in the superior adjacent disc. The superior adjacent intervertebral disc and the central part of the fractured vertebral body were identified as potential contributors to reduction loss.
Keywords: Osteoporotic thoracolumbar vertebral fractures, Hybrid stabilization, Fractured vertebral body, Unstable osteoporotic vertebral fractures, Thoracolumbar spine
Cite this paper: Mukhsin Rajabov, Abdurakhmon Norov, Identifying the Key Anatomic Structures Contributing to Reduction Loss Following Hybrid Stabilization of Osteoporotic Thoracolumbar Spine Fractures, American Journal of Medicine and Medical Sciences, Vol. 13 No. 5, 2023, pp. 672-677. doi: 10.5923/j.ajmms.20231305.27.
1. Introduction
- Hybrid stabilization is a widely accepted treatment option for unstable osteoporotic thoracolumbar vertebral fractures, leading to positive clinical outcomes for the majority of patients [1,2]. Hybrid stabilization of the spine typically involves the use of vertebral augmentation techniques such as vertebroplasty (a procedure in which a special material, such as cement, is injected into the vertebra) as well as the implantation of metallic rods, screws, and/or plates into the spine. While trauma-associated intervertebral disc lesions following osteoporotic vertebral fractures are unlikely, a significant loss of intact intervertebral disc heights cannot be ruled out despite age-related sclerotic changes and posterior stabilization [1]. One of the issues associated with hybrid stabilization of the spine is the reduction of vertebral bodies, which is the loss of vertebral height. This can occur due to many factors, including degenerative changes in the intervertebral discs and the lack of additional support for stabilization. To reduce the risk of vertebral body reduction, surgeons may take various measures such as using more rigid implants, more precise surgical planning, and more careful patient selection for surgery.There are many studies that investigate the effectiveness of hybrid stabilization of the spine and the risks associated with vertebral body reduction. These studies help surgeons better understand how to minimize the risk of vertebral body reduction and improve surgical outcomes for patients. A previous study by Spiegl et al. [2] reported a mean reduction loss of over 7° after hybrid stabilization of osteoporotic vertebral fractures, but it remains unclear which anatomic structures are responsible for this loss. Is the reduction loss localized at the fractured vertebral body or at the adjacent intervertebral discs?The objective of our study was to examine the location of reduction loss after hybrid stabilization of unstable burst fractures of the thoracolumbar spine in patients aged 60 years or older. We hypothesized that the majority of the reduction loss would be located at the fractured vertebral body without significant participation of the adjacent vertebral discs.
2. Materials and Methods
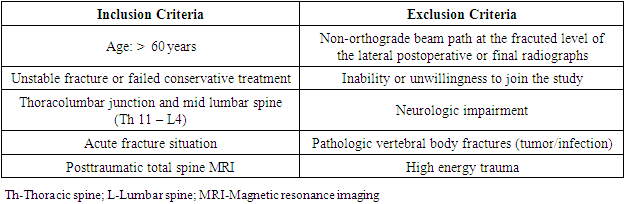
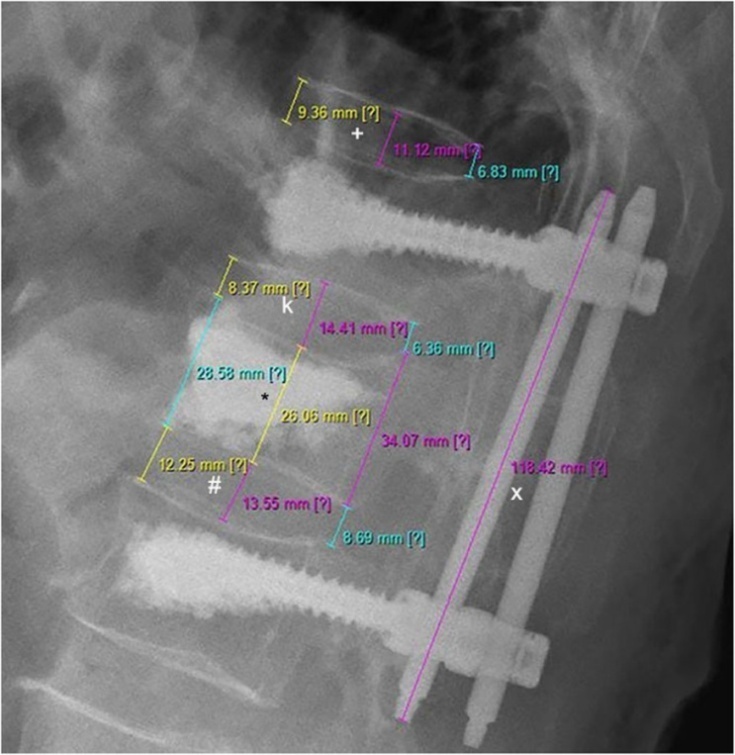
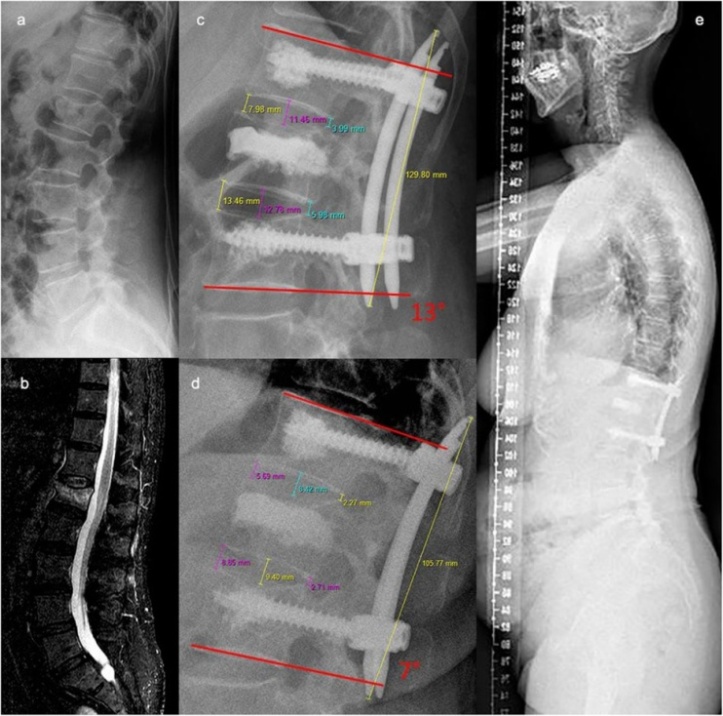
- This retrospective study was conducted at Bukhara Regional Multidisciplinary Medical Center between December 2016 and September 2021, and aimed to further investigate the impact of hybrid stabilization on unstable osteoporotic vertebral fractures of the thoracolumbar spine. Our study cohort consisted of patients aged 61 and older who underwent the procedure using short-segmental and minimally invasive techniques with cement-augmentation of all pedicle screws. To ensure accurate analysis of disc and vertebral body heights, only patients with orthograde beam path of both postoperative and latest lateral radiographs were included in the study, which differed from our previous investigation. Additionally, posttraumatic MRI was employed to evaluate potential intervertebral disc lesions. The study was approved by the regional ethics committee and all inclusion and exclusion criteria are listed in Table 1. Through our analysis, we aimed to better understand the specific anatomical structures responsible for reduction loss following hybrid stabilization, as well as evaluate the efficacy of the procedure in achieving stable outcomes for these patients.
|
3. Results and Discussion
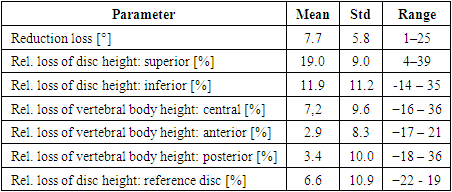
- A total of 29 patients who met the inclusion criteria were included in the study. The mean age of the patients was 73.3 years (range: 61 to 98 years), with the majority being female (72%). Most fractures occurred at L1 (n=11) and Th12 (n=8), with fewer fractures at L2 (n=5), L3 (n=3), Th11 (n=1), and L4 (n=1). Most of the fractures were incomplete burst fractures, with 20 OF 3 fractures having significant involvement of the posterior cortex and 6 OF 2 fractures having minor involvement of the posterior cortex and an OF score of at least 6. Three patients had complete burst fractures (A4; OF 4). All patients with OF 2 fractures had persistent pain and acquired significant loss of reduction after mobilization. The mean follow-up time was 36 months (range: 24-58 months). Post-traumatic MRIs did not reveal any obvious trauma-related intervertebral disc lesions. During the follow-up period, a total of three patients suffered from adjacent fractures (10.3%).The average loss of reduction was 7.7° (range: 1° – 25°). The relative loss of vertebral body and intervertebral disc heights are presented in Table 2. The heights of both adjacent intervertebral discs (superior disc: p < 0.001; inferior disc: p = 0.001), the reference disc (p = 0.003), and the central part of the fractured vertebral body (p = 0.006) were significantly reduced at the latest follow-up compared to the postoperative radiographs. The relative loss of height of the superior adjacent disc was significantly higher compared to the reference disc (p = 0.001). However, only the relative loss of central vertebral body height and loss of reduction had a significant correlation (coef = − 0.471; p = 0.048). The changes of the anterior and posterior vertebral body heights were not significant. Overall, there was significant variability in all parameters.
|
4. Conclusions
- The study found that there was a moderate amount of reduction loss three years after performing hybrid stabilization for unstable osteoporotic vertebral fractures in the thoracolumbar spine. The analysis showed a significant loss in both disc heights adjacent to the fractured vertebral body and the central vertebral body height, with the superior disc experiencing the greatest loss compared to the reference disc. This suggests that the superior disc and central part of the fractured vertebral body may be responsible for the majority of the reduction loss observed.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML