Azimova Kamola Talatovna1, Garifulina Lilya Maratovna2
1Doctoral Student of the Department of Pediatrics No. 3 and Medical Genetics, Samarkand State Medical University, Uzbekistan
2Head of the Department of Pediatrics, Faculty of Medicine, Samarkand State Medical University, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
38 children with acute bronchiolitis aged from 2 months to 2 years were examined, and children were observed from September to March 2021-2022. Conducted clinical and laboratory examinations of children with the definition of cytokine status. It was revealed that the main etiological factor of acute bronchiolitis continues to be RSV in modification (50%), with a high frequency of mixed infection with RSV (34.2%), while the occurrence of acute bronchiolitis occurred against the background of aggravated family history. The use of the ESBA acute bronchiolitis severity scale made it possible to assess the child's condition immediately after the doctor's examination, before the use of instrumental research methods. The relationship between the expression of interleukins depending on the severity of acute bronchiolitis, characterized by an increase in the concentration of IL-6 IL-8 and TNFα, depending on the severity of the disease, was revealed. The revealed changes in the content of interleukins can be used as markers for predicting the severity of the course of the pathological process. Patients with mixed infection (RSV and with Chlamydia pneumonia and RSV in modification had higher interleukin profile values.
Keywords:
Acute bronchiolitis, Children, Acute bronchiolitis severity scale, Interleukins
Cite this paper: Azimova Kamola Talatovna, Garifulina Lilya Maratovna, Features of the Clinical Characteristics of Acute Bronchiolitis in Children in Relationship with Cytokine Status, American Journal of Medicine and Medical Sciences, Vol. 13 No. 5, 2023, pp. 647-652. doi: 10.5923/j.ajmms.20231305.21.
1. Introduction
Acute bronchiolitis has been and is one of the most severe obstructive inflammatory diseases of the lower respiratory tract in young children [1,2]. Along with this, acute bronchiolitis is one of the most common diseases of the lower respiratory tract in young children. Literature data indicate that about 3% of children in the first year of life are hospitalized for acute bronchiolitis [3], which is more than 125 thousand hospitalized children annually in the United States alone [4]. According to experts, 33.8 million new episodes of lower respiratory tract infection occur annually among children under the age of 5 years, associated with a respiratory syncytial virus (RS-virus), which is one of the most common causative agents of acute bronchiolitis in children [5,6]. In this regard, the problem of acute bronchiolitis in children does not lose its relevance.Currently, much attention is paid to pro- and anti-inflammatory cytokines involved in immune processes, the action of which is associated with biological effects that determine the severity and outcome of acute respiratory viral infections, including acute bronchiolitis [7].Along with the studied properties of tumor necrosis factor α (TNFα), which have universal antiviral properties, a special role is assigned to IL-6 and IL-8. As a result of indirect immunoregulation of inflammatory processes, by influencing the production of IL-8 and IL-6, protection is realized against many types of pathogens, including viruses. In this regard, we were interested in studying the features of the cytokine status in children with acute bronchiolitis [8,9].Purpose of the study: to determine the features of the clinical characteristics of acute bronchiolitis concerning the cytokine status in young children.
2. Material and Research Methods
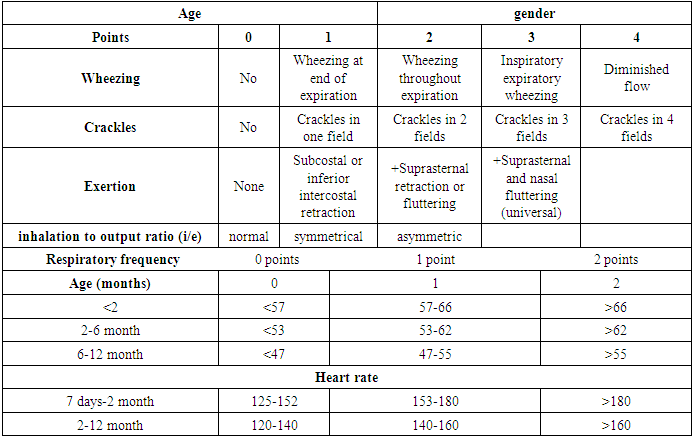
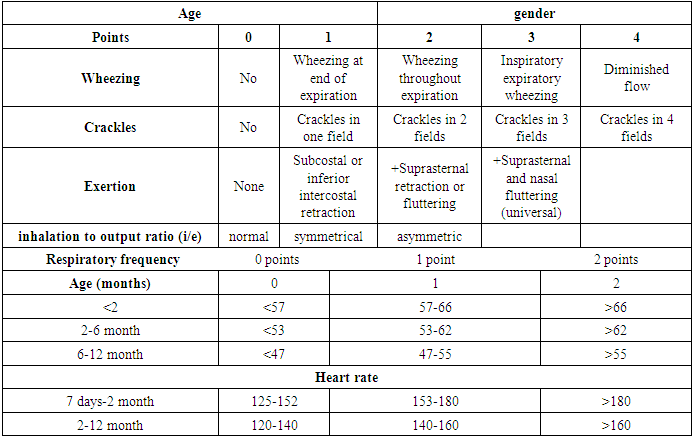
38 children with acute bronchiolitis aged from 2 months to 2 years were examined. At the same time, boys accounted for the advantage, 2/3 of the observed - 63.1% (24), and girls 36.8% (14).Given the predominant autumn-winter seasonality of the disease, children were observed from September to March, our studies were carried out in the period 2021-2022. The observed sample of patients, depending on the severity of the condition, was hospitalized in the department of pulmonology and the intensive care unit of the Samarkand Regional Children's Multidisciplinary Center and in the department of emergency pediatrics and the pediatric intensive care unit of the Samarkand branch of the Republican Scientific Center for Emergency Medical Care. All children of the observed group had bronchial obstruction of varying degrees.The criteria for exclusion from the observation group were congenital diseases of the bronchopulmonary, cardiovascular, and central nervous systems. Patients were hospitalized in accordance with the specifics of the work of the emergency medical service, according to the standards of diagnosis and treatment (the recommended length of stay of a sick child in a hospital was observed). Subsequently, the condition of patients was monitored, who continued their treatment on an outpatient basis.To assess the prognosis of the severity of the course of bronchiolitis, a point scale was used based on clinical and auscultatory signs of ESBA (J.M. Ramos Fernandez et all, 2013) (Table 1) [10].Table 1. Acute Bronchiolitis Severity Scale (Escala de Severidad de la Bronquiolitis Aguda, ESBA), J.M. Ramos Fernandez et all, 2013) Wheezing/crackles---exertion---inspiration/expiration ratio
 |
| |
|
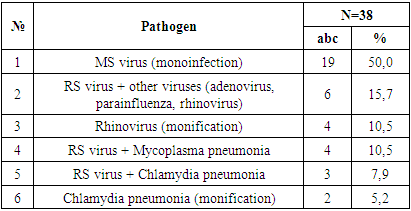
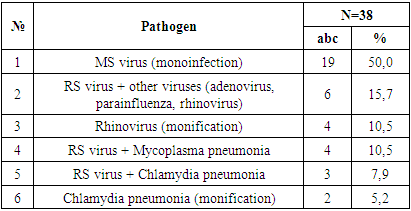
All patients with acute bronchiolitis underwent a laboratory and instrumental examination, including a complete blood count, a biochemical blood test with the determination of C-reactive protein (CRP), blood gases, oxygen saturation (SpO2), and a chest x-ray. As markers of a bacterial infection, the following were considered: leukocytosis above 15x109/l; neutrophilia above 10x109/l; neutrophil index: the ratio of young forms of neutrophils (myelocytes, metamyelocytes, promyelocytes, stab neutrophils) to mature forms (segmented neutrophils) is more than 0.2; CRP above 5 mg/l.All patients underwent real-time polymerase chain reactions to detect viral antigens (RSV, adenovirus, rhinovirus, parainfluenza). Reverse transcription and PCR reactions were carried out using commercial kits "Reverta" and "Amplisens-200" (Russian Federation). To determine the infection with pathogens of persistent intracellular infections (Chlamydia pneumonia, Mycoplasma pneumonia), an enzyme-linked immunosorbent assay (ELISA) was performed using a standard commercial kit of reagents "CHEMA" (Russia).Statistical processing of the obtained results was carried out using Microsoft Excel 2013 and Stat Soft, Statistic 10 software. For all qualitative indicators, the frequency of occurrence of the trait was calculated, and for each quantitative indicator in the entire sample and in the studied groups, the mean value was calculated with the standard error of the mean (M± m). The critical value of the level of statistical significance of the null hypothesis in all cases was taken equal to 0.05.Research results showed that, the highest incidence of acute bronchiolitis in the year of the study was observed in November 34.% (13) and December 28.9% (11), then in January 21.05% (8), while the remaining cases were observed in the range from September to March month 15.7% (6).When conducting a PCR study of the blood serum of children admitted to the hospital, it was revealed that the main etiological factor of acute bronchiolitis was respiratory syncytial virus 84.2% (32), adenovirus 10.5% (4), rhinovirus 15.7% (6), parainfluenza 10.5% (4), and cases of persistent intracellular infections were also observed: Chlamidia pneumonia 15.7% (6), Mycoplasma pneumonia 13.1% (5), i.e. the main etiological data of acute bronchiolitis were consistent with international data.Mixed infection was established in 34.2% (13) of children, while the most common combination was the combination of RS virus with other viral infections (adenovirus, parainfluenza, rhinovirus) detected in 15.7% (6) of children. At the same time, monoinfection with rhinovirus was more often determined in children born prematurely in the first 6 months of life 7.9% (4).Table 2. Etiological structure of acute bronchiolitis
 |
| |
|
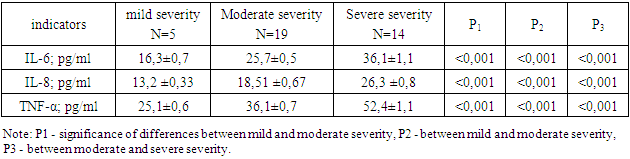
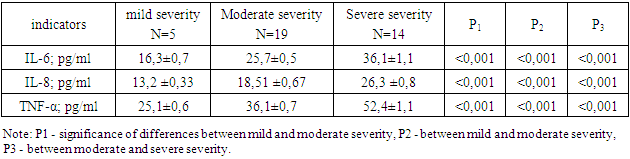
In children 2-6 months of age, there were also cases of acute bronchiolitis caused only by mono-infection in the form of Chlamydia pneumonia 5.2% (2). In 18.4% (7) of children, a combination of RS virus, and atypical flora in the form of Mycoplasma pneumonia and Chlamydia pneumonia was observed.When analyzing the family history of the studied sample of sick children, it was revealed that it was aggravated in 68.4% (26) of the patient, while 42.1% (16) of the children were from large families, while the number of people living in one family exceeded 4, in the family had older children and/or children attending a preschool institution, large families are a regional feature.At the time of admission to the hospital, only 39.4% (15) were breast-fed, 50% (19) were artificially fed, while 15.7% (6) of children were breastfed for only 2 months of life, 7.9% ( 3) children were born from multiple pregnancies, 28.9% (11) were born in the autumn-winter period. Parents of 18.4% (7) of the child smoked, allergic anamnesis was aggravated on the mother's side in 23.6% (9), on the father's side - in 31.5% (12), in 21.05% (8) there were cases of atopic dermatitis.In most patients, the disease began gradually 68.4% (26) and manifested by a deterioration in the general condition (lethargy, loss of appetite), and the appearance of catarrhal phenomena (sneezing, rhinitis, cough). The bulk of the children were admitted on the 3rd-4th day of illness (average 2.81±0.87 days). Appeared and increased shortness of breath, and cyanosis appeared on average at 2.75±0.74 days, which was the reason for going to the hospital. Apnea at the onset of the disease was observed in only 13.1% (5) of children, with the progression of the disease in 7.9% (3), which, along with other indicators, was the reason for the hospitalization of children in the intensive care unit. In the rest of the children, the disease began acutely 31.5% (12).In the majority of 65.7% (25) children, body temperature did not increase, in 28.9% (11) the disease was accompanied by low-grade fever, and febrile fever was registered only in 5.2% (2) of children.The auscultatory picture of the disease was characterized by symptoms of bronchial obstruction - expiratory lengthening 92% (35), dry wheezing 92% (35), moist small bubbling rales 63.1% (24), crepitus 81.6% (31), as well as weakening / asymmetry of breathing 7.9% (3).The severity of the patient's condition was determined by the development of respiratory failure (RF), which was manifested by shortness of breath with the participation of auxiliary muscles in the act of breathing, in severe cases by cyanosis, and was characterized by a decrease in SpO2. In assessing the severity of the condition, we used two methods, the first of them with the determination of SpO2. So, under the classification of respiratory failure S.N. Avdeeva (2007), a decrease in SpO2 to 90-94% was regarded as DN of the first degree 15.7% (6 children), up to 75-89% - DN of the II degree 47.3% (18 children), <75% - DN III degree -36.8% (14 children) [11]. In this regard, 80% (32) of children required oxygen therapy, including 10.5% (4) of children who were on mechanical ventilation.In assessing the severity of acute bronchiolitis, we also used the Acute Bronchiolitis Severity Scale (ESBA), the advantage of this scale over others was the ability to assess the severity of the child's condition from the time of the initial examination, taking into account the respiratory rate and heart rate of the child according to age. According to this scale, the severity of acute bronchiolitis with a score of up to 4 points corresponded to mild severity, 5-8 points of moderate severity, and 9-13 points of severe acute bronchiolitis. The total sample of sick children was distributed as follows: children with mild severity accounted for 13.1% (5), with moderate severity 50% (19), and 36.8% (14) of children constituted the group with severe acute bronchiolitis. At the same time, the average score in the group with severe severity was 11.36 ± 0.34 points, with an average of 6.84 ± 0.21 points and 3.4 ± 0.4 points in the group of children with mild severity of acute bronchiolitis, which was statistically less compared with moderate and severe acute bronchiolitis (p<0.001).Of particular importance in assessing the severity of the condition was the presence of wheezing, which were during exhalation in 92% (35)%, inhalation, and exhalation in 26.3% (10), weakened breathing over the entire surface of the lungs observed in 7.9% (3) children with severe bronchiolitis.Crepitus was mainly observed in the projection of 2-3 lung fields in 28.9% (11), and in 23.6% (9) cases in the projection of 4 fields or more. Also, shortness of breath consisted of retraction of the lower thoracic inlet and retraction of the intercostal spaces 73.6% (28), and in children under 6 months in the swelling of the wings of the nose 15.7% (6).Complete blood count was assessed by indicators of bacterial infection markers, so leukocytosis over 15*109/l was registered in 21.0% (8) of patients, and neutrophilia over 10*109/l - in 13.1% (5). CRP levels over 5 mg/l were recorded in 23.6% (9) of children.Bacterial complications can sometimes complicate the main course of acute bronchitis, so complications were diagnosed in 10 (26.3%) of the observed children and manifested as pneumonia in 10.5% (4) of children and urinary tract infection in 5.2% (2) children, acute enterocolitis in 10.5% (4 children).In an X-ray examination of children with acute bronchiolitis, peribronchial changes and an increase in the pulmonary pattern were observed in 60.5% (23) of children, emphysematous swelling of the lungs in 34.2% (13) of children, areas of hypoventilation in 13.1% (5), manifestations of interstitial edema in 5.2% (2). Atelectasis and segmental infiltration were found in 23.6% (9) of children.All observed children required treatment in a hospital, and 55.2% (22) of them needed treatment in the ICU. At the same time, the condition of children depended on age, the presence of mixed infections, and other risk factors, one of which was prematurity.During the assessment of the therapy of acute bronchiolitis, it was shown that all children received antibacterial drugs 38 children (100%), and 26.3% (10) received combined antibacterial therapy with two drugs at the same time. More often than others, drugs from the cephalosporin group (ceftriaxone, ceftazidime, cefotaxime, cefepime), aminoglycoside series (amikacin, neomycin) were used.In connection with the broncho-obstructive syndrome, 84.2% (32) of children used nebulizer therapy with 3% sodium chloride solution for the treatment, in some patients fulfilling was used. Hormone therapy was prescribed to 100% of children, and only 4 (10.5%) children received only inhaled glucocorticosteroids (IGCS), the remaining 89.4% (34 - systemic steroids (dexamethasone, prednisolone).The total duration of the disease ranged from 6 to 28, and averaged 9.63±0.75 days, taking into account outpatient and inpatient treatment in children of different ages, while the duration of the disease was inversely related to age (r=-0.788; p< 0.01). No lethal outcomes were registered.According to the purpose of our study, we investigated the cytokine status of children with acute bronchiolitis. Such proinflammatory interleukins as interleukin-8 (IL-8), tumor necrosis factor α (TNFα), and interleukin-6 (IL-6) had significant pathological changes. At an average level of IL-8 - 19.12±0.53 pg/ml, IL-6 - 26.01±0.62 pg/ml, TNFα 37.6±1.0 pg/ml. At the same time, the pathological level of interleukins corresponded to the severity of acute bronchiolitis, determined using the ESBA scale. As can be seen from Table 3, the level of IL-8 had a significant difference in the severity of the disease. first of all, macrophages are in the area of inflammation. A similar pattern was also observed for interleukin-6 (IL-6).Table 3. Parameters of cytokines in patients with acute bronchiolitis (M±m)
 |
| |
|
There were no significant differences in the concentration of tumor necrosis factor α (TNFα) in patients with severe acute bronchiolitis in comparison with its moderate course (p>0.05).When matching the etiological factor and the level of interleukins, it was revealed that the highest pathological level was observed when RSV was combined with Chlamydia pneumonia (n=3) (IL-8 - 39.66±0.66 pg/ml, IL-6 - 47, 33±1.20 pg/ml, TNFα 69.0±9.6 pg/ml), while the level of interleukins in mono-infection with RSV (n=19) also remained at a high level, not significantly different from the previous group (IL-8 - 39.021±0.92 pg/ml, IL-6 - 43.68±1.75 pg/ml, TNFα 60.7±3.68 pg/ml).
3. Discussion
Acute bronchiolitis retains a leading place in the structure of the causes of diseases of the bronchopulmonary system in young children for many years [1,2,3,12]. The etiology of acute bronchiolitis in our studies was also dominated by RSV, but there were also cases of chlamydial bronchiolitis, and the combination of RSV with other viruses and chlamydial and mycoplasma infection. Clinical studies have shown that bronchiolitis is most severe in premature babies, children with comorbidities [13]. Basically, all cases of the disease were registered in the autumn-winter period, with a predominance in November and December, which is the epidemic season of RSV infection in a country with a sharply continental climate.For the first time in the region, the Acute Bronchiolitis Severity Scale (ESBA) was used to assess the severity of the condition, which includes such parameters as the nature of wheezing, the presence and extent of crepitus, the nature and severity of dyspnea, respiratory rate and heart rate according to the child's age. This scale is convenient in the early assessment of the condition of a child with acute bronchiolitis, and contributes to early intensive care for the patient. We also noted 100% of the use of antibacterial drugs, which is not recommended for acute bronchiolitis of viral etiology, and is justified only for bacterial complications, which amounted to 26.3% in our studies. At the same time, according to the literature data, the use of antibiotic therapy in severe acute bronchiolitis is justified [14].Tumor necrosis factor and Interleukin-8, interleukin-6 are regulatory proteins that are actively involved mainly in the initial stage of the inflammatory process. They refer to those cytokines that “trigger” a cascade of cytokine reactions that provide an adequate innate nonspecific local and systemic response to the introduction of a foreign agent. Increased production of IFN-α by immunocompetent cells at the site of inflammation occurs almost immediately after the introduction of the virus (after 30-40 minutes), and an increased concentration of this cytokine in the peripheral blood is determined 2-8 hours after the start of the infectious process [8,15,16].We also obtained results characterized by significant activation of interleukins, which depended on the severity of acute bronchiolitis and the etiological factor.
4. Conclusions
The main etiological factor of acute bronchiolitis continues to be RSV in modification (50%), with a high frequency of mixed infection with RSV (34.2%), and modification of Chlamydia pneumonia (5.2%) and rhinovirus (10.5%).The occurrence of acute bronchiolitis occurred against the background of a burdened family history, a short duration of breastfeeding, and atopic diathesis.The use of the ESBA acute bronchiolitis severity scale made it possible to assess the child's condition immediately after the doctor's examination, before the use of instrumental research methods, while it was revealed that the children were mainly admitted with moderate severity of acute bronchiolitis with an average score on the ESBA scale of 6.84.Acute bronchiolitis is characterized by an interleukin expression relationship depending on the severity of acute bronchiolitis, characterized by an increase in the concentration of IL-6 IL-8 and TNFα depending on the severity of the disease. The revealed changes in the content of interleukins can be used as markers for predicting the severity of the course of the pathological process.Patients with mixed infection (RSV and with Chlamydia pneumonia and RSV in modification had higher interleukin profile values.
References
| [1] | Maidannik V.G., Emchinskaya E.A. Modern approaches to the diagnosis and treatment of bronchiolitis in children from the standpoint of evidence-based medicine// Practical medicine. 2013 - 5(74) -S. 7-16. |
| [2] | Baranov A.A. et al. Modern approaches to the management of children with acute bronchiolitis // Pediatric Pharmacology - 2019 - No. 6 (vol. 16) .- P. 339-348. |
| [3] | Shay D.K., Holman R.C., Newman R.D. et al. Bronchiolitis-associated hospitalizations among US children, 1980-1996 // JAMA -1999. -Vol. 282, № 15. - P. 1440-1446. |
| [4] | Meissner H.C. Bronchiolitis. In: Long S.S., Pickering L.K., Prober C.G. Principles and Practice of Pediatric Infectious Diseases. 3nd. New York: Churchill Livingstone, Elsevier. - 2008. - P. 241-245. |
| [5] | Nair H., Nokes J., Gessner B.D. et al. Globalburden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis // Lancet. - 2010. - Vol. 375, № 9725. - Р. 1545-1555. |
| [6] | Gupta S., Shamsundar R., Shet A. et al. Prevalence of respiratory syncytial virus infection among hospitalized children presenting with acute lower respiratory tract infections // Indian J. Pediatr. - 2011. - Vol. 78, № 12. - Р. 1495-1497. |
| [7] | Afanaseva O.I. et al. Indicators of the cytokine status in children with acute respiratory viral infections during therapy with intranasal interferon preparations. Children's infections. 2021 - 20(4) - P.6-12. |
| [8] | Ivanov Yu.V., Shipilov M.V., Ivanov V.V. Cytokines of the early phase of inflammation in patients with acute respiratory infection. Nauchnye Vedomosti. Medical series. Pharmacy. 2011.- No. 16 (111). - S. 140-145. Trushina E.Yu., Kostina E.M., Molotilov B.A., Tipikin V.A.. |
| [9] | Baranova N.I. The role of cytokines IL-4, IL-6, IL-8, IL-10 in the immunopathogenesis of chronic obstructive pulmonary disease // Medical Immunology. - 2019 - No. 1 (21) - S. 89-98. |
| [10] | Rivas-Juesas C, et al. A comparison of two clinical scores for bronchioli-tis. A multicentre and prospective study conducted in hospitalised infants. Allergol Immunopathol (Madr). 2017. http://dx.doi.org/10.1016/j.aller.2017.01.012. |
| [11] | Avdeev S.N. Respiratory failure: definition, classification, approaches to diagnosis and therapy // Respiratory medicine / ed. A.G. Chuchalin. M.: GEOTAR-Media, 2007. T. 2. S. 658–668. |
| [12] | Ralston SL, Lieberthal AS, Meissner HC, et al; American Academy of Pediatrics. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014; 134(5): e1474– 1502. doi: 10.1542/peds.2014-2742. |
| [13] | Krsheminskaya I.V., Ovsyannikov D.Yu., Degtyarev D.N., Degtyarev E.A. Respiratory syncytial viral bronchiolitis in premature infants and predictors of its severe course // Neonatology: news, opinions, training. - 2016 - No. 2 - S. 67-80. |
| [14] | Spurling G.K.P., Doust J., Del Mar C., Eriksson L. Antibiotics for bronchiolitis in children // Cochrane Database Syst. Rev. 2011. Vol. 6: CD005189. |
| [15] | Nagoev, B.S. On the role of cytokines in the regulation of the immune system in infectious diseases / B.S. Nagoev, M.Kh. Nagoeva, E.A. Kambachokova // Proceedings of the III Annual All-Russian Congress on Infectious Diseases (Moscow, March 28-30, 2011). – Infectious diseases. - 2011. - Volume 9. - Appendix No. 1. - M. - 2011. - S. 260. |
| [16] | Simbirtsev, A.S. Interleukin-8 and other chemokines / A.S. Simbirtsev // Immunology. - 1999. - No. 4. - P. 9 - 14. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML