F. Sh. Mavlyanov, F. M. Tukhtaev, Sh. Kh. Mavlyanov, T. F. Shirov
Samarkand State Medical University, Samarkand, Uzbekistan
Correspondence to: F. Sh. Mavlyanov, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
In order to identify the features of the immediate postoperative period, a prospective study was conducted in 30 children with reflux ureterohydronephrosis. The analysis was carried out depending on the correction of vesicoureteral reflux, for this the children were divided into 2 equal groups. Patients of group 1 underwent traditional surgical treatment, group 2 underwent endourological correction. The results of the study showed that the introduction of minimally invasive interventions into surgical practice significantly improves the results of treatment and saves this category of patients from traumatic operations, as well as related complications that occur in the early postoperative period.
Keywords:
Vesicoureteral reflux, Children, Treatment, Postoperative period
Cite this paper: F. Sh. Mavlyanov, F. M. Tukhtaev, Sh. Kh. Mavlyanov, T. F. Shirov, Features of the Postoperative Period in Children with Reflux Ureterohydronephrosis, American Journal of Medicine and Medical Sciences, Vol. 13 No. 5, 2023, pp. 593-595. doi: 10.5923/j.ajmms.20231305.09.
1. Introduction
Currently, various methods of surgical treatment of VUR have been developed, however, all of them do not meet the main trend of pediatric surgery, i.e. achieving recovery with low invasiveness and traumatism with a decrease in the number of complications and relapses.Endoscopic correction with implantation of a binding agent has become the youngest operation in the treatment of VUR, which was first proposed in 1981 by Matouschek E. as an alternative to conservative therapy and open surgery. In the future, the technique was improved and popularized by O'Donnell V. and Puri R., who in 1984 published the results of the introduction of Teflon paste. Since then, thousands of children with VUR have been treated using various implants.The increased interest in this type of treatment was due to a number of its important advantages — low traumatism, short duration of surgery, the possibility of outpatient use, minimal risk of complications characteristic of various reconstructive plastic neoimplantations of the ureters and the absence of the need for prolonged angibiotic therapy.According to various authors, the effectiveness of the endoscopic method varies from 52.4% to 86.7%, so this problem cannot be considered finally solved.
2. Purpose of the Research
To conduct a comparative analysis of the immediate postoperative period in children with reflux ureterohydronephrosis, depending on the method of surgical treatment.
3. Materials and Methods of the Research
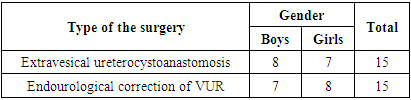
In our work, a comparative analysis of the early postoperative period was carried out in 30 children with congenital urterohydronephro ureterohydronephrosis. Depending on the type of VUR correction, the children were divided into 2 groups (Table 1).Table 1. Types of surgical interventions
 |
| |
|
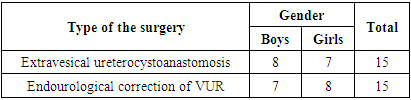
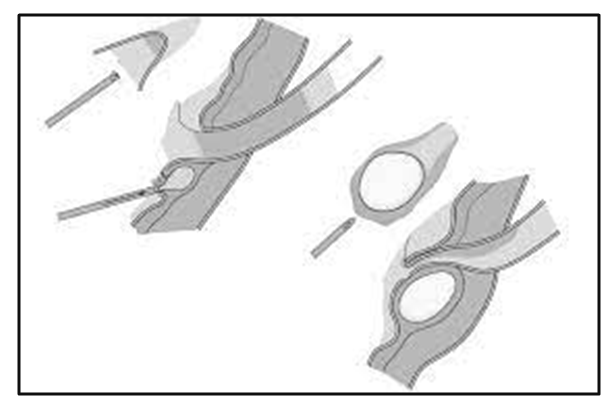
With intravesical discharge of the distal ureters, the main unfavorable factor is the traumatization of the Lieto triangle. In addition, in the area of implantation of the ureter into the bladder, it is necessary to dissect the detrusor with its subsequent suturing over the ureter, and this is what creates the conditions for the formation of a scar in the anastomosis zone. In this regard, the first group included 15 patients who had an extravesical ureterocystoanastomosis without a wide opening of the bladder and who did not have the above disadvantages (Figure 1).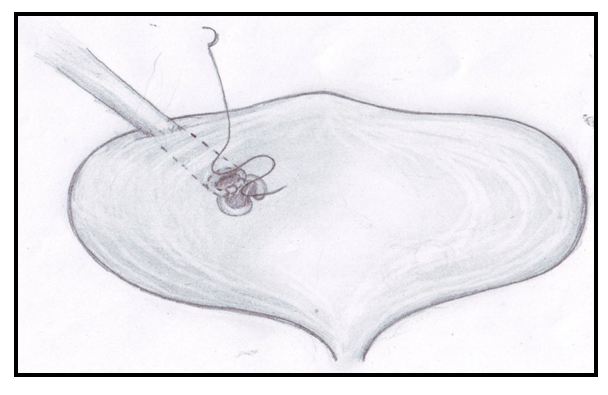 | Figure 1. Scheme of extravesical ureterocystoanastomosis |
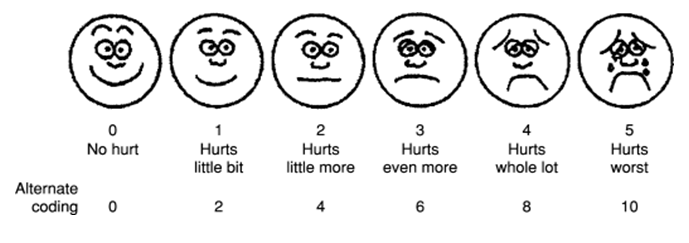
To date, a large number of different methods of surgical correction of VUR have been developed. However, due to the introduction of high-tech methods of treatment, there is a tendency to minimize the traumatism of antireflux operations, reduce the number of complications and relapses. Endoscopic modeling of the ureterovesical anastomosis by implantation of a volume-forming material is a well-known method of eliminating VUR.The second group included 15 patients who underwent endourological correction of VUR (Figure 2). | Figure 2. Endoscopic administration of a volume-forming substance |
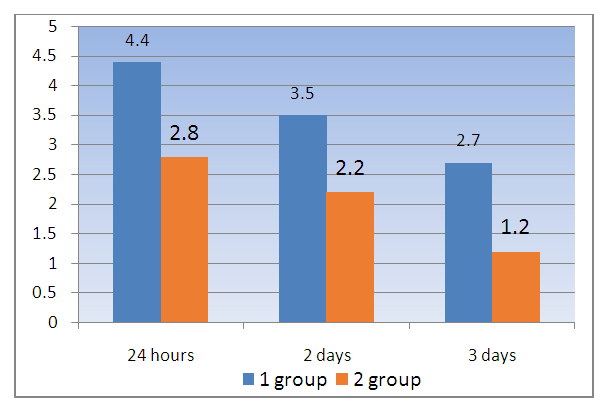
Endoscopic modeling of the ureterovesical anastomosis by implantation of a volume-forming material was performed in a cystoscopic office. The method of anesthesia is general. A cystoscope with a diameter of at least 10 Fr was inserted into the bladder, allowing an injectable flexible endoscopic needle to be inserted through the working channel of the cystoscope. Carrying out the supply of 0.9% sodium chloride solution, cystoscopy was performed. A needle filled with a volume-forming substance was brought to the mouth of the pathological ureter, at the 6 o'clock position of the dial. Mucosal puncture was performed by inserting a needle to a depth of about 1 cm (the length of the metal tip of the needle) at an acute angle to the back wall of the intravesical part of the ureter. Then the opposite end of the needle was connected to an insulin syringe filled with a biopolymer. Visually controlling the area of UVS, the drug was slowly injected (Figure 2).Assessing the severity of the pain syndrome in a child is not an easy, but extremely important task, since therapeutic tactics depend on it. The severity of pain syndrome in the early postoperative period was determined by the Wong-Baker 2008 pain intensity assessment system (Figure 3).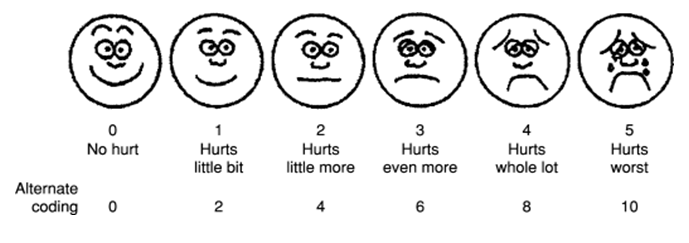 | Figure 3. Wong-Baker scale |
The Wong-Baker faces pain rating scale was created to assess the intensity of pain in children. It includes pictures of faces - a smiling face, which means no pain (0 points out of 5), a distorted grimace of a crying face, which means the greatest pain in intensity (5 points out of 5). The Wong-Baker scale also has a close relationship with the indicators of the visual analog scale and the facial pain scale.
4. Results
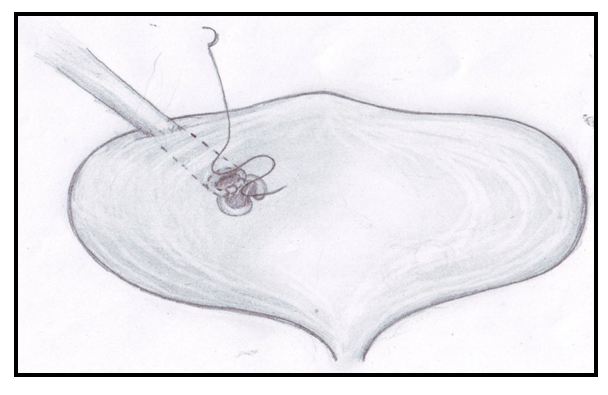
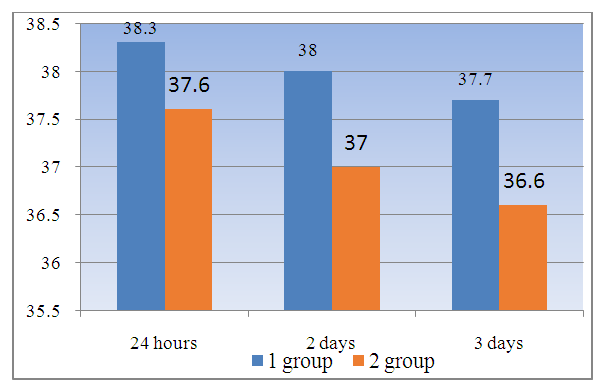
The study was conducted 24 hours later, on the 2nd and 3rd days after the operation. The average score was calculated (Figure 4).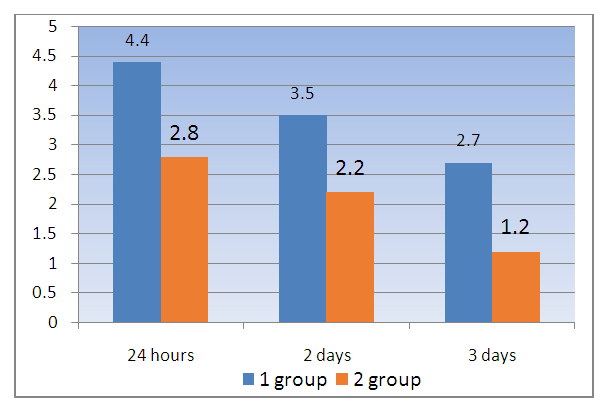 | Figure 4. Average score on the Wong-Baker scale in children with reflux ureterohydronephrosis after surgery |
As can be seen from the diagram, when studying the pain syndrome on the Wong-Baker scale, the average score in children of group 1 24 hours after surgery was 4.3, on day 2 – 3.5 and on day 3, the average score was 2.7. In patients of group 2 who underwent endourological treatment, the pain syndrome was the least pronounced and the average score on the scale was 2.8, 2.2 and 1.2, respectively, for the time intervals of the examination in the immediate postoperative period. Due to the presence of severe pain syndrome in children of group 1, anesthesia with non-narcotic analgesics was performed 3 times a day by intramuscular or intravenous administration. Children of group 2, since the pain syndrome was insignificant, anesthesia was carried out 1-2 times a day with rectal suppositories.Body temperature indicators in the immediate postoperative period in children with reflux ureterohydronephrosis, depending on the treatment method, also had different values.Thus, in children who underwent open (traditional) methods of antireflux protection - ectsravesical ureterocystoneoanastamosis 24 hours and 2 days after surgery, an increase in temperature to febrile values was noted. Only on the 3rd day after the operation, the body temperature of the patients decreased to subfebrile figures (Figure 5).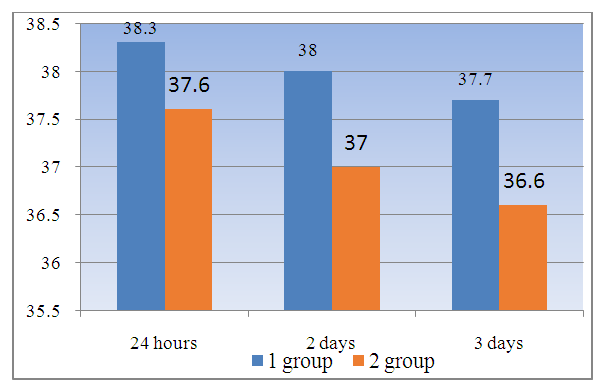 | Figure 5. Body temperature indicators in the immediate postoperative period in children with reflux ureterohydronephrosis |
In the graph presented, it can be noted that in children of group 2, who underwent implantation of a volume-forming material, there was practically no increase in body temperature in the immediate postoperative period.The cancellation of bed rest in group 1 children occurred on the 3-4 day after surgery, when the body temperature normalized and the intensity of pain in the area of the postoperative wound decreased. Catheters inserted into the ureters were removed on 7-8 days, and a Foly-type urethral catheter was removed from the bladder on 8-10 days after surgery. The sutures were removed on the 9th-10th day after surgical treatment. The duration of hospital stay, from the end of the operation to discharge, of patients of these groups varied from 9 to 11 days, on average 9.6 ±0.7 bed days.Cancellation of bed rest in patients of group 2 occurred after 1-2 days, but as a rule, children got up the next day after surgery. The urethral catheter was removed from the bladder on the 3rd day after endourological intervention, the catheter was not installed in the ureters. The duration of hospital stay, from the end of the operation to discharge, of patients of this group varied from 3 to 5 days, on average 3.6 ± 0.6 bed days.
5. Conclusions
The introduction of minimally invasive interventions in the treatment of obstructive uropathies into surgical practice significantly improves the results of treatment and saves this category of patients from traumatic operations, as well as related complications that occur in the early postoperative period. The advantage of the endourological technique of VUR correction is the early activation of patients, as a rule, on the next day after surgery, or on the same day.
References
| [1] | Matouschek E. Urologische Verletzungen [Urologic injuries]. Langenbecks Arch Chir. 1981; 355: 361-4. doi: 10.1007/BF01286871. PMID: 7200174. (In German) |
| [2] | Ainakulov AD, Mavlyanov FSh, Mavlyanov ShKh. Modern treatment of congenital obstruction of the upper urinary tract (literature review). Uzbek Journal of Case Reports. 2022; 2(2): 24–28. doi: 10.55620/ujcr.2.2.2022.5 (In Russ.) |
| [3] | O'Donnell B, Puri P. Treatment of vesicoureteric reflux by endoscopic injection of Teflon. Br Med J (Clin Res Ed). 1984 Jul 7; 289(6436): 7-9. doi: 10.1136/bmj.289.6436.7. PMID: 6428669; PMCID: PMC1442065. |
| [4] | Mavlyanov FSh, Mavlyanov ShKh. Results of surgical treatment of obstructive uropathies in children depending on the level and degree of obstruction. Vestnik of the Immanuel Kant Baltic Federal University. Natural and Medical Sciences Series. 2022; (2). |
| [5] | Shmyrov OS, Vrublevsky SG, Vrublevskaya EN, Vrublevsky AS. Endosurgical interventions in the correction of pathologies of the ureterovesical segment in children. Children's Surgery. 2014; (4): 25-28. (In Russ.) |
| [6] | Capozza N, Patricolo M, Lais A, Matarazzo E, Caione P. Endoscopic treatment of vesico-ureteral reflux: twelve years' experience. Urol Int. 2001; 67(3): 228-231. |
| [7] | Moore K, Bolduc S. Prospective Study of Polydimethylsiloxane vs Dextranomer/Hyaluronic Acid Injection for Treatment of Vesicoureteral Reflux. The Journal of Urology. 2014; 192(6): 1794-1800. |
| [8] | Kaefer M, Misseri R, Frank E, Rhee A, Lee SD. Refluxing ureteral reimplantation: A logical method for managing neonatal UVJ obstruction. Journal of Pediatric Urology. 2014 Oct; 10(5): 824-830. |
| [9] | Kumar R, Puri P. Endoscopic correction of vesicoureteral reflux in failed reimplantated ureter. Eur Urol. 1998; 33(1): 98-100. |
| [10] | Kirsch AJ. Vesicoureteral Reflux. In: Wein AJ, Kavoussi LR, Partin AW, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021: 2341-2365. |
| [11] | Puri P, Kalikiri MK. Vesicoureteric reflux. Indian J Pediatr. 2010; 77(11): 1249-1255. |
| [12] | Routh JC, Inman BA. Vesicoureteral Reflux. In: Wein AJ, Kavoussi LR, Partin AW, Peters CA, eds. Campbell-Walsh Urology. 11th ed. Philadelphia, PA: Elsevier; 2016: 3062-309. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML