-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(5): 586-592
doi:10.5923/j.ajmms.20231305.08
Received: Apr. 14, 2023; Accepted: Apr. 26, 2023; Published: May 12, 2023

The Effectiveness of Staged Surgical Tactics for the Treatment of Complicated Forms of Cholelithiasis in Elderly and Senile Patients
E. A. Rizaev1, Z. B. Kurbaniyazov2, S. E. Mamaradjabov2, Z. N. Nurmurzaev2, F. J. Olimzhonova2
1Tashkent State Dental Institute, Tashkent, Uzbekistan
2Samarkand State Medical University, Samarkand, Uzbekistan
Correspondence to: E. A. Rizaev, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Patients with complicated forms of cholelithiasis account for a significant proportion of hospital admissions, with elderly and senile patients being particularly affected. These patients often experience complications beyond acute inflammation of the gallbladder, such as bile duct lesions and concomitant pathologies, which can exacerbate the severity of the disease. Surgical treatment of complications in this patient group has been challenging, with high rates of septic conditions and mortality. However, advancements in minimally invasive surgical techniques and staged surgical tactics have led to a decrease in mortality and are recognized as effective by most clinicians. Objectifying the severity and prognosis of the disease is crucial for the development of promising treatment approaches, especially for complications such as abdominal and biliary sepsis, which have diverse clinical manifestations. The results of treatment of 171 elderly and senile patients with complicated forms of cholelithiasis are presented. Staged surgical treatment, taking into account the developed criteria for assessing the severity of the condition of patients and the predicted risk of postoperative complications with the use of preliminary minimally invasive decompression interventions on the biliary tract performed in 42.2% of patients of the main group, allowed to stop purulent-cholemic intoxication, improve the results of subsequent radical operations. In 15.6% of patients, these interventions were the final method of treatment. Priority staged use of minimally invasive interventions significantly reduced mortality, postoperative purulent-septic and extra-abdominal complications (3.1%, 12.4% and 29.9%, respectively), whereas in the comparison group these indicators were 8.1%, 32.4% and 41.9%. Elderly and senile patients who underwent simultaneous radical surgical correction for acute destructive cholecystitis or obstructive cholangitis had the highest percentage of mortality, purulent-septic and extra-abdominal complications. Biliary and abdominal sepsis, as well as cardiovascular and pulmonary complications, were the main causes of death. A stage-by-stage surgical treatment approach, using minimally invasive decompression interventions in 42.2% of patients, helped to stop purulent-cholemic intoxication and improve subsequent radical operations. In some cases, these interventions were the final treatment. A therapeutic and diagnostic algorithm based on the prevalence of destructive cholecystitis or obstructive cholangitis clinic allowed for laparoscopic cholecystectomy in 19.6% of patients and mini-laparotomy access in 64.9% of patients. By prioritizing staged use of minimally invasive interventions and optimizing tactical and technical aspects of surgical treatment for elderly and senile patients, mortality and postoperative complications were significantly reduced compared to a comparison group.
Keywords: Cholelithiasis, Complications, Elderly and senile age
Cite this paper: E. A. Rizaev, Z. B. Kurbaniyazov, S. E. Mamaradjabov, Z. N. Nurmurzaev, F. J. Olimzhonova, The Effectiveness of Staged Surgical Tactics for the Treatment of Complicated Forms of Cholelithiasis in Elderly and Senile Patients, American Journal of Medicine and Medical Sciences, Vol. 13 No. 5, 2023, pp. 586-592. doi: 10.5923/j.ajmms.20231305.08.
Article Outline
1. Introduction
- Patients with complicated forms account for 54-65% of the number admitted to hospitals for cholelithiasis (CL). Among the patients operated with acute inflammation of the gallbladder, elderly and senile patients account for up to 30% [1,4,6,7,9]. Along with severe complications of acute inflammation of the gallbladder, lesions of the bile ducts are frequent in patients of older age groups (35-60%). Choledocholithiasis occupies the main place in the structure of bile duct lesions, accounting for 50-78% of all types of pathology [2,3,5,8,10]. In these patients, the severity of the underlying disease is aggravated by concomitant pathology. At the same time, in the acute period of the disease, the effect of mutual aggravation of the underlying and concomitant diseases is manifested.In numerous studies, the results of surgical treatment of elderly and senile patients with complications of CL do not always satisfy specialists, in 40-65% of cases, septic conditions occur in patients, as a result of which from 16.5% to 30.0% of observations end in death [11,12].Objectification of the assessment of the severity of the condition and the prognosis of the disease is of particular importance for the development of promising directions for the treatment of complications of CL as abdominal and biliary sepsis, which is characterized by heterogeneity of clinical manifestations. In recent decades, due to the development of minimally invasive surgical interventions and the introduction of staged surgical tactics, mortality in complicated forms of cholelithiasis in elderly and senile patients has been decreasing. This is mainly due to the development of minimally invasive surgical interventions and the introduction of staged surgical tactics, the effectiveness of which is recognized by most clinicians.
2. Purpose of the Research
- Improving the results of treatment of elderly and senile patients with complicated forms of cholelithiasis by optimizing the tactical and technical aspects of surgical correction with the priority use of minimally invasive interventions.
3. Material and Methods
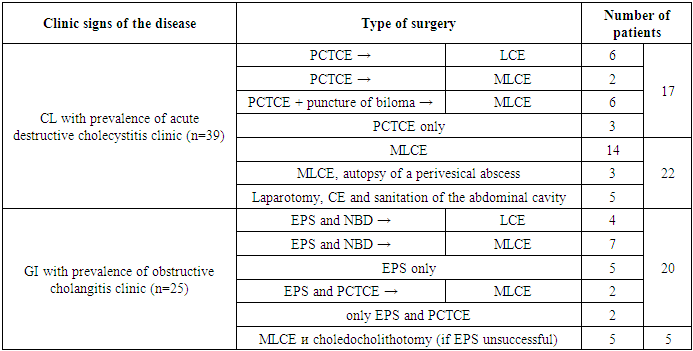
- The results of treatment of 171 elderly and senile patients with complicated forms of GI who were treated in surgical departments of the clinic of the Samarkand State Medical University in the period from 2015 to 2022 are presented. According to the classification adopted by the WHO Regional Office for Europe (2016), elderly patients (60-74 years old) there were 143 (83.6%), elderly patients (75 years and older) – 28 (16.4%). The oldest patient in the study was 87 years old. Female patients prevailed – 104 (60.8%), men – 67 (39.2%). The average age is 64.7±3.4 years, the ratio of women to men is 1.5:1. Of 171 patients with complicated forms of GI, 130 (76.1%) were diagnosed with destructive forms of inflammation of the gallbladder, including 56 - gangrenous cholecystitis. In the structure of complications of bile duct lesions, the main place was occupied by mechanical jaundice, which was observed in 79 patients (44.4%), of which 51 had a total bilirubin content in blood serum exceeding 60 mmol/L.Concomitant pathology was detected in all 171 patients. 135 of them had a combination of 2-3 or more systemic diseases. On average, there were 2.1 concomitant diseases per patient, while in the first age group (60-74 years) - 1.7, and in the second (over 75 years) - 2.4. Diagnosis was carried out on the basis of the clinical picture of the gastrointestinal tract, laboratory and instrumental research methods (sonography, RHG, MR-cholangiography). In accordance with the purpose and objectives of the study, the patients were divided into 2 study groups. The comparison group consisted of 74 (43.3%) patients who were operated on for acute cholecystitis and bile duct lesions for emergency and urgent indications in the period 2015-2018. The main group of the study consisted of 97 (56.7%), in which the algorithm for conducting therapeutic and diagnostic measures according to indications was based on the principles of priority use of surgical treatment methods with the use of minimally invasive surgical interventions. In the study, both groups of patients were identical both in age and in the severity of clinical manifestations and severity of the disease.Of all 74 patients in the control group, 47 (63.5%) had a clinic of acute destructive cholecystitis, and 27 (36.5%) had a clinic of mechanical jaundice and cholangitis due to choledocholithiasis and BDS stenosis. In this group, surgical intervention consisted of performing HE (in 47 patients), or HE with choledocholithotomy (in 27 patients) with external drainage of the choledochus, and surgical intervention was performed from a wide laparotomy access in 33, from a mini–laparotomy access - 41.Factor analysis revealed that the highest percentage of mortality, purulent-septic and extra-abdominal complications (14.8%, 48.1% and 55.6%, respectively) in elderly and senile patients were observed after attempts of simultaneous radical surgical correction of acute destructive cholecystitis or obstructive cholangitis (Fig.1). The cause of mortality was equally biliary and abdominal sepsis, as well as cardiovascular and pulmonary complications.
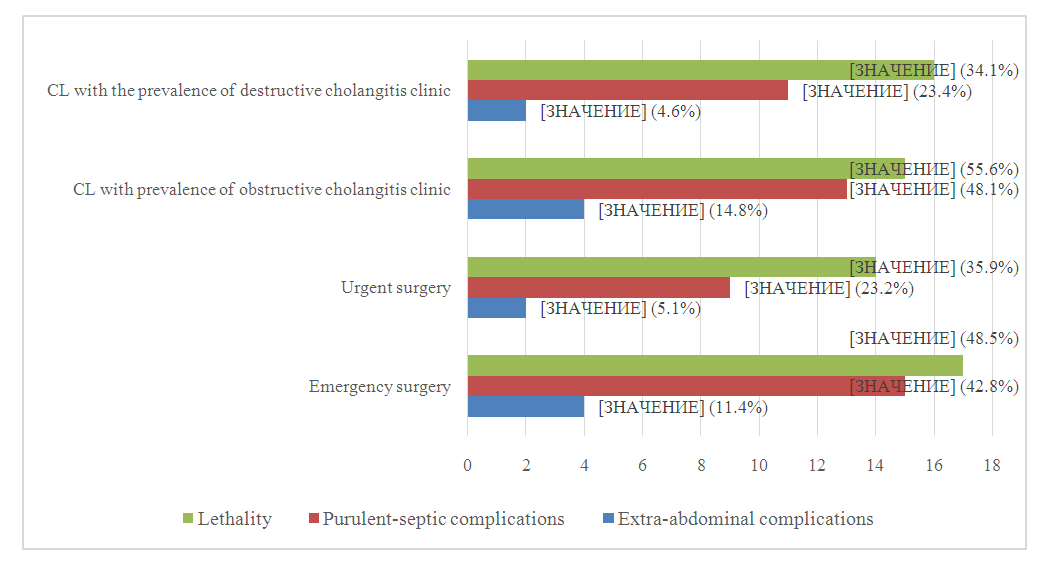 | Figure 1. The frequency of mortality and postoperative complications depending on the urgency of operations and complicated CL clinic in the comparison group in elderly and senile patients |
|
|
4. Results and Discussion
- PCTCE in the surgical treatment of patients with acute cholecystitis, 25 (25.8%) patients of the main study group were treated. Drainage of the gallbladder under ultrasound control was carried out through a section of the liver parenchyma in order to seal the channel and prevent leakage of bile into the abdominal cavity. Drainage in all cases was carried out with an "umbrella" stiletto catheter with a "basket" at the end, with a catheter diameter of 4F and 9F (Fig.2).
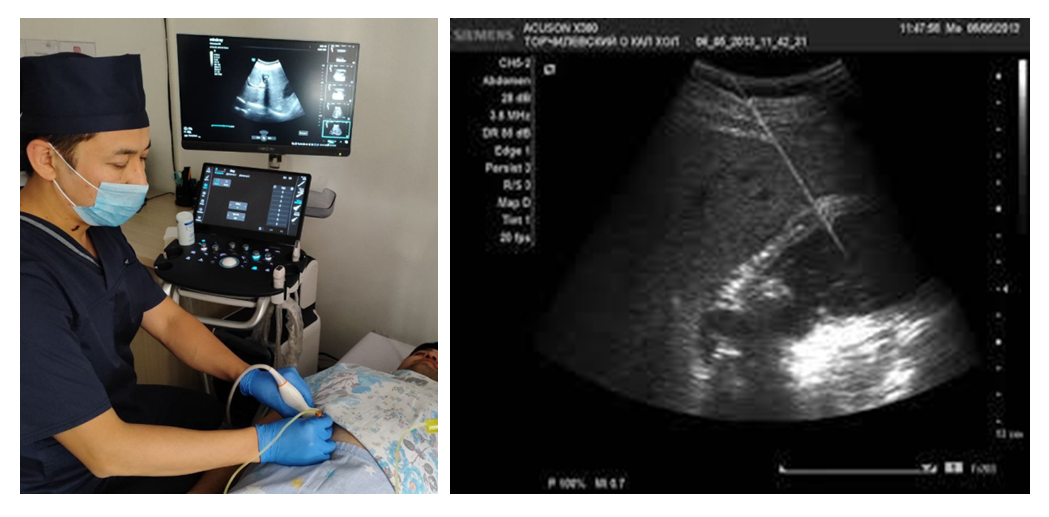 | Figure 2. Percutaneous transhepatic microcholecystostomy under the control of ultrasound scanning |
 | Figure 3. Endoscopic papillosphincterotomy and nasobiliary drainage |
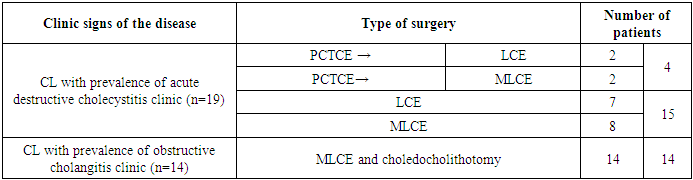
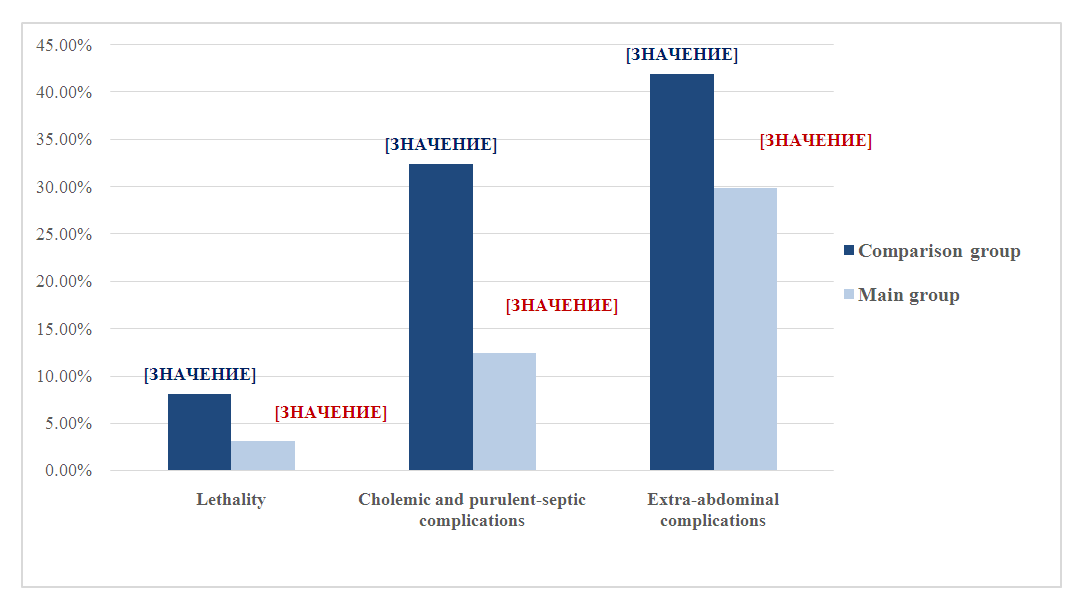 | Figure 4. Results of surgical treatment of elderly and senile patients with complicated forms of CL in comparison groups |
5. Conclusions
- 1. Factor analysis revealed that the highest percentage of mortality, purulent-septic and extra-abdominal complications (14.8%, 48.1% and 55.6%, respectively) in elderly and senile patients were observed after attempts of simultaneous radical surgical correction of acute destructive cholecystitis or obstructive cholangitis. The cause of mortality was equally biliary and abdominal sepsis, as well as cardiovascular and pulmonary complications. 2. Stage-by-stage surgical treatment, taking into account the developed criteria for assessing the severity of the condition of patients and the predicted risk of postoperative complications with the use of preliminary minimally invasive decompression interventions on the biliary tract performed in 42.2% of patients of the main group, allowed to stop purulent-cholemic intoxication, improve the results of subsequent radical operations. In 15.6% of patients, these interventions were the final method of treatment.3. The developed therapeutic and diagnostic algorithm of staged surgical treatment, depending on the prevalence of destructive cholecystitis or obstructive cholangitis clinic using PCTCE under ultrasound guidance, EPS or a combination of them, made it possible to perform cholecystectomy laparoscopically at the subsequent stage of treatment in 19.6% and from the mini-laparotomy access - 64.9%.4. Optimization of the tactical and technical aspects of surgical treatment of elderly and senile patients with complicated forms of GI, taking into account the severity of the patients' condition and the predicted risk of postoperative complications with priority staged use of minimally invasive interventions, significantly reduced mortality, postoperative purulent-septic and extra-abdominal complications (3.1%, 12.4% and 29.9%, respectively), while as in the comparison group, these indicators were 8.1%, 32.4% and 41.9%.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML