Mardieva Gulshod Mamatmuradovna, Turdumatov Jamshed Anvarovich
Samarkand State Medical Institute, Uzbekistan
Correspondence to: Turdumatov Jamshed Anvarovich, Samarkand State Medical Institute, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Today, there is a continuing trend towards an increase in mortality from chronic obstructive pulmonary disease (COPD), which is alarming. Patients with COPD have significant comorbidity. Diabetes mellitus is associated with COPD from 2 to 16%. Concomitant diabetes mellitus accelerates the progression of ventilation disorders and worsens the prognosis, increasing the risk of mortality from COPD. During the research we have examined patients and divide them into 3 groups: 40 patients with combined COPD diabetes mellitus, 20 patients with isolated COPD and 15 patients with diabetes mellitus. Purpose. Determination of clinical, functional and radiological features of COPD in diabetes mellitus, the possibility of predicting its development. Materials and methods. The examined patients were divided into 3 groups: patients with COPD in combination with diabetes mellitus – 40 patients, 20 patients with COPD and 15 patients with diabetes mellitus. Of the X-ray morphological research methods, traditional X-ray and multispiral computed tomography (MSCT) were used, using high-resolution computed tomography parameters. Results. When managing patients with COPD in combination with diabetes mellitus, attention was paid to more pronounced clinical manifestations of respiratory failure compared to patients with COPD. COPD is formed as a result of damage to the small bronchi, which determines the characteristic clinical and radiological symptom complex, and makes it possible to differentiate this disease from emphysema and chronic bronchitis. Diagnostically significant for COPD during computed tomography is a symptom of expiratory air trap, combined with expansion and deformation of bronchi of various sizes, up to broncho- and bronchioectasis. When MSCT in patients with COPD and diabetes mellitus, pathognomic changes characterizing microangiopathy and fibrotic changes. The clear-cut shape of microvessels is a specific X-ray morphological sign in patients with COPD in combination with diabetes mellitus. Conclusions. In the structure of COPD, the pulmonary component and systemic extrapulmonary manifestations, including diabetes mellitus, are distinguished, which can aggravate the disease. The manifestations of diabetes mellitus are based on micro- and macroangiopathies that affect pulmonary microcirculation. In COPD in combination with diabetes mellitus, clinical manifestations of respiratory failure are more pronounced in comparison with patients with COPD.
Keywords:
Chronic obstructive pulmonary disease, Diabetes mellitus, X-ray, MSCT
Cite this paper: Mardieva Gulshod Mamatmuradovna, Turdumatov Jamshed Anvarovich, Features of the Manifestation of Chronic Obstructive Pulmonary Disease in Combination with Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 13 No. 5, 2023, pp. 552-558. doi: 10.5923/j.ajmms.20231305.03.
1. Introduction
Today, there is a continuing trend towards an increase in mortality from chronic obstructive pulmonary disease (COPD), which is alarming. COPD is one of the priority problems in medicine today. COPD is a systemic disease. As the patho-pulmonary process progresses, along with lung damage, pulmonary hypertension, chronic cor pulmonale and significant systemic effects such as cachexia, skeletal muscle atrophy, osteoporosis, anemia, and an increased risk of cardiovascular diseases develop.Many researchers estimate that the current costs of health care and social services in reimbursing the health damage caused by COPD are 30–40 times higher than the costs of preventing them. Such patients need hospitalization, often in intensive care units, in the use of more powerful and expensive antibiotics [9,14]. According to the documents of the European Respiratory Society, only 25% of cases are diagnosed in a timely manner [19,20].According to the definition of COPD, included in the main document on the management of COPD [13,16], the huge role of comorbidities in increasing the severity of COPD, affecting the quality of life, prognosis and survival is emphasized. It should be noted that significant comorbidity is observed in patients with COPD. In modern practice, it is increasingly common to find patients who combine type 2 diabetes mellitus, coronary heart disease, arterial hypertension and COPD [12,17].According to various authors, diabetes mellitus is combined with COPD from 2 to 16% [6]. The pathogenetic mechanisms underlying the high incidence of the combined course of COPD and type 2 diabetes mellitus are being actively studied. Potential mechanisms include: chronic systemic inflammation, oxidative stress, chronic hyperglycemia [1,2,11]. COPD is the 6th leading cause of death in the world, 5th in Europe, and 4th in the United States. The increase in mortality is associated with smoking and population aging. Mortality is significantly higher in patients with COPD hospitalized with an exacerbation against the background of insufficient glycemic control.Special attention is paid to the combination of COPD and type 2 diabetes mellitus. both diseases belong to the second half of life, and according to a number of authors, diabetes mellitus is combined with COPD in 2.0-16.0% of cases [5,6,10]. Concomitant diabetes mellitus accelerates the progression of ventilation disorders and worsens the prognosis, increasing the risk of mortality from COPD [4,16,18]. In general, the important role of comorbid diseases has now been identified. At the same time, the features of X-ray diagnosis of COPD in diabetes mellitus are not well understood.Considering the above, the purpose of our study is to determine the clinical, functional and radiological characteristics of COPD in diabetes mellitus, the possibility of predicting its development.
2. Material and Research Methods
We analyzed the data of a study of 75 patients, among whom there were 46 men and 29 women. A random sample was carried out from an array of patients with established diagnoses of Chronic Obstructive Pulmonary Disease and Diabetes Mellitus. The age of the patients in the main group varied from 25 to 70 years. Patients aged 50 to 65 years predominated.The inclusion criteria were the presence of chronic obstructive pulmonary disease in accordance with GOLD, as well as the presence of diabetes mellitus in accordance with the algorithms of specialized medical care for patients with diabetes.The control group consisted of 10 healthy individuals who did not have lung diseases and diabetes mellitus at the age of 20-40 years: men - 6, women - 4.All patients were divided into 3 groups depending on the characteristics of the course of COPD in combination with diabetes mellitus. The main group I consisted of patients with COPD in combination with diabetes mellitus. In comparison, patients with COPD made up group II and patients with diabetes mellitus - group III (Fig. 1). | Figure 1. Nosological and group characteristics of patients |
The study of patients with COPD was carried out upon admission to the clinic after stabilization of the condition. Patients with diabetes mellitus were examined upon admission to the department or on an outpatient basis.Of the X-ray morphological research methods, traditional X-ray and multispiral computed tomography (MSCT) were used, which was performed on a Light Speed 16 tomograph (General Electric Medical Systems) using high-resolution computed tomography (KTBP) parameters. The scanning step is 1.3 mm, with the reconstruction of sections with a thickness of 1 mm or less.
3. Results
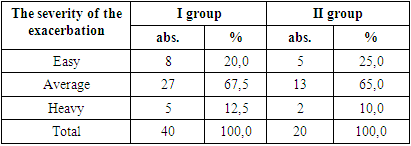
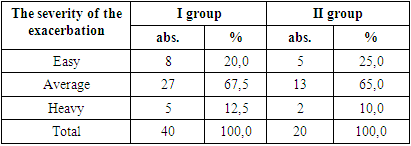
The leading complaints of patients with COPD were shortness of breath, cough, sputum production, chest pain was less often observed in patients with COPD in combination with diabetes mellitus. The decrease in pain sensitivity is most likely associated with patients with diabetic neuropathy. The frequency of exacerbations of COPD 3 or more times a year in group I was observed in 16 (40.0%) patients, in group II - in 3 (15.0%) patients. As can be seen, more frequent exacerbations of COPD were observed in the COPD group with concomitant diabetes mellitus. Strengthening the purulent character of sputum was one of the signs of the severity of the exacerbation. In the examined patients, a mild exacerbation of COPD was revealed in 8 (20.0%) patients of the main group, and in 5 (25.0%) patients of group II (Table 1). The average severity of exacerbation of COPD was detected in 27 (67.5%) patients of the main group and in 13 (65.0%) patients from group II. Severe exacerbation of COPD was determined in 5 patients (12.5%) in group I, and in group II - in 2 (10.0%) patients.Table 1. Characteristics of the severity of exacerbation of COPD
 |
| |
|
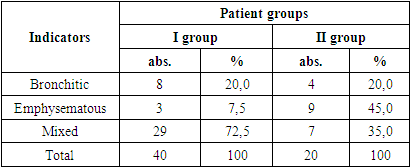
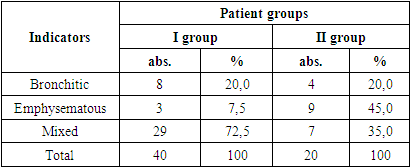
As can be seen from the presented table, depending on the severity of exacerbation of COPD, the data of groups I (main) and II in general did not differ. Analysis of risk factors revealed that patients with COPD smoked more often, followed by frequency of patients with COPD in combination with diabetes mellitus and patients with diabetes mellitus. The duration of COPD was 7.2 ± 0.55 in group I, in group II - 8.2 ± 1.01 years. The duration of diabetes mellitus in patients of the main (I) group was 4.6 ± 1.15 years, in group III - 10.3 ± 0.62 years.Therefore, provided that the severity of COPD in these groups is comparable, one can assume an adverse effect of diabetes mellitus on the development of COPD. Especially considering that diabetes mellitus preceded COPD or was detected simultaneously with COPD in 14 (35%) patients of the main group. And this gives reason to assume the possibility of an adverse interaction between diabetes mellitus and COPD.The participation of auxiliary muscles in respiration was observed in 14 (35%) patients of the main group, in group II - in 2 (10%) patients. That is, the work of breathing in patients with COPD in combination with diabetes mellitus was higher. In addition, severe shortness of breath and cough were more often observed in the main group.The study of the incidence of clinical forms of COPD revealed the following features. Thus, the emphysematous type of COPD was more common in group II. The main group was dominated by patients with mixed type of COPD (Table 2).Table 2. Characteristics of the types of COPD
 |
| |
|
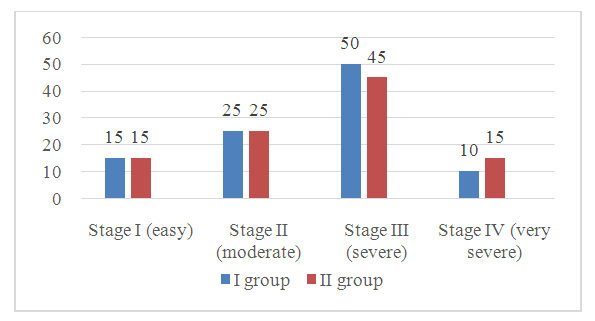
It is known that the emphysematous form is prognostically more favorable, since the decompensation of cor pulmonale occurs at a later stage in comparison with the bronchitic form of COPD.The study of the results of the study of laboratory parameters of blood showed that groups I and II did not differ in terms of indicators of a general blood test, levels of total blood protein, fibrinogen. The blood glucose level was increased in the COPD group with concomitant diabetes mellitus (7.1 ± 0.33 mmol / L) compared to patients with COPD (4.3 ± 0.12 mmol / L). The fasting blood glucose level in patients III averaged 12.5 ± 0.99 mmol / L.Comparison of indicators of the stage of COPD showed that in the main (I) group, the mild stage of the course of COPD was detected in 6 (15.0%) patients, the moderate stage of the course - in 10 (25.0%), the severe stage of the course - in 20 (50, 0%) and a very severe stage of the course - in 4 (10.0%) patients (Fig. 2). A similar distribution was observed in group II. Consequently, the main and comparison group I were randomized according to the stage of COPD.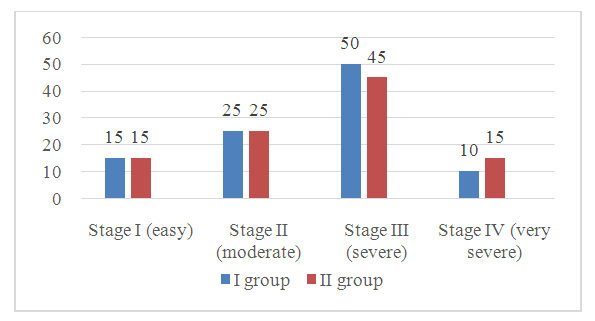 | Figure 2. Distribution of patients depending on the stage of the course of COPD |
According to a clinical study, respiratory failure I was detected in 5 (12.5%) patients in group I, and in 8 (20.0%) patients in group II (Table 3). Respiratory failure of the II degree was revealed in 20 (50.0%) patients of the I group and 9 (45.0%) patients of the II group. Respiratory failure of the III degree was noted in 9 (22.5%) patients of the main group and in 8 (20.0%) of the II group. That is, according to the data of clinical examination, respiratory failure developed with the same frequency in both groups.Table 3. Clinical characteristics of respiratory failure
 |
| |
|
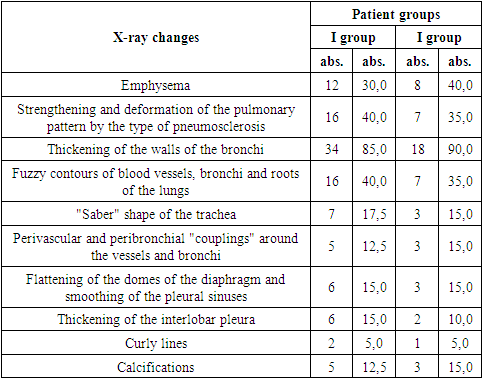
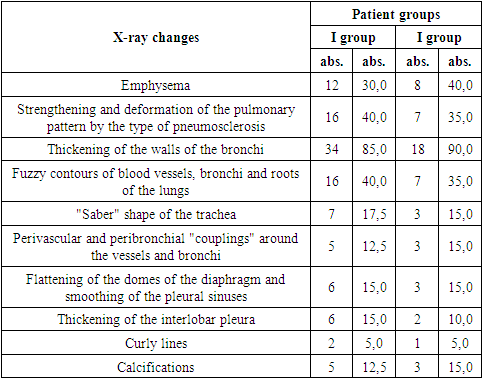
The study of the peculiarities of respiratory failure depending on PaO2 showed that PaO2 60-79 mm was regarded as the I degree of severity, 40-59 mm - as the II degree of severity, <40 mm - as the III degree of severity. Respiratory failure was detected in 39 (97.5%) patients of the main (I) group, which was 22.5% more often than in group II - in 15 (75.0%) (Table 3). Thus, grade I respiratory failure was detected in 24 (60.0%) patients of the main group and 12 (60.0%) patients from group II. Respiratory failure of the II degree was revealed in 12 (30.0%) patients of the main group, which was 20% more often than in the II group - in 2 (10.0%) patients. Respiratory failure III was determined in 3 (7.5%) patients of the main group and in 1 (5.0%) patient from group II. Consequently, respiratory failure depending on PaO2 was more common in patients with COPD in combination with diabetes mellitus.Radiation examination of patients began with traditional plain radiography. All radiographs of the lungs were performed at inspiratory height, with holding the breath. The most characteristic radiological signs of obstruction in the lungs were: increased airiness of the lung tissue in the expiratory phase due to the excess air content in the respiratory parts of the lungs (30% in group I, 40% in group II); flattening of the domes of the diaphragm and smoothing of the pleural sinuses (15% each in both groups); the vertical position of the axis of the heart on the general X-ray of the chest organs in direct projection (heart shadow of "small" size or the so-called "drop" heart); "Saber" shape of the trachea - the predominance of the sagittal (anteroposterior) size of the trachea, determined from the lateral radiograph, over the transverse size, measured from the radiograph in frontal projection (17.5% and 15%, respectively).In addition, the plain chest X-ray in patients with COPD revealed: strengthening and deformation of the pulmonary pattern in the hilar and supraphrenic parts of the lungs by the type of pneumosclerosis (40% and 35%, respectively); thickening of the walls of the lobar and segmental bronchi (85% and 90%, respectively); indistinctness of the contours of blood vessels, bronchi, as well as "blurred" structure of the roots of the lungs.Evaluation of the results of X-ray examination did not reveal significant differences in the assessment of the lung parenchyma in groups I and II of the examined patients (Table 4).Table 4. Frequency of detection of radiological signs of lesion in COPD
 |
| |
|
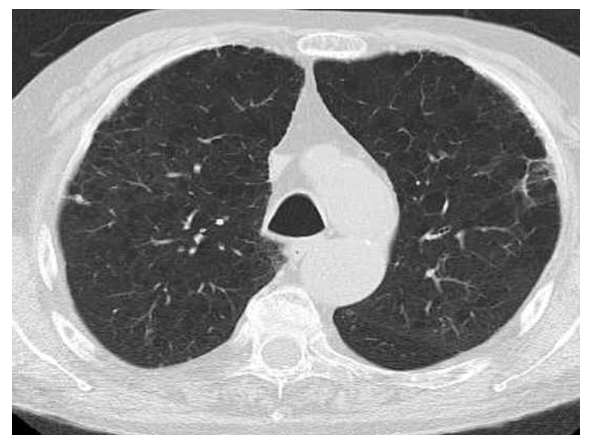
Assessment of the state of the mediastinal shadow during radiography in patients with COPD revealed its own characteristics. Due to the overload of the right ventricle in COPD, the examined patients showed some change in the configuration of the mediastinal shadow on the roentgenogram. Due to the increase in pressure in the pulmonary circulation, the large branches and the main trunk of the pulmonary artery expand, respectively, the second arc of the left contour of the cardiovascular shadow is lengthened and made more convex. With increasing load, the right ventricle expands, so the lower arch of the right contour is shifted to the right, and the atriovasal angle is upward. Changes in the heart caused by a chronic pulmonary process in the lungs are known to have received the general name "cor pulmonale" [3]. In patients with COPD, included in groups I and II, during X-ray examination in the prevailing percentage of our observations, the configuration "cor pulmonalis" was noted.A similar clinical symptomatology in patients with various pathological changes in the lungs created significant difficulties in the differential diagnosis of COPD with chronic bronchitis and emphysema, as well as in assessing the severity of COPD. This circumstance served as the basis for the study of additional possibilities of computed tomography (CT) in the diagnosis of COPD in order to increase the efficiency of radiation research methods (Fig. 3).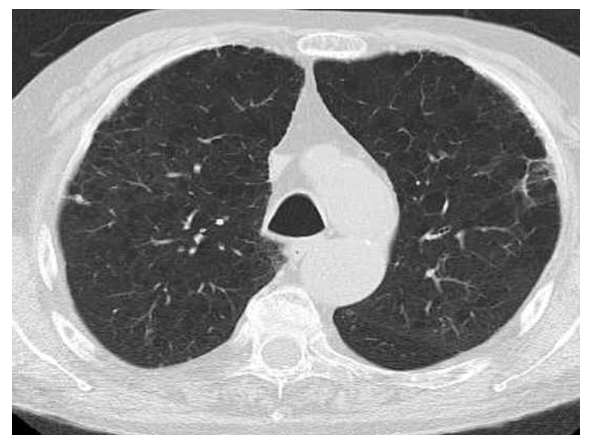 | Figure 3. Patient H., 68 years old. Computed tomogram in the axial plane. In the lung tissue, centrilobular emphysema is determined on both sides |
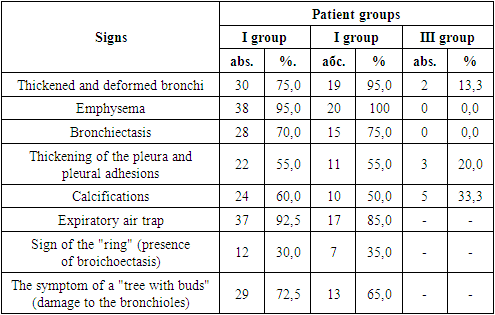
The results of a detailed analysis of X-ray morphological changes in patients with COPD and diabetes mellitus using CT are presented in Tables 5 and 6. All analyzed data were divided into two groups. The changes included in group 1 included signs that were characteristic of COPD and the postponed inflammatory process in the lungs: thickened and deformed bronchi, emphysema, bronchiectasis, pleural thickening and pleural adhesions, intrapulmonary calcifications. The changes included in group 2 included the signs of microangiopathy: dilated vessels of the parenchyma, including focal-like shadows of vascular origin, 2-5 mm in size; clear vasodilation.MSCT of the lungs using functional breathing tests (inspiratory and expiratory phases) made it possible to detect early signs of COPD development already at the preclinical stage of the disease, even under the condition of normal parameters of external respiration function. When using CT in the expiratory phase, the majority of patients with COPD in groups I and II revealed the presence of air "traps" in the lungs, a symptom of a "tree with kidneys", indicating changes at the level of small bronchi.Emphysema and bronchiectasis were found in groups I and II and were absent in patients in group III (Table 5). Pleural thickening, pleural adhesions, calcifications were detected in all three groups. Thickened and deformed bronchi were detected in 30 (75.0%) patients of the main group and 18 (90.0%) patients in group II. In group III, thickening and deformation of the bronchi occurred in 2 (13.3%) patients, which was significantly less common in comparison with groups I and II. Therefore, this symptom was typical for patients with COPD in combination with diabetes mellitus and without diabetes mellitus.Table 5. CT scan - symptoms characteristic of COPD and previous pneumonia
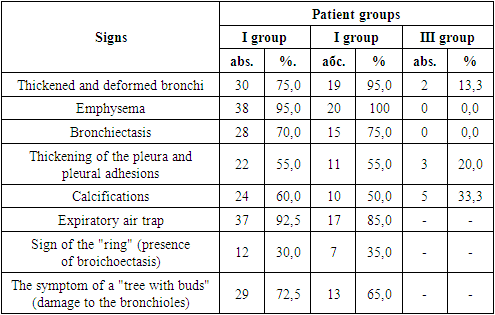 |
| |
|
CT symptoms of changes in the pulmonary parenchyma, such as an expiratory air trap, a sign of a ring (presence of bronchiectasis), a symptom of a tree with kidneys (damage to bronchioles) were pathognomical for patients with COPD from groups I and II.Dilated vessels of the parenchyma and focal-like shadows of vascular origin with a diameter of 2-5 mm were equally common in all compared groups (Table 6). However, in patients with COPD, these signs were combined with thickening and deformation of the bronchi, bronchiectasis, emphysema and were a consequence of COPD and the inflammatory process. In patients of group III, thickened and deformed bronchi, emphysema and bronchiectasis were not found.Table 6. CT - symptoms characteristic of microangiopathy
 |
| |
|
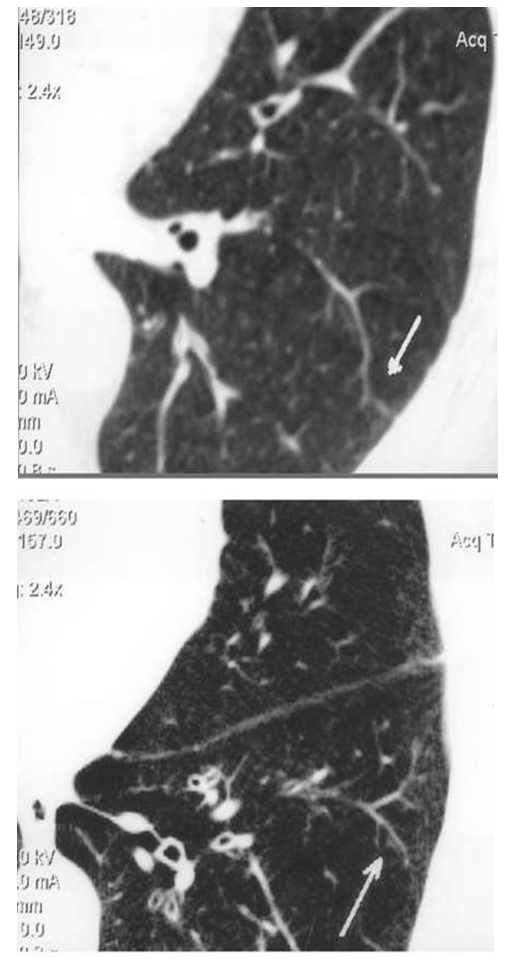
Consequently, in patients with diabetes mellitus, vasodilation of the parenchyma and vascular foci-like shadows of small diameter can be considered as a manifestation of diabetic angiopathy (Fig. 4). In patients with COPD, this symptom is due to the development of fibrosis. A clear-cut shape of the vessels was detected in 38 (95.0%) patients in group I and in 8 (40.0%) patients in group II. In group III, this sign was detected in 14 (93.3%) patients, which was 53.3% more often than in group II.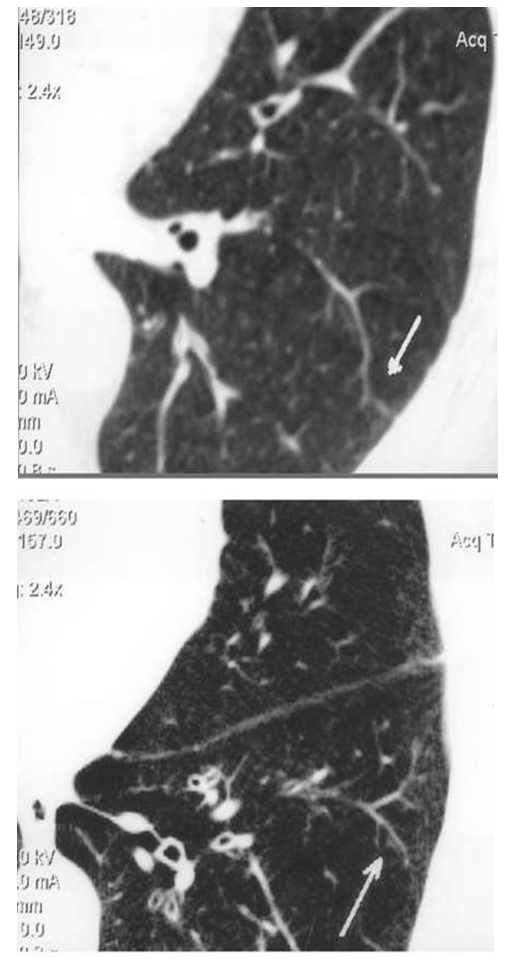 | Figure 4. MSCT of patient B. 59 years old. The arrow indicates an enlarged deformed vessel in the parenchyma of the VIII segment of the left lung |
Consequently, a clear-cut shape of the vessels was characteristic of patients with COPD in combination with diabetes mellitus and patients with diabetes mellitus. That is, a clear-cut shape of blood vessels is more common in patients with COPD in combination with diabetes mellitus in comparison with patients with COPD, which indicates an unfavorable effect of diabetes mellitus on the state of microcirculation in COPD.
4. Discussion of Research Results
The incidence of cyanosis in the study of the main manifestations of respiratory failure did not differ in groups I and II. The participation of auxiliary muscles in respiration was more often observed in the main group. Dyspnea in patients of the main group was more pronounced than in the comparison group. In general, in the main group, respiratory failure, revealed by clinical and laboratory-instrumental methods, was more pronounced than in group II. The severity of shortness of breath did not depend on the stage of the course of COPD and prevailed in the main group.Summarizing our discussion, we can say that in the structure of COPD there is a pulmonary component and systemic manifestations that can aggravate the disease. The extrapulmonary effects of COPD include diabetes mellitus. The manifestations of diabetes mellitus are based on micro- and macroangiopathies that affect pulmonary microcirculation. When managing patients with COPD in combination with diabetes mellitus, one should pay attention to more pronounced clinical manifestations of respiratory failure (shortness of breath, participation in breathing of auxiliary muscles, hypoxemia), especially in patients with stage III COPD in patients with COPD.Standard X-ray examination did not reveal pronounced differences between the examined groups of patients with COPD. The variety of different broncho-pulmonary diseases with similar clinical symptoms makes it extremely difficult to carry out the differential diagnosis of COPD. In this regard, there is a need to identify objective diagnostic criteria that can be obtained using X-ray and computed tomography studies. COPD is formed as a result of damage to the small bronchi, which determines the characteristic clinical and radiological symptom complex, and makes it possible to differentiate this disease with emphysema and chronic bronchitis.To diagnose microvascular lesions in patients with COPD and diabetes mellitus, to predict the course of nonspecific lung diseases, based on the specific results of the study, it is advisable to carry out multispiral computed tomography with the detection of dilated parenchymal vessels, focal-like shadows of vascular genesis with a diameter of 2-5 mm, and a well-shaped vessel shape. Signs of the development of macro- and microangiopathy in patients with COPD in combination with diabetes mellitus is hypoxemia. Lung microangiopathy is likely to play a decisive role in the unfavorable course of COPD in patients with diabetes mellitus.
5. Conclusions
In patients with COPD, assessment of the degree of impaired ventilation in the lungs should be carried out in conditions of CT performed in the inspiratory and expiratory phases. Diagnostically significant for COPD during computed tomography is a symptom of expiratory "air trap", combined with expansion and deformation of bronchi of various sizes, up to broncho- and bronchioectasis. In MSCT, patients with COPD and diabetes mellitus have pathognomonic changes characterizing microangiopathy and fibrous changes: dilated parenchymal vessels, foci-like shadows of vascular genesis with a diameter of 2-5 mm, a clear shape of the vessels. The clear-cut shape of microvessels is a specific X-ray morphological sign in patients with COPD in combination with diabetes mellitus.
References
| [1] | Budnevsky A.V. et al. Diagnostic value of biomarkers of systemic inflammation in chronic obstructive pulmonary disease // Clinical Medicine. - 2014. - T. 92. - No. 9. - S. 16-21. |
| [2] | Vertkin A.L. Comorbidity in chronic obstructive pulmonary disease: the role of chronic systemic inflammation and clinical and pharmacological niches of roflumilast // A.L. Vertkin, A.S. Skotnikov, O. M. Gubzhokova. - Therapist. - 2013. - No. 9. - S. 34-39. |
| [3] | Korolyuk I.P., Lindenbraten L.D. Radiation diagnostics. Moscow "BINOM" - 2017. - P. 496. |
| [4] | Lyubavina N.A. The influence of type 2 diabetes mellitus on the clinic, the immune response and microbiocenosis of the respiratory tract in patients with obstructive diseases: author. dis. ... Cand. honey. sciences. N. Novgorod, 2011. |
| [5] | Russian Respiratory Society: Federal Clinical Recommendations for the Diagnosis and Treatment of Chronic Obstructive Pulmonary Disease / A.G. Chuchalin et al. // Pulmonology. - 2014. - No. 3. - S. 15-54. |
| [6] | Samorukova E.I. Malinicheva Yu.V., Zadionchenko B.C. Obesity and metabolic disorders in patients with chronic obstructive pulmonary disease: the possibilities of phenotyping. Pulmonology. 2014; 5: 32-38. |
| [7] | Tatarkina N.D., Tatarkin A.A. Pathogenetic bases of the comorbid course of chronic obstructive pulmonary disease and hypertension. Health. Medical ecology. The science. 2013. T. 51. No. 1. S. 33-37. Blanc PD. Occupation and COPD: a brief review. J Asthma. 2012 Feb; 49(1): 2-4. |
| [8] | Comorbidity between chronic obstructive pulmonary disease and type 2 diabetes: A nation-wide cohort twin study / H. Meteran, V. Backer, K.O. Kyvik // Respir Med. 2015 Aug; 109(8): 1026-1030; The prevalence of diabetes mellitus in copd patients with severe and very severe stage of the disease / J. Stojkovikj, B. Zafirova-Ivanovska, B. Kaeva et al. // Open Access Maced J Med Sci. 2016. Vol. 15; 4(2): 253-258). |
| [9] | Couillard A. Comorbidities in COPD: a new challenge in clinical practice / A. Couillard, D. Veale, J.F. Muir // Rev Pneumol Clin. – 2011. – Vol. 67. – № 3. – P. 143-53. |
| [10] | Diabetes among outpatients with COPD attending a university hospital / P. Rogliani [et al.] // Acta Diabetologica. – 2014. – Vol. 51. – № 6. – P. 933-40. |
| [11] | Global Strategy for the Diagnosis, Management and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD) (Updated 2018). [Electronic resource]. URL: http://goldcopd.org/. Access: 11.05.2018. |
| [12] | Global Initiative for Chronic Obstructive Lung Disease, GOLD, 2016. |
| [13] | Ibatova, S.M., Mamatkulova, F.K., Ruzikulov, N.Y. The clinical picture of acute obstructive bronchitis in children and the rationale for immunomodulatory therapy (2020) International Journal of Current Research and Review, 12 (17), pp. 152-155. |
| [14] | Miller J., Edwards L.D., Agusti A., Bakke P., Calverley P.M., Celli B. et al. Comorbidity, systemic inflammation and outcomes in the ECLIPSE cohort. Respir Med. 2013. № 107. Р. 1376-1384. |
| [15] | Okboev, T.A., Dusanov, A.D., Yuldasheva, D.A., Zakiriayeva, P.O. Distribution of alleles and genotypes of Noesg 3 genes polymorphism among individuals with bronchial asthma in the Uzbek family (2020) European Journal of Molecular and Clinical Medicine, 7 (1), pp. 3430-3441. |
| [16] | Ibatova, S.M., Mamatkulova, F.Kh., Abdukadirova, N.B., Rakhmonov, Y.A., Kodirova, M.M. Risk factors for development of broncho-ostructive syndrome in children (2020) International Journal of Current Research and Review, 12 (23), pp. 3-6. |
| [17] | Parappil A., Depczynski B., Collett P., Marks G.B. Effect of comorbid diabetes on length of stay and risk of death in patients admitted with acute exacerbations of COPD. Respirology. 2010. № 15. Р. 918-922. |
| [18] | Turdumatov Zh.A., Mardieva G.M. Aspects of verification of radiation diagnostics of chronic obstructive lung disease. Евразийский Союз Ученых (ЕСУ) 3(72), 2020. C43-45. |
| [19] | Turdumatov, J., Mardieva, G. Clinical and x-ray peculiarities of the course of chronic obstructive pulmonary disease in combination with diabetes mellitus (2020) European Journal of Molecular and Clinical Medicine, 7 (2), pp. 3009-3028. |




 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML