-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(4): 540-543
doi:10.5923/j.ajmms.20231304.40
Received: Apr. 14, 2023; Accepted: Apr. 25, 2023; Published: Apr. 28, 2023

The Use of Minimally Invasive Interventions in the Treatment of Liver Abscesses
B. D. Babadjanov, К. J. Matmurotov, U. I. Pulatov, S. Sh. Yakhshibaev
Department of General Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: К. J. Matmurotov, Department of General Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

To date, despite various newly developed methods of surgical treatment for purulent liver diseases, the frequency of purulent complications and mortality remains high. In this study, the results of treatment for 31 patients with liver abscesses who underwent minimally invasive surgical interventions were analyzed. Along with drainage of the purulent cavity of the liver, patients simultaneously underwent long-term catheter therapy with catheterization of their own renal artery. Using this strategy, we managed to achieve favorable clinical outcomes in a short time.
Keywords: Liver abscess, Minimally invasive, Catheter therapy
Cite this paper: B. D. Babadjanov, К. J. Matmurotov, U. I. Pulatov, S. Sh. Yakhshibaev, The Use of Minimally Invasive Interventions in the Treatment of Liver Abscesses, American Journal of Medicine and Medical Sciences, Vol. 13 No. 4, 2023, pp. 540-543. doi: 10.5923/j.ajmms.20231304.40.
Article Outline
1. Introduction
- In recent decades, there has been a clear upward trend in the frequency of liver abscesses. Hepatic abscesses are not rare and their frequency in hospitalized patients reaches from 0.5 to 2–3% [4,10,15]. Liver abscess is a severe polyetiological disease, and the causes of liver abscess are most often purulent inflammatory diseases of the abdominal organs, postoperative complications, cyst and hematoma suppuration, and liver neoplasm.According to researchers, the following factors can be distinguished in the origin of liver abscesses: laparotomy in the nearest anamnesis - 51.3% of the total number of patients, cholangiogenic - 18.5%, infected hematomas -6%, suppurative cysts - 2%, idiopathic - 22.2% [3,5,8]. According to most researchers, the lethality of microbial abscesses is high and is from 20 to 30%, while amoebic and opisthorous abscesses have a 26% and 15.5% lethality, respectively [11].Lethality in multiple liver abscesses is significantly higher than in single ones and may reach, according to some authors, 50-90% [1,14]. When treating multiple small bacterial liver abscesses, a technique of long-term intraportal infusion antibiotic therapy has been developed at the clinic, as the draining and opening of such abscesses are technically difficult and not always efficient [7].In these cases, one can only hope for conservative treatment. It is obvious that treatment will be more successful with the introduction of drugs directly into the liver vascular bed. According to some authors, the intraarterial introduction of medicines has several advantages, namely: the high concentration of their lesions in the unchanged form, a short way of delivery of drugs to the hearth defeats [2,12].According to A.L. Levchuk and V.F. Zuberitsky, supplement surgical interventions Regional intraarterial administration of drugs capable of effectively affecting various cell metabolic links, largely improves treatment outcomes. At the same time, the fastest and most stable clinical effect is noted in the regional intraarterial application of multi-component antihypoxants-based solutions [6,9]. Since the drugs have 3 antihypoxanth and antioxidants that are able to purposefully correct hypoxic disorders in tissues, their use by regional introduction leads to the conclusion that the pathogenetic validity of this path is the high introduction [6].In recent years, despite many published materials and research aimed at improving the results of surgical treatment of patients with liver abscess, there is no single standard or algorithm of treatment tactics that determine the outcome of the disease in each individual case, depending on the localization of the pathological hearth [13,16]. In this regard, the purpose of our research was to improve the surgical treatment of patients with liver abscesses using mini-invasive methods.
2. Material and Methods
- This study analyzed the results of the treatment of 31 patients with liver abscesses of different etiology and localization who received inpatient treatment at the Department of Purulent Surgery and Surgical Complications of Diabetes Mellitus at the Multidisciplinary Clinic of the Tashkent Medical Academy from 2016 to 2021. Among them, 17 were women and 14 were men aged between 27 and 69. In 4 (12.9%) patients, the cause of abscess formation was infection from a post-traumatic hematoma, while in 5 (16.1%) cases, parasitic cyst suppuration was diagnosed. Hepatic cholangiogenic abscesses were present in 17 (54.8%) patients, and only in 3 cases (9.6%) was there a purulent process in the liver after the initial operation (residual cavities). Liver metastatic abscesses were found in 2 (6.4%) patients with identified primary sources.In addition to general clinical examinations, all patients underwent multislice computed tomography (MSCT) of the abdominal cavity to determine the surgical treatment tactics. Based on the examination results, a surgical plan was developed for each patient. In cases where there were no clinical signs of an obvious inflammatory process, the purulent abscess was drained first, followed by whole-liver perfusion chemotherapy (WCL). The duration of this procedure ranged from 3 to 6 days, depending on the stage of the inflammatory process. In our practice, a minimally invasive surgery (percutaneous puncture) was performed during the second stage of the WCL procedure, which led to favorable results in all cases.During the drainage of the pathological site, material was taken for bacteriological research, and adequate antibacterial treatment was initiated based on the results. Patients received infusion and empirical antimicrobial treatment prior to the resulting therapy.
3. Result and Discussion
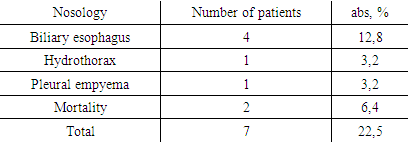
- In the absence of emergency indications for laparotomy, minimally invasive methods of treatment were used, and 23 (74.1%) out of 31 patients underwent percutaneous venting of liver abscesses on the second day of inpatient treatment. Eight (25.8%) patients had multiple small and septic episodes of abscess in the liver. These abscesses always pose a real threat to the lives of patients, since the usual surgical intervention consists of opening each pustule. However, it is not always possible to perform an ultrasound-controlled puncture and venting due to a large number of abscesses and their small size.All patients underwent intra-arterial catheterized antibiotic therapy via the celiac trunk as the main and only method for complex treatment, as in this situation one had to rely only on it in view of creating a maximum concentration of the drug. On the second day after catheterization of the celiac trunk, a control ultrasound of the abdominal cavity was performed in 3 patients, and percutaneous drainage of the liver cavity was performed due to the formation of a unified cavity. All 8 patients were discharged for outpatient treatment and recovered. This indicates the possibility of using intraarterial catheter therapy as an independent method of treatment in patients with multiple small and miliary liver abscesses, in which the prognosis is considered to be extremely poor.All surgical interventions with ultrasonically assisted drainage of the purulent cavity were performed in 22 (84.6%) patients with a single liver abscess and 4 (15.3%) patients with two or more lesions. Simultaneous emptying of the abscess using percutaneous drainage and catheterization of the celiac trunk was performed in 8 (25.8%) patients. When evacuating the contents of the abscess, the material was sent for cytological and bacteriological study, after which drainage sanitation of the abscess cavity was performed. Analysis of the data revealed that pyoinflammatory liver disease in 12 (38.7%) patients appeared after primary liver surgery. Residual purulent liver abscesses were observed in 19 (61.3%) patients (Figure 1).
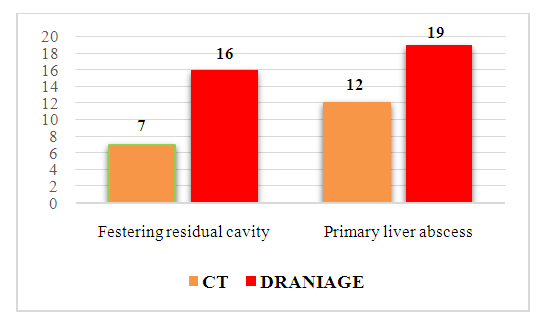 | Figure 1. Characteristics of the surgical interventions |
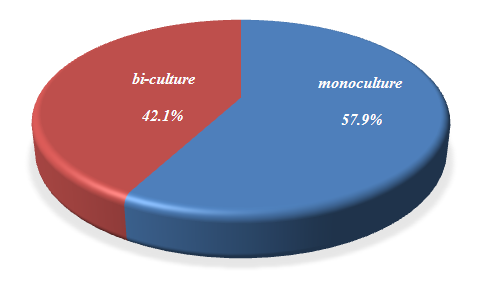 | Figure 2. Results of the bacteriological examination |
|
4. Discussion
- Nowadays, the number of patients with liver abscesses is increasing. It is crucial to diagnose them at an early stage and treat them with minimally invasive methods, as the mortality rate of patients with this disease is very high, and the complications can be severe and even fatal. Given the above indicators, it is important to perform individual bacteriotherapy through a catheter inserted into the celiac trunk and drain a purulent focus in the liver. However, a difficult task for surgeons when handling patients with pyoinflammatory liver diseases (abscesses) is to determine the risk of developing purulent peritonitis when choosing minimally invasive treatments. In such cases, attention should be paid to the presence of diabetes, liver cirrhosis, pronounced body intoxication, etc., which directly affect the outcome. To achieve the above objectives, randomized studies are needed to determine the risk criteria for each individual patient. In our opinion, this is a very promising area in terms of developing an optimal algorithm for the treatment of patients with liver abscesses.
5. Findings
- 1. Ultrasonic drainage is an effective treatment for liver abscesses of various etiologies and in the vast majority of cases avoids open surgery. It should be noted that drainage tactics and intracavity therapy of abscesses depend on the localization of the abscess, the nature of the contents, the connection of the cavity with bile ducts, as well as the presence of bile or portal hypertension.2. The use of minimally invasive methods in the treatment of liver abscesses in combination with long-term intraarterial catheter therapy is highly effective and in the future requires more detailed treatment of this method.3. Complex treatment of liver abscesses using minimally invasive technologies allows for achieving better results at a lower cost, reducing the number of postoperative complications, reducing the time of patients in inpatient, and being allocated more favorable courses of rehabilitation of patients.
Consent
- It is not applicable.
Ethical Approval
- It is not applicable.
Competing Interests
- The authors have declared that no competing interests exist.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML