-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(4): 502-506
doi:10.5923/j.ajmms.20231304.32
Received: Apr. 4, 2023; Accepted: Apr. 19, 2023; Published: Apr. 26, 2023

Evaluation of the Effectiveness of Microsurgical Varicocelectomy in 2871 Patients with Male Infertility
Yuldashev J. M.1, Giyasov Sh. I.1, 2, Mukhtarov Sh. T.1, 2, Kurbanov B. B.2
1“Republican Specialized Scientific and Practical Medical Centre of Urology” (RSSPMCU)
2Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Correspondence to: Yuldashev J. M., “Republican Specialized Scientific and Practical Medical Centre of Urology” (RSSPMCU).
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

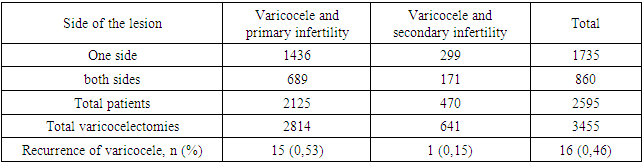
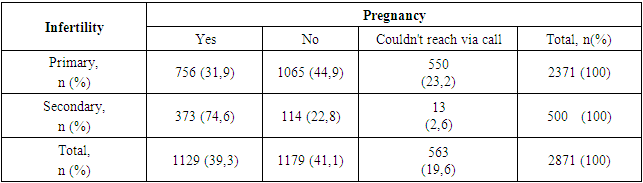
Background. Varicocele is a widespread pathology among adolescents and adult men, which can be accompanied by subfertility, impaired testicular growth and development, hypogonadism and often requires surgical treatment. Purpose of the study. Retrospective analysis of the results of transinguinal microsurgical varicocelectomy in patients with primary and secondary infertility. Material and methods. In the period from November 2005 to January 2022, 2871 patients with a diagnosis of varicocele and infertility were examined and treated at Republic Medical Center of Urology, where patients underwent microsurgical varicocelectomy with a transinguinal approach under spinal anesthesia. The mean age of the patients was 30.16 ± 0.09 (years) (min. 18, max. 60 years). The mathematical analysis of the obtained data was carried out on a personal computer using the Microsoft Excel program, 2019. The Student and Fisher criteria were used. Differences were considered statistically significant at p <0.05. Results. Of the 2871 patients, 2595 (90.4%) were operated on for the first time, of which 1735 patients underwent transinguinal unilateral microsurgical varicocelectomy, in 860 patients on bilateral. As a result, 3455 varicocelectomies were performed for the first time in 2595 patients. The remaining 276 (9.6%) patients underwent microsurgical varicocelectomy, also through inguinal access, for recurrence of the disease, which had previously been operated on in other clinics. At the same time, of these, 105 (3.7%) patients were with primary infertility, 6 (0.2%) - secondary. Conclusions. In patients with infertility and varicocele, the onset of spontaneous pregnancy after transinguinal microsurgical varicocelectomy was 1129 (39.3%), the recurrence rate in primary patients was 0.46% and there was no recurrence after reoperations.
Keywords: Varicocele, Infertility, Surgical treatment, Recurrence
Cite this paper: Yuldashev J. M., Giyasov Sh. I., Mukhtarov Sh. T., Kurbanov B. B., Evaluation of the Effectiveness of Microsurgical Varicocelectomy in 2871 Patients with Male Infertility, American Journal of Medicine and Medical Sciences, Vol. 13 No. 4, 2023, pp. 502-506. doi: 10.5923/j.ajmms.20231304.32.
1. Introduction
- Varicocele is a common pathology among adolescents and adult men, which may be accompanied by subfertility, impaired testicular growth and development, hypogonadism, and possible clinical manifestation as pain and discomfort in the testicular region of the lesion.Varicocele is determined in 15% of adult men, 25% of patients with pathospermia and 35-40% of patients with infertility [1,2,3,4]. According to the literature data, the prevalence of varicocele in men with primary infertility is 35-44%, with secondary infertility – 45-81% [1,4]. It is believed that increased scrotal temperature, hypoxia and reflux of toxic metabolites can lead to testicular dysfunction and infertility as a result of increased oxidative stress and DNA damage [4]. It should be noted that the exact relationship between a decrease in male fertility and varicocele has not been proven. But, according to the data of numerous studies, the improvement of ejaculate parameters after surgical varicocelectomy in patients with pathospermia has been proved [23], and also after varicocelectomy the restoration of sperm DNA damage and reduction of oxidative stress are possible [4,23].However, surgical treatment is not always effective in treating varicocele. According to RCT data, varicocelectomy does not increase pregnancy rates in the subclinical form [24]. In addition, among men with normal ejaculate parameters, there were no advantages of surgical treatment of varicocele compared with dynamic observation. That is why, for several decades, the issues of surgical treatment of varicocele have remained a subject of discussion, as well as the degree of effectiveness of existing various methods of intervention. The purpose of our study was a retrospective analysis of the results of transinguinal microsurgical varicocelectomy in patients with primary and secondary infertility.
2. Material and Methods
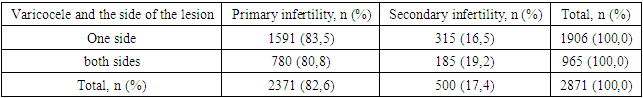
- In the period from November 2005 to January 2022, 9292 patients diagnosed with infertility were examined and treated at RSSPM Center of Urology, of which 2871 (31.0%) patients were found to be associated with the presence of varicocele of varying degrees, for which patients underwent microsurgical varicocelectomy with transpinguinal access.The average age of patients diagnosed with varicocele and infertility was 30.16 ± 0.09 (years) (min.18, max.60 years). The age of patients with primary infertility and varicocele was - 29.36 ± 0.09 (years) (18-54), secondary infertility and varicocele - 33.96 ± 0.25 (years) (23-60), table 1.
|
|
3. Results
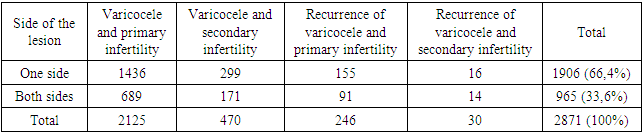
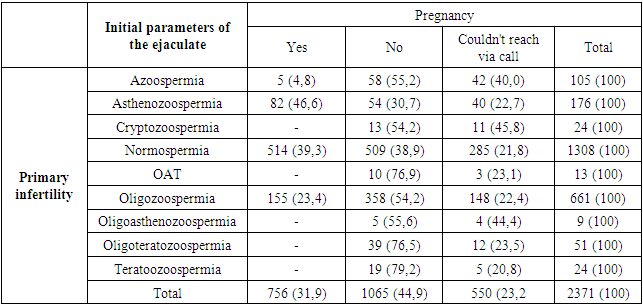
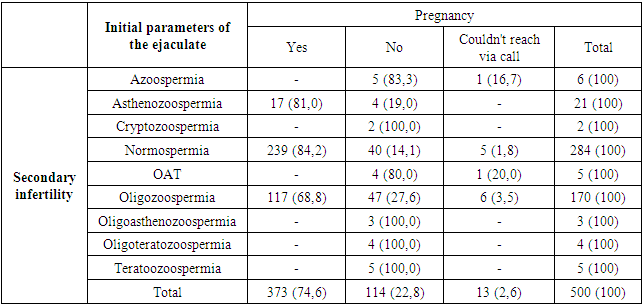
- Our analysis of 2871 patients with primary and secondary infertility, depending on the presence of a newly diagnosed varicocele or recurrence of the disease, taking into account the side of the lesion, showed the following picture, Table 3.
|
|
|
|
|
4. Discussion
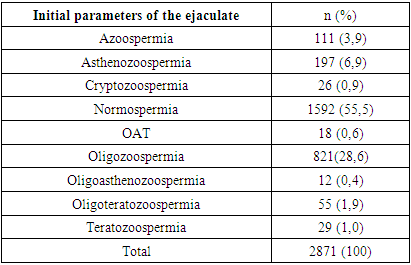
- According to the literature, varicocele is determined in 35–40% of patients with infertility [1,2,3,4]. Among our 9292 patients who came to our Urology Center and were diagnosed with infertility, 2871 (31.0%) had varicocele. According to the literature, where the examination and treatment of 224 patients was carried out, unilateral varicocele was detected in 46.4%, bilateral - in 53.5%, while varicocele of the I degree was determined - in 28.1%, II degree - 44.2%, III degree - in 27.7% [5]. Among our 2871 patients, varicocele on one side was in 66.4%, on 2 sides in 33.6%, while varicocele of I degree was found in 11.4%, II - in 80.6%, III - in 8.0% of patients.Historically, there are various options for surgical treatment of varicocele. According to the literature, the most effective is microsurgical access [6,7], after which the incidence of complications and relapses is lower than after other methods [8]. For example, according to the literature, after microsurgical inguinal or subinguinal varicocelectomy, the recurrence rate of the disease is the lowest and is 0.4%, hydrocele 0.44% [8,9,10,11]. We confirmed the data of the literature and the indicated indicator among our patients was 16 (0.46%) cases of relapse out of 3455 primary microsurgical transinguinal interventions (Table 4). Complications in the form of hydrocele, which caused discomfort in patients, were not registered by us. According to the literature, the average time to improve ejaculate parameters after surgical treatment of varicocele is about 6 months [12,13], while spontaneous pregnancy occurs on average 6–12 months after varicocelectomy [14,15]. According to the literature, the highest incidence of spontaneous pregnancy was after performing microsurgical subinguinal varicocelectomy in 41.97% of all cases (Watanabe et al., 2005). In 37.69% of cases, spontaneous pregnancy occurred after performing surgical treatment of varicocele according to the Palomo method (Cayan et al., 2000), in 30.07% - after performing laparoscopic varicocelectomy (Watanabe et al., 2005), in 33.2% - with selective embolization of spermatic veins (Yavetz et al., 1992) and in 36% of all cases after Ivanissevich's operation. At the same time, it is worth noting that statistically significant differences were identified between the techniques used for the surgical treatment of varicocele (p = 0.001) [16,17,18,19]. Our study showed that among patients after transinguinal microsurgical varicocelectomy performed at the Center for Urology, at a period of 5 to 15 months, 1129 (39.3%) couples had a spontaneous pregnancy. In the literature, there are somewhat contradictory data on the need to perform varicocelectomy in patients with normal ejaculate parameters in patients with infertility. Since in RCTs that included men with normal ejaculate parameters, there were no advantages of surgical treatment of varicocele compared with observation. But, in a 2013 Cochrane Review and other comparative studies, the authors concluded that there was an increase in pregnancy rates after varicocelectomy in men with unexplained infertility [20,21]. Among our patients with infertility, in 1592 (55.5%), i.e. in the vast majority, the normal parameters of the ejaculate were determined, while 1308 (45.6%) suffered from primary infertility, 284 (9.9%) - secondary. Analysis of spontaneous pregnancies among patients with normal sperm counts showed that 47.3% had spontaneous pregnancies after surgery, 34.5% had no spontaneous pregnancies and 18.2% of patients were unreported. Also, in 2019, interesting and promising data on future studies appeared in the literature regarding patients with azoospermia and varicocele. It has been reported that after microsurgical varicocelectomy, men with non-obstructive azoospermia (NOA) have been reported to have spermatozoa, which increased the likelihood of a natural pregnancy or using assisted reproductive technologies (ART) [22]. Our analysis showed that among our patients with infertility and varicocele, 111 (3.9%) had NOA (Table 2). At the same time, of these, 105 (3.7%) patients were with primary infertility, 6 (0.2%) - secondary. However, according to the indications, they performed varicocelectomies. According to long-term results, it was possible to find out that of all patients with NOA, 5 (4.8%) with primary infertility became pregnant with ART.
5. Conclusions
- Transinguinal microsurgical varicocelectomy is an effective and safe operation with a recurrence rate of 0.46%.In patients with infertility and varicocele, the onset of spontaneous pregnancy after transinguinal microsurgical varicocelectomy was 1129 (39.3%).Men with an established diagnosis of varicocele and infertility, but with normal ejaculate indicators, it is advisable to perform varicocelectomy, since in this contingent the frequency of spontaneous pregnancy was 47.3%.Men diagnosed with infertility and non-obstructive azoospermia in the presence of varicocele are advisable to surgically treat it, since some patients have a chance to have children with ART.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML